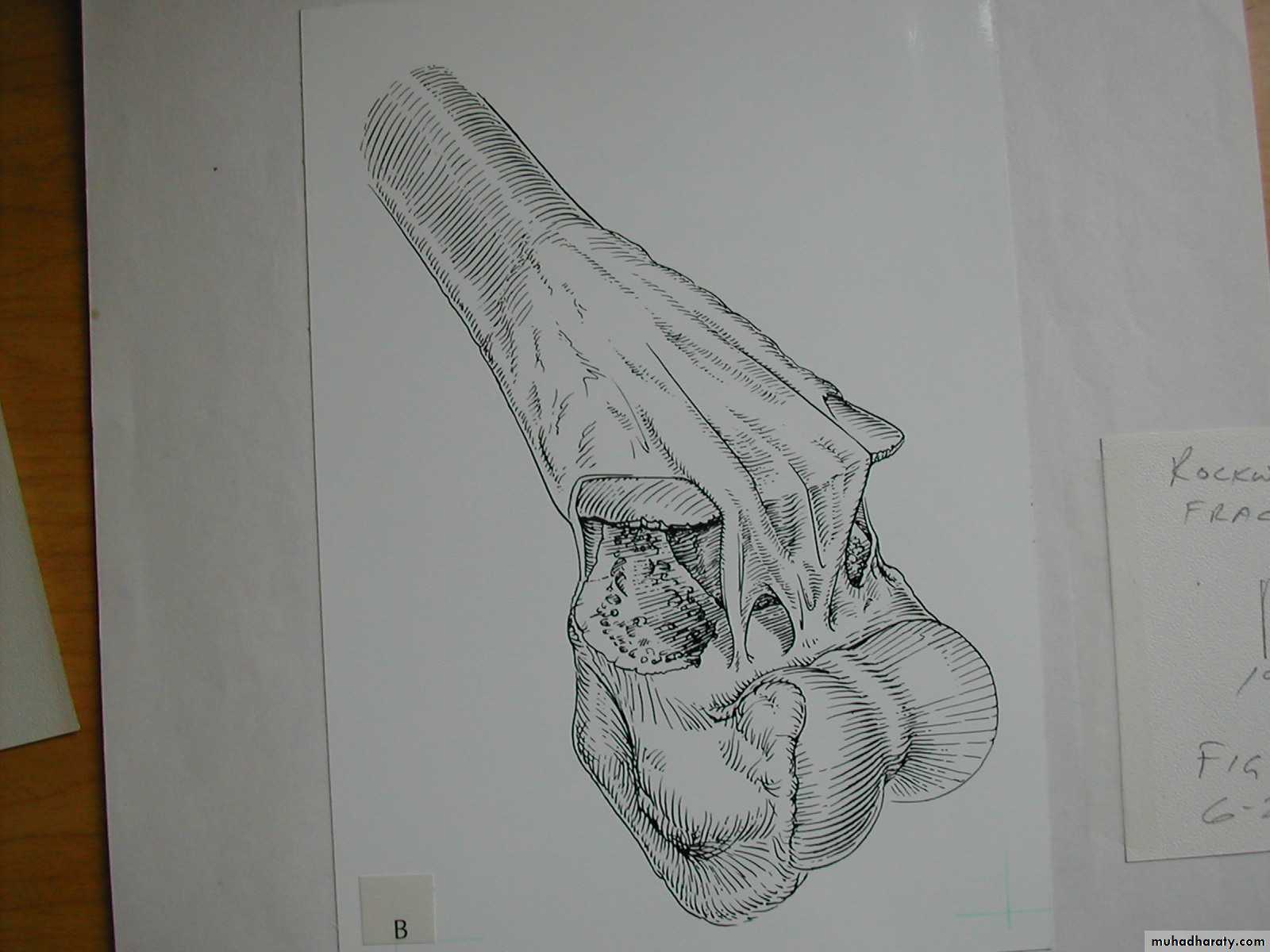
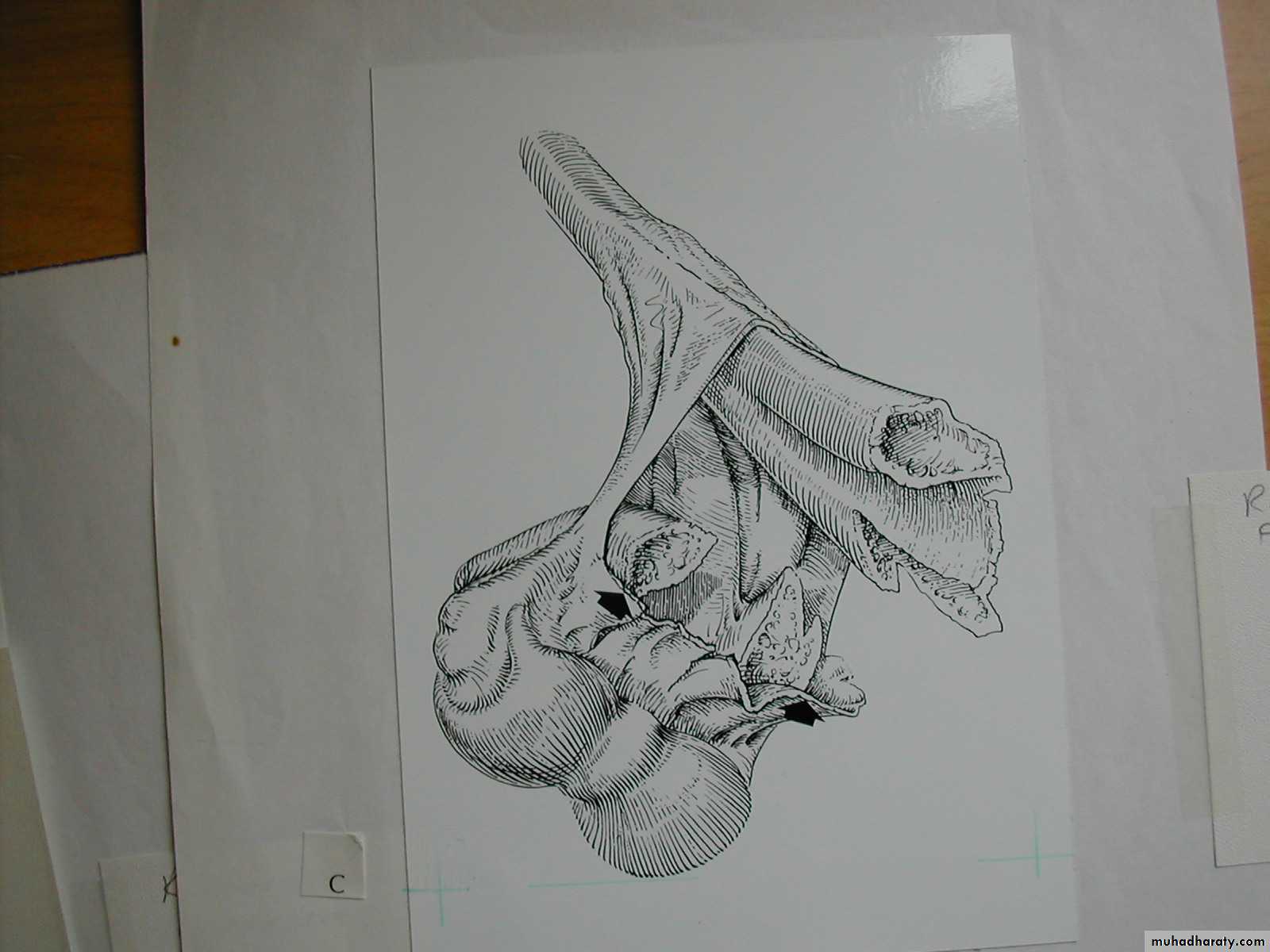
2. The distal fragment is in valgus.
3. The medial spike of the proximal fragment is usually posterior.
Supracondylar Fractures
of the HumerusInter-active
Part I
The incidence peaks at
I. IncidenceAt what age do supracondylar fractures
most commonly occur ?
Why?
3 years
7 years.
10 years
That is the age when children reach
their maximum ligamentous laxity.
