Drugs used in infectious diseases
OBJECTIVES:1-Classification of antimicrobial drugs
2-How antimicrobials act3-Principles of optimal antimicrobial therapy
4-Use of antimicrobial drugs: choice, combinations
5-Special problems with antimicrobial drugs
Classification
AntibacterialAntiviral drugs
Antifungal drugs
Antiprotozoal drugs
Antihelminthic drugs
Classification of antimicrobial drugs
Bacteriostatic, i.e those that act primarily by arresting bacterial multiplication, such as sulphonamides, tetracyclines, chloramphenicol.Bacteriocidal, i.e those that act primarily by killing bacteria, such as penicillins, aminoglycosides and rifampicin.
How antimicrobial act-sitesof action
The cell wall: Give the bacteria its charecterstics shape and provide protection against the lower osmotic pressure of the enviroment. Antimicrobial interfere with synthsis of cell wall during multiplication e.g. penicillins, cephalosporine.
The cytoplasmic membrane: Interfere with its structure such as polynes(nystatin).
Protein synthesis: Interfere with the build up of peptide chains on the ribosome of the organism such as tetracycline, chloramphenicole.
Nucleic acid metabolism:
Directly with microbial DNA or its replication or repair, e.g quinolones,metronidazole,or with RNA ,e.g rifampicin.
Indirectly on nucleic acid synthesis, e.g. sulphonamides, trimethoprim.(inhibition of folic acid synthesis).
Principles of antimicrobial therapy
Make a diagnosisRemove barriers to cure,e.g infected I.Vcatheter,drain abscess,remove obstruction in UTI.
Decide whether the drug is really necessary
Select the best drug
Administer the drug in optimum dose, frequency, route.
Continue therapy 5-10 days, chronic infection 9 months
Test for cure
prophylactic chemotherapy
Carriers of pathogenic or resistant organisms
Antibiotic combinations
Avoid the development of drug resistance.T.B.Broaden the spectrum of antibacterial activity, peritonitis.
Obtain potentiation (or’synergy’)penicillin+gentamicin for endocarditis
Enable reduction of the dose of one component and hence reduce the risks of adverse drug reactions.
Problems with antimicrobial drugs
Resistance
Superinfection
Masking of infections
Opportunistic infection
Resistance
Mechanism of resistanceNaturally resistant strains
Spontaneous mutation
Transmission of genes from other organisms
Resistance
Resistance is mediatedProduction of enzymes that modify the drug e.g. aminglycosides are phosphorylated, B-lactamases hydrolyse penicillins.
Decreasing the passage onto or increasing the efflux of drug from the bacterial cell (e.g. imipenem resistance in Pseudomonas aeruginosa)
Target site so that the antimicrobial binds less effectively
Bypassing of inhibited metabolic pathways e.g. resistance to trimethoprim in many bacteria
Superinfection
When any antimicrobial drug is used, there is usually suppression of part of the normal baterial flora of the patient that is susceptible to the drug. Often, this causes no ill effects, but sometimes a drug- resistant organism, freed from competition, proliferates to an extent that allows an infection to be established.e.g candida albicans, (antibiotic-associated)clostridium difficile associated colitisSuperinfection
Opportunistic infection
Arises in patients with compromised immune systems or reduced phagocytic cellular defences, by disease (AIDS, hypogammaglobulinaemia, leukemia) or drugs (cytotoxics, adrenal steroids).
