BLOOD TRANSFUSION
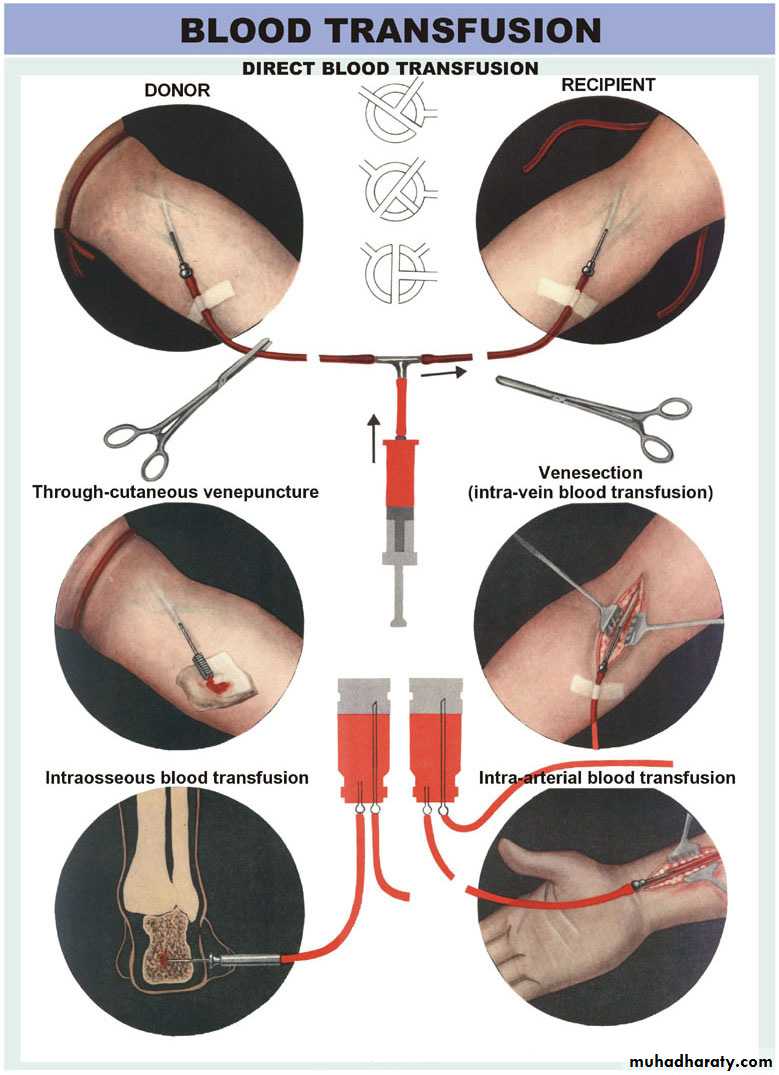
Blood transfusion is generally the process of receiving blood or blood products into one's circulation intravenously. Transfusions are used for various medical conditions to replace lost components of the blood. Early transfusions used whole blood, but modern medical practice commonly uses only components of the blood, such as red blood cells, white blood cells, plasma, clotting factors, and platelets.History of Transfusions
Blood transfused in humans since mid-1600’s1828 – First successful transfusion
1900 – Landsteiner described ABO groups
1916 – First use of blood storage
1939 – Levine described the Rh factor
INDICATION OF BLOOD TRANSFUSION
1- To replace blood lost during surgery or loss of blood due to bleeding in case of injury or any disease cause bleeding such as bleeding DU.To restore oxygen carrying capacity of blood
To provide plasma factor to prevent or treat bleeding
If patient cannot make blood in blood disease
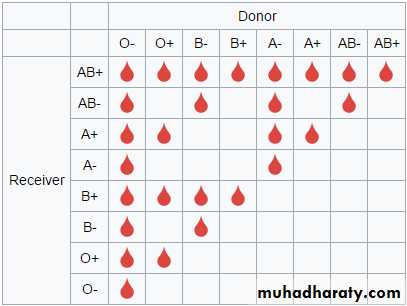
All donated blood should also be tested for the ABO blood group system and Rh blood group system to ensure that the patient is receiving compatible blood.
Before a recipient receives a transfusion,
• The first step before a transfusion is given is to type and screen the recipient's blood.• compatibility testing between donor and recipient blood must be done..
• The sample is then screened for any alloantibodies that may react with donor blood.
It takes about 45 minutes to complete (depending on the method used).