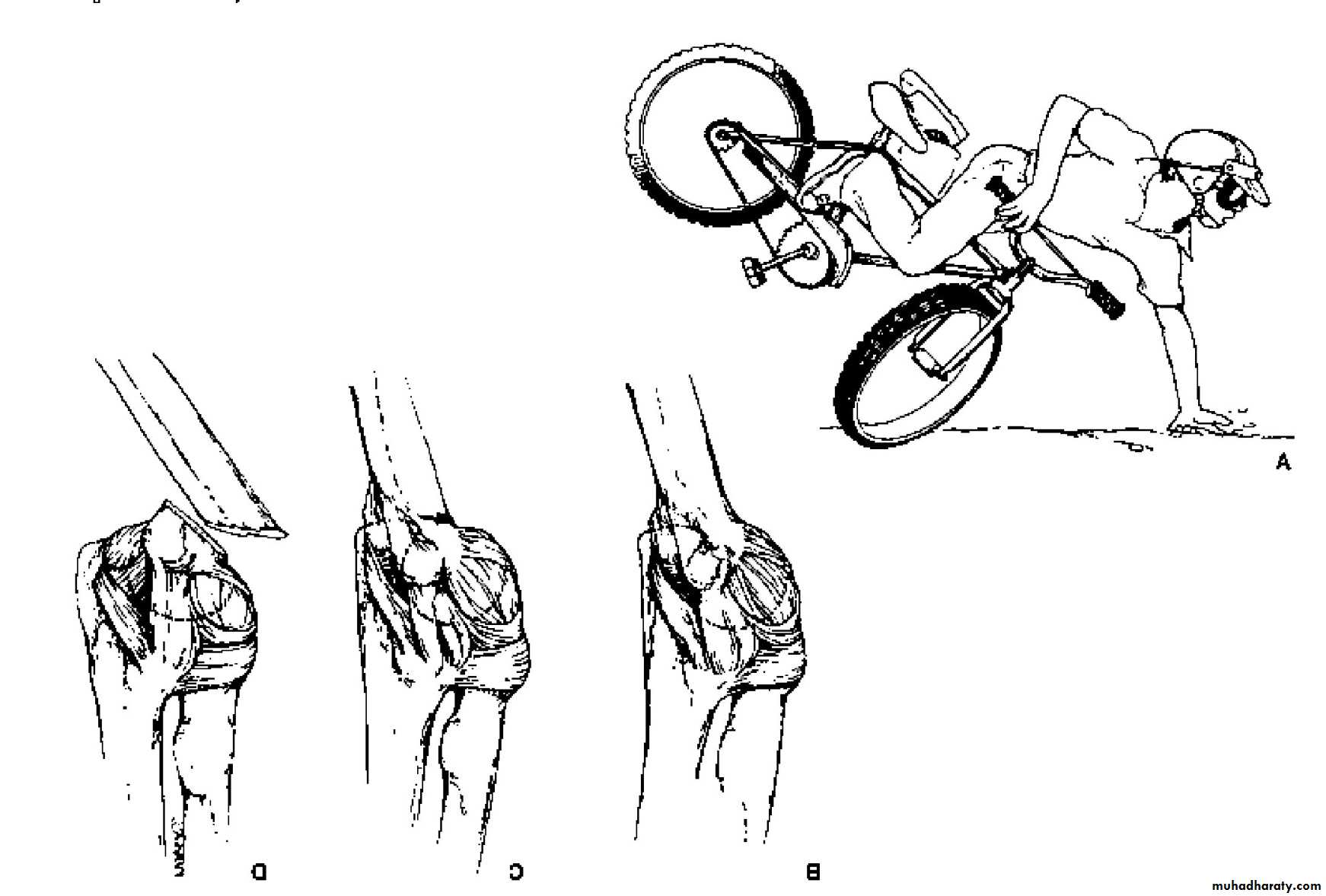
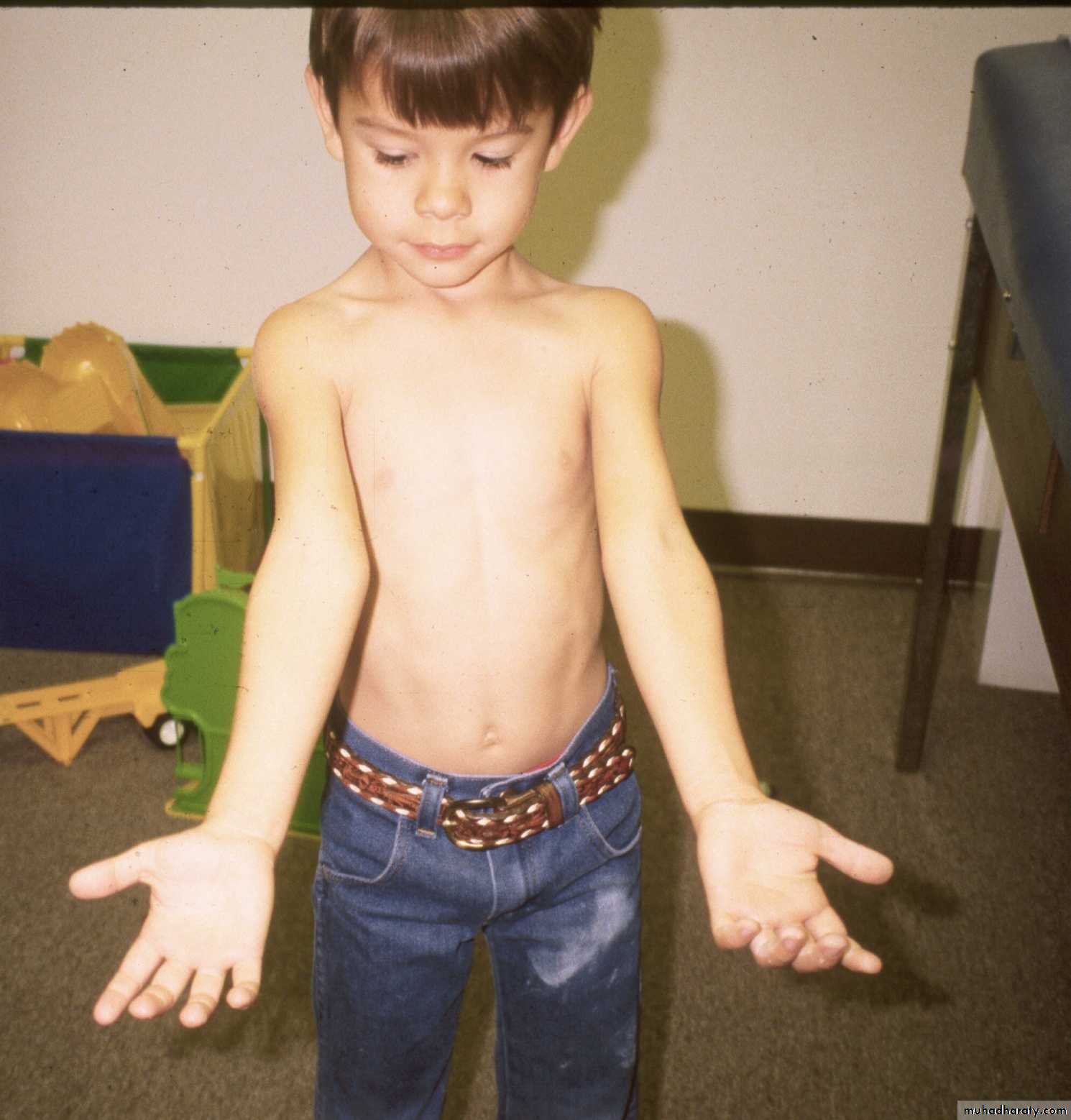
Mechanism of Injury
What other factor contributesto the development of
fractures in the supracondylar area?
