Year three, Pathology: Blood vessel diseases:
Lecture 3: Aneurysms and Dissection:
February 2018 by Dr. Ehsan.
Aneurysm definition:
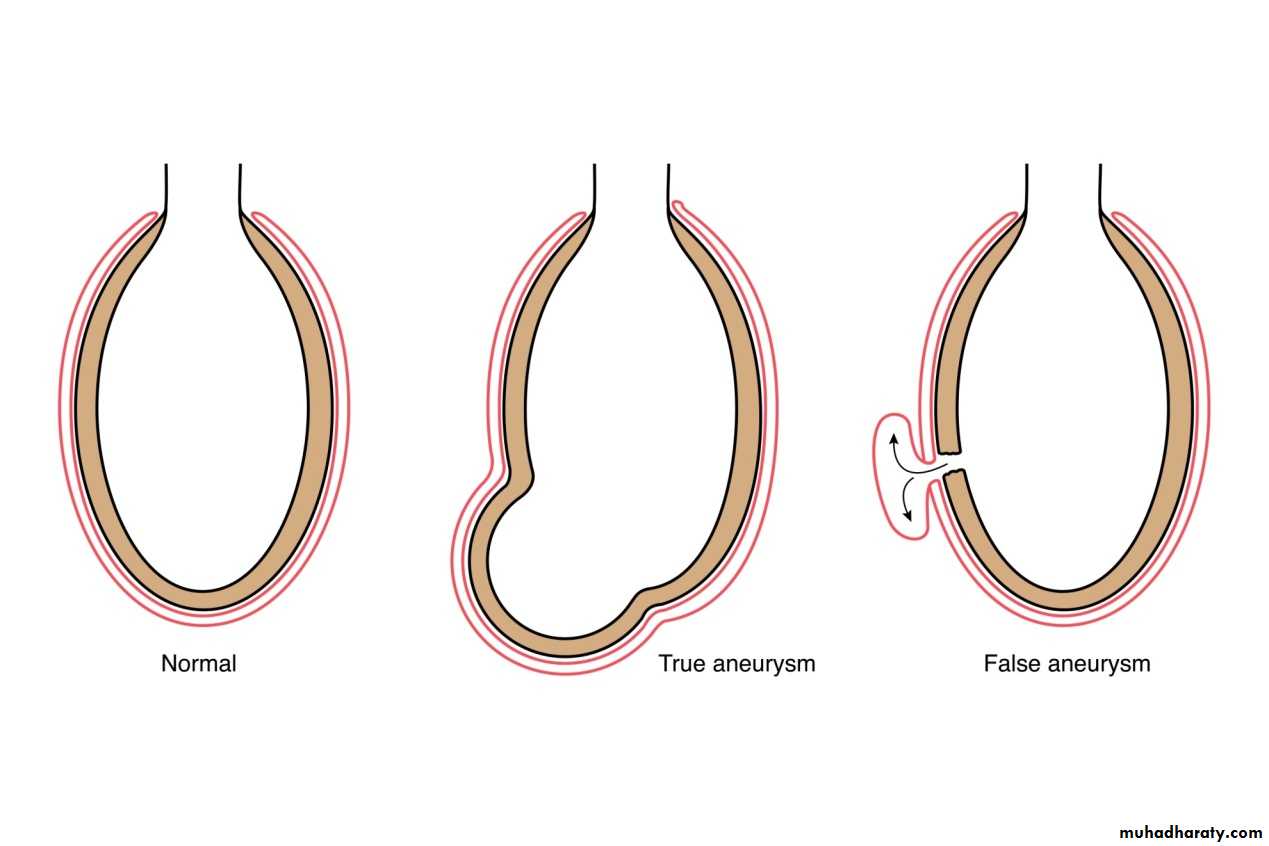
It is a localized abnormal dilation of a blood vessel or the heart, it can be congenital or acquired. When an aneurysm involves an intact attenuated arterial wall or thinned ventricular wall of the heart, it is called a true aneurysm. In contrast, a false aneurysm (also called pseudo-aneurysm) is a defect in the vascular wall leading to an extravascular hematoma that freely communicates with the intravascular space (“pulsating hematoma”).