• the history of the patient to see if they have previously identified antibodies and any other serological anomalies.
- The blood bank scientist also checks for special requirements of the patient (e.g. need for washed, irradiated or CMV negative blood)
Donar must be free of the disease and especially HIV, Hepatitis B, Hepatitis C, Treponema pallidum (syphilis) and, where relevant, other infections that pose a risk to the safety of the blood supply, such as Trypanosoma cruzi (Chagas disease) and Plasmodium species (malaria
Component of blood
Denoting blood is usually subjected to processing after it is collected to make it possible to use in specific patient.Collected blood is separated in to blood components by centrifugation
1- RBC
2- Plasma ; FFP fresh frozen plasma, Cryoprecipitate
3-platlets
4-albumin protein
5-clotting factor concentrate
6-immunoglobins (antibody)
7- others Anti-D, Growth Factors, Colloid volume expanders
Apheresis may also used to collect blood components
1-Whole Blood
Storage4° for up to 35 days
Use filter as platelets and coagulation factors will not be active after 3-5 days
Donor and recipient must be ABO identical
Indications
Massive Blood Loss/Trauma/Exchange Transfusion
2-RBC Concentrate
Storage4° for up to 42 days, can be frozen
Recipient must not have antibodies to donor RBC’s (note: patients can develop antibodies over time)
Usual dose 10 cc/kg (will increase Hg. by 2.5 gm/dl)
Usually transfuse over 2-4 hours (slower for chronic anemia
Indications
i e anemia, hypoxia, shock due to bleeding etc.
RBC TransfusionsPreparations
• Type
• Typing of RBC’s for ABO and Rh are determined for both donor and recipient
• Screen
• Screen RBC’s for atypical antibodies
• Approx 1-2% of patients have antibodies
• Cross match
• Donor cells and recipient serum are mixed and evaluated for agglutination
RBC TransfusionsAdministration
• Dose• Usual dose of 10 cc/kg infused over 2-4 hours
• Maximum dose 15-20 cc/kg can be given to hemodynamically stable patient
• Procedure
• May need Premedication (Tylenol and/or Benadryl) (to ovoid allergy)
• Filter use—routinely leukodepleted
• Monitoring, clinical status
• Do NOT mix with medications
• Complications
• Rapid infusion may result in Pulmonary edema
• Transfusion Reaction
3-Platelets
• Storage• Up to 5 days at 20-24°
• Contain Leukocytes and cytokines
• 1 unit/10 kg of body weight increases Plt count by 50,000
• - Donor and Recipient must be ABO identical
• Indications
• Thrombocytopenia, Plt <15,000
• Bleeding and Plt <50,000
• Invasive procedure and Plt <50,000
Platelet TransfusionsPreparations
• ABO antigens are present on platelets• ABO compatible platelets are ideal
• This is not limiting if Platelets indicated and type specific not available
• Rh antigens are not present on platelets
• Note: a few RBC’s in Platelet unit may sensitize the Rh- patient
Platelet TransfusionsAdministration
• Dose
• May be given as single units or as apheresis units
• Usual dose is approx 4 units/m2—in children using 1-2 apheresis units is ideal
• 1 apheresis unit contains 6-8 Plt units (packs) from a single donor
• Procedure
• Should be administered over 20-40 minutes
• Filter use
• Premedicate if hx of Transfusion Reaction
• Complications—Transfusion Reaction
4 - Plasma and FFP (fresh frozen plasma)
• Contents—Coagulation Factors (1 unit/ml)• Storage
• FFP--12 months at –18 degrees or colder
• Plasma should be recipient RBC ABO compatible
• In children, should also be Rh compatible
• Account for time to thaw
• - Usual dose is 20 cc/kg to raise coagulation factors approx. 20%
• Indications
• Coagulation Factor deficiency, fibrinogen replacement, DIC, liver disease, exchange transfusion, massive transfusion
5-Cryoprecipitate
• Description
• Precipitate formed/collected when FFP is thawed at 4°
• Storage
• After collection, refrozen and stored up to 1 year at -18°
• ABO compatible preferred (but not limiting)
• - Usual dose is 1 unit/5-10 kg of recipient body weight
• Indication
• Fibrinogen deficiency or dysfibrinogenemia
• vonWillebrands Disease
• Factor VIII or XIII deficiency
• DIC (not used alone)