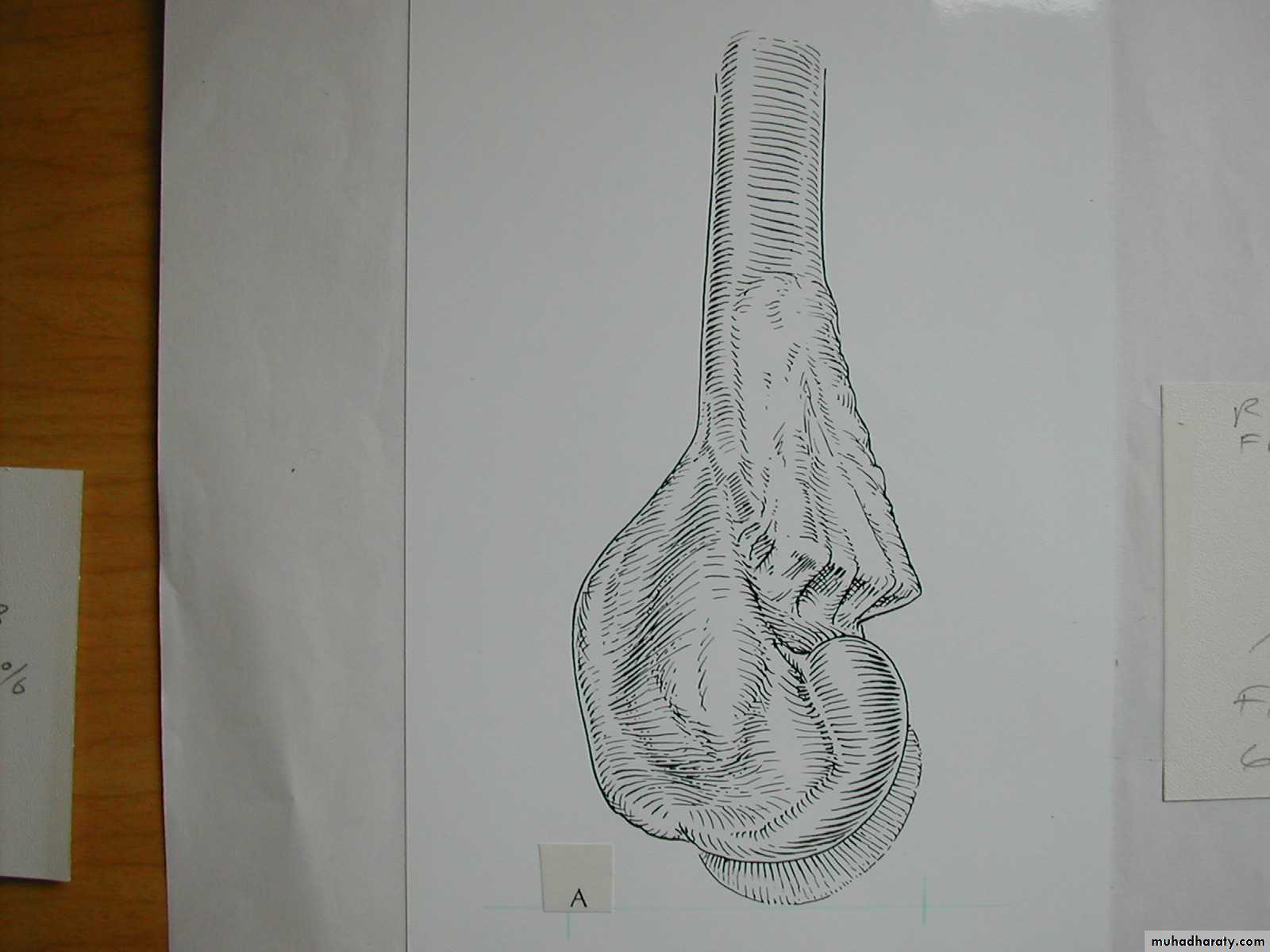
The supracondylar area consists
of weak metaphyseal bone.
Very thin
corticalstructure
II. Mechanism of Injury
What is the mechanism of injury
for extension type supracondylar fractures ?As the
extended extremityattempts to break
the fall,
the olecranon
is forced
deep into its fossa.
This causes
the humerus to failin the weak metaphyseal
supracondylar area.
How are the extension type supracondylar
humeral fractures further classified?*
*Gartland,JJ:.
Surg Gynecol Obstet 109:145,1959.
What does his classification represent ?
How are the extension type supracondylar
humeral fractures further classified?His types represent
no more than the
three stages
of displacement.
What are the
three stages
of displacement?