Atherosclerotic, syphilitic, and congenital vascular aneurysms, and ventricular aneurysms that follow transmural myocardial infarctions are examples of true aneurysms. Examples of false aneurysms include a ventricular rupture after myocardial infarction that is contained by a pericardial adhesion, or a leak at the sutured junction of a vascular graft with a natural artery.
Arterial dissection:
Arises when blood enters the wall of the artery, dissecting between its layers and creating a blood filled cavity (hematoma) within the wall. It is often but not always aneurysmal.Both true, false aneurysms and dissection are liable for rupture with catastrophic results.
Pathogenesis of aneurysms:
It occurs in diseases affecting the ability of the arterial wall connective tissue for repair, as synthesizing the ECM constituents.
The two most important disorders that predispose to aortic aneurysms are atherosclerosis and hypertension. But the most important mechanisms are:
The intrinsic quality of the vascular wall connective tissue is poor. In Marfan's syndrome defect in synthesis of fibrillin leads to abnormal activity of the TGF-Beta and progressive weakening of the elastic tissue, so aorta is dilated due to defect in media. Also in defect of synthesis of type III collagen in Ehlers-Danlos syndrome. Also in vitamin C deficiency there is defect in collagen cross linking and aneurysm formation.
The collagen degradation is more than synthesis due to local inflammatory infiltrates and the destructive proteolytic enzymes produced by the inflammatory cells. Occur in atherosclerosis and vasculitis, by effect of macrophages, with genetic liability.
The vascular wall is weakened by loss of smooth muscle cells or by the inappropriate synthesis of noncollagenous or nonelastic ECM. Aneurysms occur if there is intimal atheroma that presses on the inner media causing ischemia, and increase the distance that oxygen and nutrients must diffuse. Also systemic hypertension causes significant narrowing of the vasa vasorum as in aorta and cause ischemia of outer media. Smooth muscle cell loss replaced by scarring and with inadequate production of ECM, so there is formation of amorphous ground substance (glycosaminoglycans) = cystic medial degeneration.