6 - Granulocyte Transfusions
• Prepared at the time for immediate transfusion (no storage available)• Indications – severe neutropenia associated with infection that has failed antibiotic therapy, and recovery of BM is expected
• Donor is given G-CSF (granulocyte- colony stimulating factor)and steroids or Hetastarch (volum expander)
• Complications
• Severe allergic reactions
• Can irradiate granulocytes for GVHD prevention
Transfusion Complications
• Acute Transfusion Reactions (ATR’s)
• Chronic Transfusion Reactions
• Transfusion related infections
Acute Transfusion Reactions
• Hemolytic Reactions (AHTR)• Febrile Reactions (FNHTR)
• Allergic Reactions
• TRALI
• Coagulopathy with Massive transfusions
• Bacteremia
1 - Acute Hemolytic Transfusion Reactions (AHTR)
• Occurs when incompatible RBC’s are transfused into a recipient who has pre-formed antibodies (usually ABO or Rh)• Antibodies activate the complement system, causing intravascular hemolysis
• Symptoms occur within minutes of starting the transfusion
• This hemolytic reaction can occur with as little as 1-2 cc of RBC’s
• Labeling error is most common problem
• 1 in 25,000
• Can be fatal
Symptoms of AHTR
• High fever/chills
• Hypotension
• Back/abdominal pain
• Oliguria
• Dyspnea
• Dark urine
• Pallor
What to do?If an AHTR occurs
STOP TRANSFUSIONABC’s
Maintain IV access and run IVF (NS or LR)
Monitor and maintain BP/pulse
Give diuretic
Obtain blood and urine for transfusion reaction workup
Send remaining blood back to Blood Bank
Labs found with AHTR
HemoglobinemiaHemoglobinuria
Positive (DAT) direct agglutination test
Hyperbilirubinemia
Monitoring in AHTR
Monitor patient clinical status and vital signs
Monitor renal status (BUN, creatinine)
Monitor coagulation status (DIC panel– PT/PTT, fibrinogen, D-dimer/FDP, Plt, Antithrombin-III)
Monitor for signs of hemolysis (LDH, bili, haptoglobin)
2- Febrile Nonhemolytic Transfusion Reactions (FNHTR)
Definition--Rise in patient temperature >1°C (associated with transfusion without other fever precipitating factors)Occurs with approx 1% of PRBC transfusions and approx 20% of Plt transfusions
FNHTR caused by alloantibodies directed against HLA antigens
Need to evaluate for AHTR and infection
1 in 200
What to do?If an FNHTR occurs
STOP TRANSFUSIONUse of Antipyretics—responds to Tylenol
Use of Corticosteroids for severe reactions
Use of Narcotics for shaking chills
Future considerations
May prevent reaction with leukocyte filter
Use single donor platelets
Use fresh platelets
Washed RBC’s or platelets
3 - Allergic Nonhemolytic Transfusion Reactions
Etiology
May be due to plasma proteins or blood preservative/anticoagulant
Best characterized with IgA given to an IgA deficient patients with anti-IgA antibodies
Presents with urticaria and wheezing
Treatment
Mild reactions—Can be continued after Benadryl
Severe reactions—Must STOP transfusion and may require steroids or epinephrine
1 in 1,000
Prevention—Premedication (Antihistamines)
4-Transfusion Related Acute Lung Injury TRALI
Clinical syndrome similar to ARDSOccurs 1-6 hours after receiving plasma-containing blood products
Caused by WBC antibodies present in donor blood that result in pulmonary leukostasis
Treatment is supportive
High mortality
5- Massive Transfusions
Coagulopathy may occur after transfusion of massive amounts of blood (trauma/surgery)Coagulopathy is caused by failure to replace plasma
See electrolyte abnormalities
Due to citrate binding of Calcium
Also due to breakdown of stored RBC’s
6-Bacterial Contamination
More common and more severe with platelet transfusion (platelets are stored at room temperature)
Organisms
Platelets—Gram (+) organisms, ie Staph/Strep
RBC’s—Yersinia, enterobacter
Risk increases as blood products age (use fresh products for immunocompromised)
7-Chronic Transfusion Reactions
AlloimmunizationTransfusion Associated Graft Verses Host Disease (GVHD)
Iron Overload
Transfusion Transmitted Infection
transfusion Associated Infections
Hepatitis CHepatitis B
HIV
CMV
CMV can be diminished by leukoreduction, which is indicated for immunocompromised patients