Type I
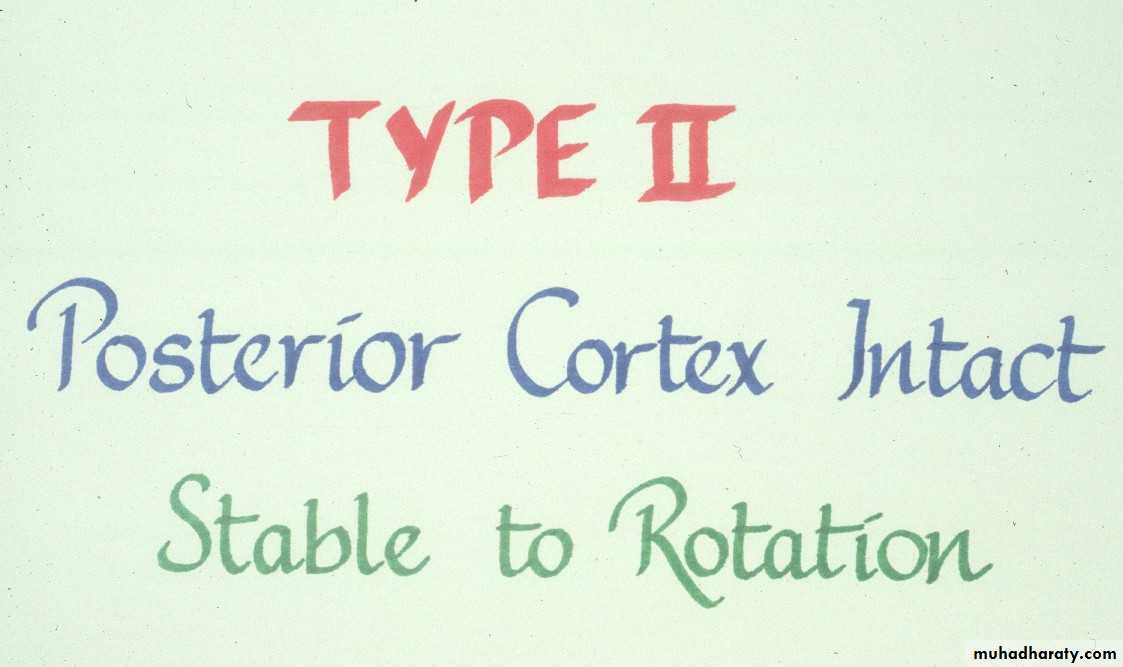
No displacementType II
Incomplete
displacement
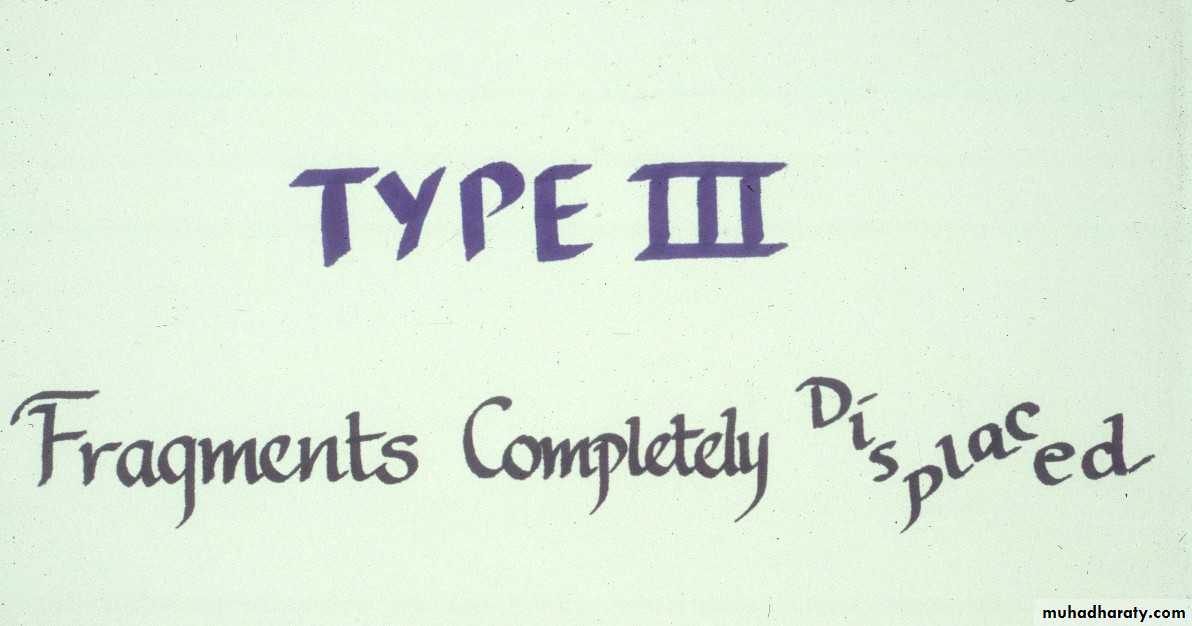
Type III
Complete
displacement
Why all this
emphasison the classification?