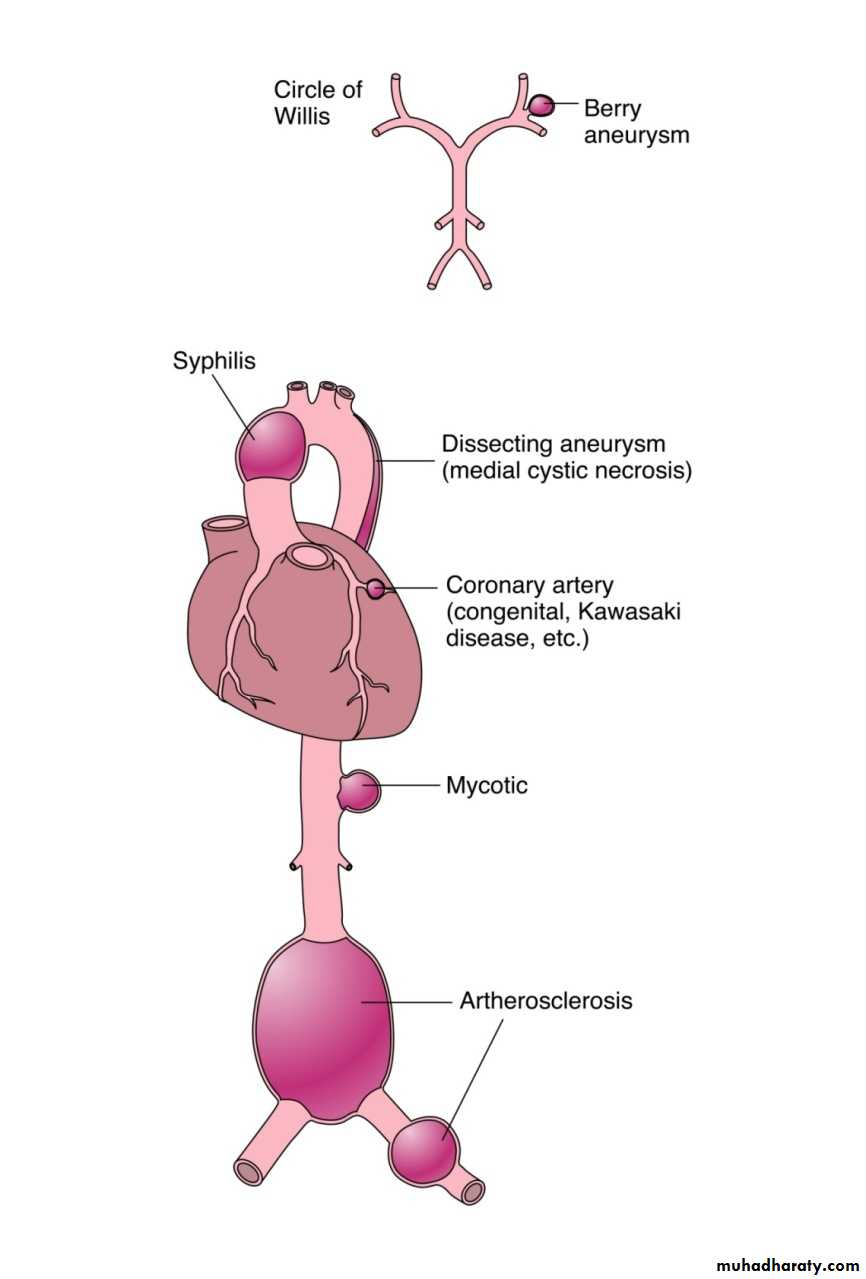
Etiological Classification:
Atherosclerosis.
Cystic medial necrosis or degeneration.
Vasculitis e.g. PAN & Kawasaki dis.
Trauma → arterio-venous aneurysm.
Congenital defects (Berry aneurysm in the brain).
Mycotic aneurysm (infection of arterial wall). (1- from embolization of septic embolus usually in infective endocarditis, 2- extension of adjacent suppurative process, 3- circulating organisms directly infecting the arterial wall).
Syphilis.
Berry aneurysm (saccular A, congenital A)
It is intracranial and responsible for sub arachnoid hemorrhage.
Its incidence is 2% in the general population.
An intact berry aneurysm is a thin walled bright red out-pouching at arterial branch points along the circle of Willis. (anterior circulation mainly).
The etiology and pathogenesis is due to congenital defect of the media especially at bifurcations.
Ruptured berry aneurysm with clinically significant hemorrhage is most frequent in the group 40-50 years.
Abdominal Aortic Aneurysm (AAA):
It is related to atherosclerosis and occurs more frequently in men and smokers, above 50 years. By effect of atherosclerotic plaques and inflammatory cells, that lead to arterial wall thinning by ischemia, and increase the distance that oxygen and nutrients must diffuse, with medial necrosis result in weakness and thinning.
Morphology:
Gross:
Site: below the renal arteries and above the bifurcation of the aorta.
Sometimes accompanied by small aneurysms of iliac arteries
Occasionally can affect the renal, superior and inferior mesenteric aa, by pressure or narrowing or occluding the ostia.
They are usually fusiform, up to 15 cm in diameter and up to 25 cm in length. The intimal surface show severe complicated atherosclerosis, with ulcers covered by mural thrombi associated with medial destruction and thinning.
Microscopy: two AAA variants:
Inflammatory AAA: dense periaortic fibrosis containing abundant lympho-plasmacytic inflammation with many macrophages and often giant cells.