Infections involve organisms that rarely or never cause clinical disease in normal hosts
Masking of infections
Masking of infections by chemotherapy is an important possibilityA course of penicillin adequate to cure gonorrhea, may prevent simultaneously contracted syphilis from showing primary and secondary stages without effecting a cure; a serological test for syphilis should be 3 months after treatment for gonorrhea
Antibacterial drugs
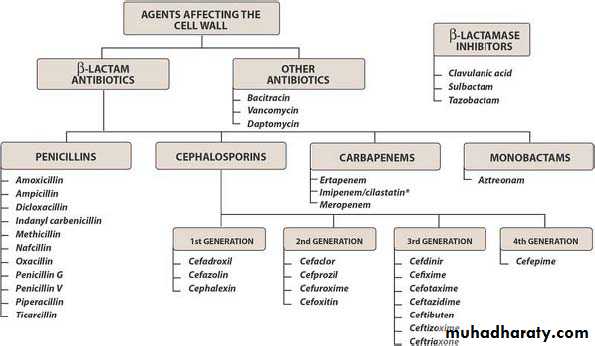
Classification of antibacterialsInhibition of cell wall synthesis
Inhibition of protein synthesis
Interfere with nucleic acid
Inhibition of cell wall synthesis
Β-lactamsPenicillins
Mode of action (bacteriacidal)
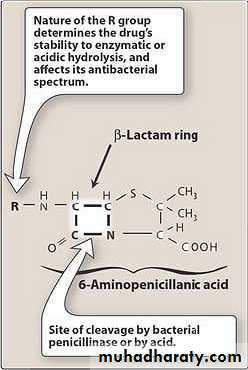
Penicillin act by inhibiting the enzymes (penicillin binding proteins, PBPs) involved in the cross-linking of the peptidoglycan layer of the cell wall. Which protects the bacterium from its environment; incapable of withstanding the osmotic gradient between it’s interior and it’s environment, the cell swells and ruptures.
Bacterial resistant
The main defence of bacteria against penicillins is:to produce enzymes β-lactamases, which open the β-lactam, ring and terminate antmicrobial activity.
Other possible mechanisms include modifications to PBPs to render them unable to bind β-lactams, reduced permeability of the outer cell membrane of Gram-negative bacteria.
Adverse effects
The main hazard with the penicillins is allergic reaction. These include itching, rashes, (eczematous or urticarial), fever, and angio-oedema. Rarely (about 1 in 10000) there is anaphylactic shock,There is 10% partial cross allergy with cephalosporins.
Other such as diarrhoea, neutropenia, anaemia and sometimes haemolytic, and thrombocytopenia or interstitial nephritis.
Also pay attention to the effects of sodium or potassium salts taken with penicillin in case of long use
Calssification of penicillins
Narrow spectrum penicillins.Broad spectrum penicillins.
Extended spectrum penicillins.
Mecillinam.
Monobactam.
Antipseudomonal penicillins.
Narrow-spectrum penicillins
Benzlypenicillin (penicillin G): has short t½(0.5h) so it should given every 6h, it can be given IV or IM(it very painful), benzlypenicillin is effective against G+ bacteria such as streptococcus pneumonia, streptococcus pyogenes.
In case of endocarditis penicillin G is combined with aminoglycoside especially gentamicin
Penicillin G is the drug of choice for infection due to Neisseria meningiditis (meningococcal meningitis), bacillus anthrax, cl. Perfringeus (gas gangrene), cl.tetani (tetanus), corynebacterium diphtheriae (diphtheria), treponema pallidum (syphllis), actinomycosis, drug of choice of borelia burgdorferi (lyme disease in children).
Penicillin G is rapidly eliminated by the kidney and to avoid this we use probencid
Least toxic penicillin and not suitable by orall route since its destroyed by gastric acid
Phenoxy methyl penicillin (penicillin V) is given orally is resistant gastric acid and reach small intestine intact where its moderately well absorbed
All oral penicillin are best given on an empty stomach to avoid the delay in absorption caused by food.
Penicillins distribute mainly in the body water and enter well into the cerebrospinal fluid if the meninges are inflamed.