Mycotic AAA aneurysm. Lesions that have been become infected by the lodging of circulating microorganisms in the wall, particularly in bacetremia from a primary salmonella gastroenteritis. In such cases suppuration further destroys the media, potentiating rapid dilation and rupture.
Clinical features: Consequences include:
Rupture: in peritoneal cavity or retroperitoneum with massive fatal hemorrhage.Occlusion: of a vessel by direct pressure or intramural thrombus formation e.g. vertebral branches supplying spinal cord.
Embolism: From the atheroma or mural thrombus.
Pressure on adjacent structures: e.g. obstruction of a ureter or erosion of vertebrae.
Creation of abdominal mass: (often pulsatile), that may be confused with a tumor.
The risk of rupture: Is related to size and rapidity in enlargement. Prosthetic grafts and surgical bypass, should replace large aneurysms (> 5 cm in diameter) to avoid the possibility of rupture.
Thoracic aortic aneurysms:
Most commonly associated with hypertension, other cause is Marfan’s syndrome. Signs and symptoms:
Pressure on mediastinal structures.
Pressure on lungs and airways with respiratory distress.
Difficulty in swallowing, by pressure on esophagus.
Persistent cough due to irritation of laryngeal nerves.
Pain due to bone erosion of ribs and vertebra.
Cardiac disease as aortic valve dilation, insuffeciency and angina by coronary artery ostia narrowing.
Rupture.
Aortic dissection
Dissection occur when blood splays apart the laminar planes of aortic media, with the formation of blood-filled channel within the aortic wall that often ruptures, causing massive hemorrhage. This may be associated with aortic dilation. This dissection of the aorta occurs in two groups of patients:Men aged 40 - 60 years with antecedent hypertension and comprise 90% of the patients with dissection.
Younger patients with systemic or localized abnormality of connective tissue that affects the aorta (e.g. Marfan’s Synd.)
Dissection can also be iatrogenic as in catheterization or cardiopulmonary bypass.
Rarely occur with unknown cause as in pregnancy.
Clinically start as sudden onset of severe anterior chest pain, radiating to the back between scapulae, and move downward.
The risk and nature of complications depend on the region of aorta affected by dissection and rupture has a fatal outcome.
Pathogenesis:
Hypertension is the major risk factor. There is medial hypertrophy of vasa vasorum associated with degenerative changes in the aortic media and variable loss of medial smooth muscle cells, due to mechanical and injury and ischemic injury as a result of diminished flow in vasa vasorum.
Smaller risk factors are connective tissue disorders as Marfan’s syndrome, Ehlers Danlos syndrome, vit C deficiency, and copper metabolic defect.
The trigger for the intimal tear and intramural aortic hemorrhage is not known in most cases.
Morphology:
In most cases, no specific underlying causal pathology is identified in the aortic wall.
The most important finding is cystic medial degeneration; inflammation is characteristically absent.
It is initiated by intimal tear, in the ascending aorta within 10 cm from the aortic valve.
It has a transverse or oblique shape and about 1-5 cm in length, with sharp, jagged edges.
The site is mainly in the ascending aorta or descending or in both.
Dissection can extend:
Retrograde dissection into the aortic root that leads to disruption of the valvular apparatus→ aortic valve insufficiency.
Extend distally; extension of the dissection into great arteries of the neck, coronaries, renal, mesenteric or iliac arteries lead to obstruction with ischemic damage to tissues e.g. M.I. , renal infarction, spinal cord ischemic injury.
Hematoma spreads along the laminar planes of the aorta, usually between the middle and outer thirds.
Rupture through the adventitia, into any of the 3 body cavities i.e. pericardial, pleural or peritoneal (most common cause of death).
Hematoma reenters the lumen of the aorta through a second distal intimal tear, creating a new vascular channel, forming double barreled aorta wit0h a false channel.