Antistaphylococcal penicillin
These group of penicillins are resist β-lactamase degradiation by possession of an acyl side-chain in their lactam ring by stearic hindrance limits access of the drug to the enzymes’ active site. However its effect on pneumococcus and β-haemolytic streptococci and Neisseria 20 time less than benzylpenicillin so when there is mixed infection antistaphlycoccus as well as a benzylpenicillin should be given. Flucloxacillin is better absorbed and may cause cholestatic jaundice in elderly patients, cloxacilllin, methicillin, oxacillin are now used to confine the laboratory sensitivity test. Identification of (MRSA) indicate the patient is resistant to flucloxacillin and cloxacillin.broad-spectrum penicillins
These semisynthetics penicillins act against G+ and G- cocci in addition to some of G- bacilli however they do not resist β-lactamases, and their usefulness has reduced markedly because of the increased prevalence of organisms that produce these enzymes. It activity against G+ are less than benzlypenicilli, it have useful activity against Enterococcus faecalis and many strains of Haemophilus influenzaebroad-spectrum penicillins
Ampicillin (t½ 1h)is acid stable and is moderately well absorbed when swallowed. The oral dose is 250mg-1g 6-8hourly; im or iv 500mg 4-6hourlyAmoxicillin(t½ 1h) is a structural analogue of ampicillin. And is better absorbed from the gut, diarrhoea is less frequent with amoxicillin than with ampicillin given every eight hours.
Extend spectrum penicillins
Co-amoxiclav: Clavulanic acid is a β-lactam molecule with little interinsic antibacterial activity, which binds irreversibly to β-lactamases. It competitively protects the penicillin (suicide inhibitor).
Usually used with staph. Aurues many strains of E.coli and H.Infleunza
Others Sulbactam and tazobactam.
Adverse effect: Ampicillin may cause diarrhea.
Patient with renal failure and those taking allopurinol for gout also seem more prone to ampicillin rash which is a maculopapular rash resembling measles or rubella.cholestatic jaundice has been associated with use of co-amoxiclav;the clavulanic acid may be the cause.
mecillinam
Pivmecillinam is an oral agent closely related to the broad-spectrum penicillins but with differing antibacterial activity. It is active against G- organisms including extended spectrum B-lactamase enterobateriaceae but inactive against G+ organisms and against pseudomonas aeruginosa.Monobactam
Aztreonam is the first member of this class of β-lactam antibiotics. It is active against G- organisms including pseudomonas aeruginosa, Haemophilus influenzae and Neisseria meningitidis and gonorrhoeae. Aztreonam is effective in septicaemia and complicated urinary tract infections and gonorrhoea. S.E: rashes, GIT upset, hepatits, thrombocytopenia, neutropenia.Antipseudomonal penicillins
CarboxypenicillinsUreidopenicillins
Carboxypenicillins
These have the same antibacterial activity as ampicillin (destroyed by β-lactamase), but have additional activity against Pseudomonas areuginosa and indole-positive Proteus sppE.g. ticarcillin is presented is combination with clavulanic acid, so to provide greater activity against organisms producing β-lactamase (ticarcillin disoduim salt and each 1g delivers 5.4mmole sodium) this should be noted in patient with cardiac or renal failure.
Ureidopenicillins
Their major advantages over the carboxypenicillins are higher efficacy against Pseudomonas aeruginosa and that as monosodium salts they are safer in respect of sodium over load. they exhibit saturation kinetics.
Piperacillin, Azlocillin,Piperacillin is more active than Azlocillin againstGr-ve and may be in combination with the B-lactam tazobactam.
Piperacillin very effective in burns against pseudomonas.
Cephalosporins
Mechanism of action is the same as penicillins so it bactericidal. Addition of various side chains on the cephalosporin molecule confers variety in pharmacokinetic and antibacterial activities because the B-lactam ring is protected. The result is a range of compounds with improved activity against G- organisms but having less anti-G+ activity, the cephalosporins resist attack by B-lactamases.MRSA should be considered resistant to cephalosporin.
Cephalosporins
Pharmacokinetics: most ceph excreted in the urine unchanged, cephalosporinsin general have a t½ of 1-4h, but with exceptions, e.g. ceftriaxone t½8h. Wide distribution in the body allows treatment of infectin at most sites, including bone, soft tissue, muscle and CSF (in some cases).* In case of renal failure it should be reduced the dose.
Ceftriaxone is excreted through the bile into the feces and is employed in patien with renal insufficiency.
Adverse effects
Allergy (cross allergy with penicillin) 10%Sites of IV or IM may be painful
If continued for more than 2 weeks may cause reversible thrombocytopenia, hemolytic anemia, interstitial nephritis or abnormal liver function tests(reversible)
The third generation of cephalosporin may predispose to opportunist infections (Candida albicans and clostridium dificile ).
Ceftriaxone achieve high conc. In bile and Ca+2 salts may precpitate cause symptoms resembling cholelithiasis.
1st generation
Clinical use
They active against staph infections but the newer cephalosporin is better.
They active against streptococcus pneumonia and Moraxella catarrhalis but have lower activity against Hemophilus influenzea and also active against E.coli.so it can given for treatment of upper and lower RTI, UTI and soft tissue infection.
E.g. cephalexin,cefadroxil orally,
cefazolin I.V.,I.M.
2nd generation
In addition to the uses of 1st gentration they use for community-acquired pneumonia (not when causal organism is Mycoplasma pneumoniam legionella or chamydia)they are more resistant to B-lactamases than the 1st generation drug and active against Staph.aurues,Strep.pyogen,Strept.Pneumonia,Neisseria spp.H.influenza,and many
Enterobacteriaceae.Cefoxitin I.M kill Bacteriods
Fragilis and effective in abdominal and pelvic infection.
E.g cefuroxime orally,cefoxitin,cefprozil
3rd generation
The parenteral such as ceftriaxone, cefotaxime, ceftazidime are used in case of pneumonia, septicemia and meningitis.more effective than 2nd Generation against G-ve whilist retaining activity against G+ve bacteria Cefetriaxone used for gonorrhea and lyme disease.Oral such as cefixime,and cefpodoxime proxetil
Are active against G-ve and G+ve Staph.aureus ,Strept.Pyogen,Strept.Pneumonia,Neisseria,H.influenza and many enterobactereiaceae.and used for upper and lower RTI and UTI.
4 th Generation
Cefepime: used parentrally against staph and strept. And aerobic G-ve E.coli K.pnuemoniae P.aeruginosa
Other B-lactam antibacterials
Carbapenems
The members of this group is widest spectrum of all currently available antibacterial, they active against G- and G+ aerobic and anaerobic pathogenic bacteria. they resist to hydrolysis by most B-lactamases.
e.g. imipenam metabolized by kidney to products that are potentially toxic to renal tubules; combining imipenem with cilastatin (the enzymme responsible for its renal metabolism)
Prevent inactivation and toxication.
Other B-lactam antibacterials (continue)
CarbapenemClinical used intra-abdominal infection, septicamia, nosocomial pneumonia.
Side effect GIT upset including nausea, blood disorders, allergic reaction, confusion and convulsion.
Other carbapenems such as meropenem (not affected by renal dihydropeptidase) and ertapenem not active against pseudomonas erug.
Other inhibitors of cell wall synthesis and membrane function
Vancomycine (8h)Glycopeptide (peptolide)acts on multiplying organisms by inhibiting cell wall formation at a site different from that of the B-lactam antibacterials.
Vancomycine
vancomycine activite against clostridia (including Clostridium difficile),almost all strains of Staphlyococcus aureus (including those that produce B-lactamase and meticillin-resistant strains), and coagulase-negative staphylococci.
Viridans group streptococci and enterococci.
vancomycine
Pharmacokinetics: is poorly absorbed from the gut and the I.V. route is necessary for systemic infections, there being no satisfactory I.M. preparation. It distributes effectively into body tissues and is excreted in urine.
Clinical uses: treatment pseudomembranous colitis that caused by cl.dificile and given with an aminoglycoside for treating streptococcal endocarditis in patients who are allergic to benzylpenicillin.
Vancomycin
Adverse effectsTinnitus and deafness may arise.
Nephrotoxicity and allergic reactions also occur.
Rapid i.v. infusion may cause maculopapular rash possibly due to histamine release( the red person syndrome).
Other inhibitors of cell wall synthesis and membrane function
Other members of this category is:Teicoplanin (is similar to vancomycin) but has long half-life 50hrs and used with serious infection with G+ve endocarditis & peritonitis.
Daptomycin: lipopeptide antibiotic naturally produced by streptomyces roseosporus with activity against virtually all G+ve bacteria.