It dictates
the
method of
treatment.
*
*Abraham E, Powers T, Witt P, Ray RD
Clin Orthop 171:309, 1982.
Let us examine the treatment
based upon the
Gartland Types.IV. Extension type supracondylar fractures
How are the Type I
fractures usually treated?How must Type II fractures
be managed?Treatment
1. Manipulate to obtain a reduction
then
2. Stabilize the reduction
Treatment
150
What must be accomplished with
the manipulative process?
First
This is usually accomplished
by first forcing the forearminto pronation.
The deformities in both planes
need to be corrected.
Some manipulative correction
may need to be accomplished
in the coronal plane as well.
150
One usually meets resistance,
at the point where the shaft condylar malalignment limits flexion.First
Then
The deformities in both planes
need to be corrected.This usually re-establishes the saggital
alignment (shaft-condylar angle) of the distal fragment.To obtain a complete reduction in the
saggital plane, one must
To obtain a complete reductionin the
saggital plane one must
400
How does one determine
if this fracture can beimmobilized with a cast
alone?
Following this hyper flexion, the elbow is then extended
and examined to be sure the carrying angle
has been corrected as well.
Full
.The reduction has been maintained
at 1200 of flexionand 900 of external rotation.
Determine if it is
400
.
If the reduction is stable
at 1200 of flexion,and there is no evidence
of
vascular compromise,
how can these fractures
be best immobilized
post reduction?
Stabilization with a
may not be adequate !!The elbow must be flexed to 120 0
Injury filmReduced at 1200
Reduction lost
at 900WARNING
Flexing to > 1200 may increase the riskof vascular problems.
*
*Millis MB, Singer IJ, Hall JE.
Clin Orthop 188:90–97,1984.
to maintain the reduction .
Thus these fractures need to be immobilized
with a figure
8cast.
Always incorporate
the sling intothe cast.
Mommy,
this slingis
bothering me!
That’s
muchbetter !
But,
loss of
elbow
flexion
may
result in
a loss of
reduction.
What are the criteria for
fractures?How are Type III extension supracondylar
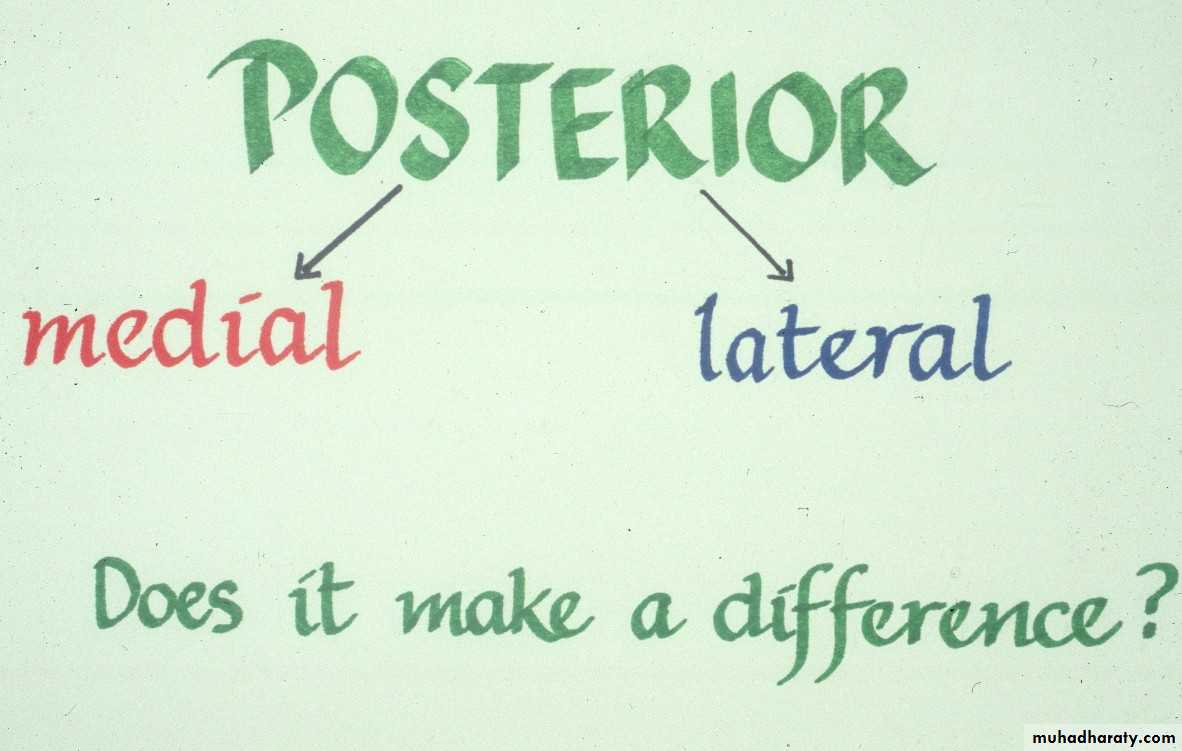
fractures sub-classified?Yes
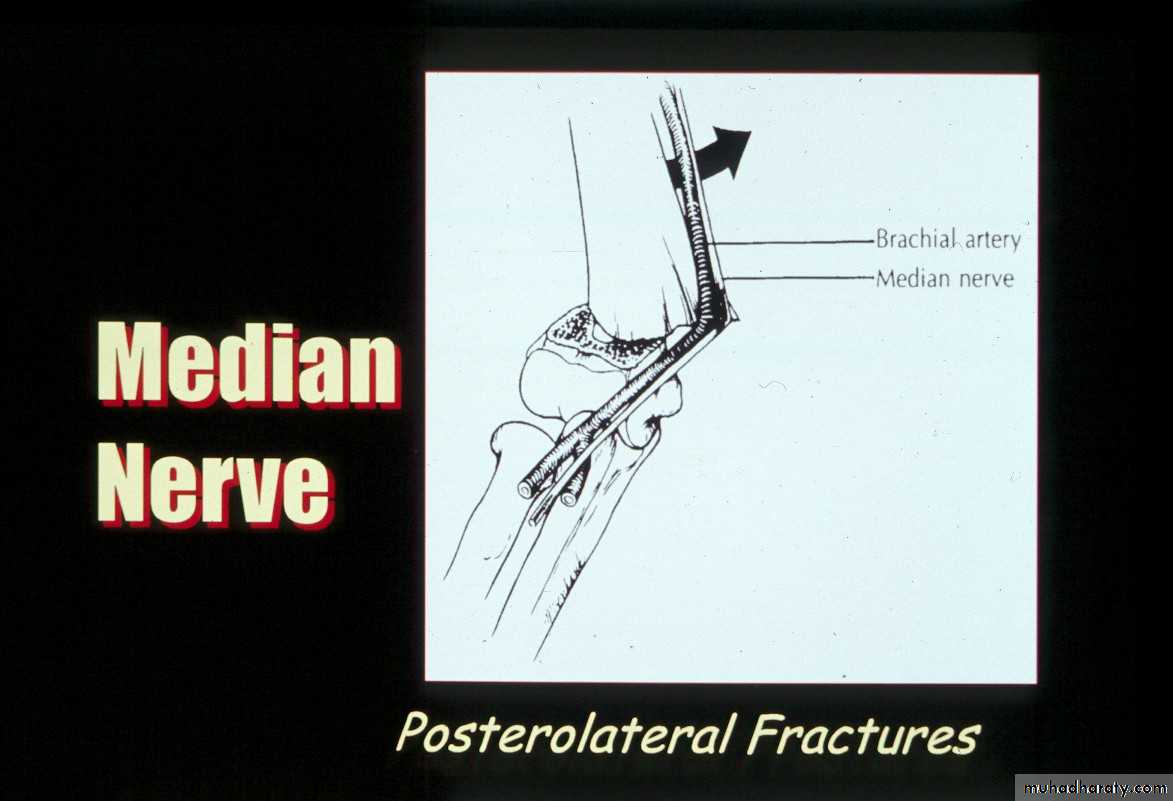
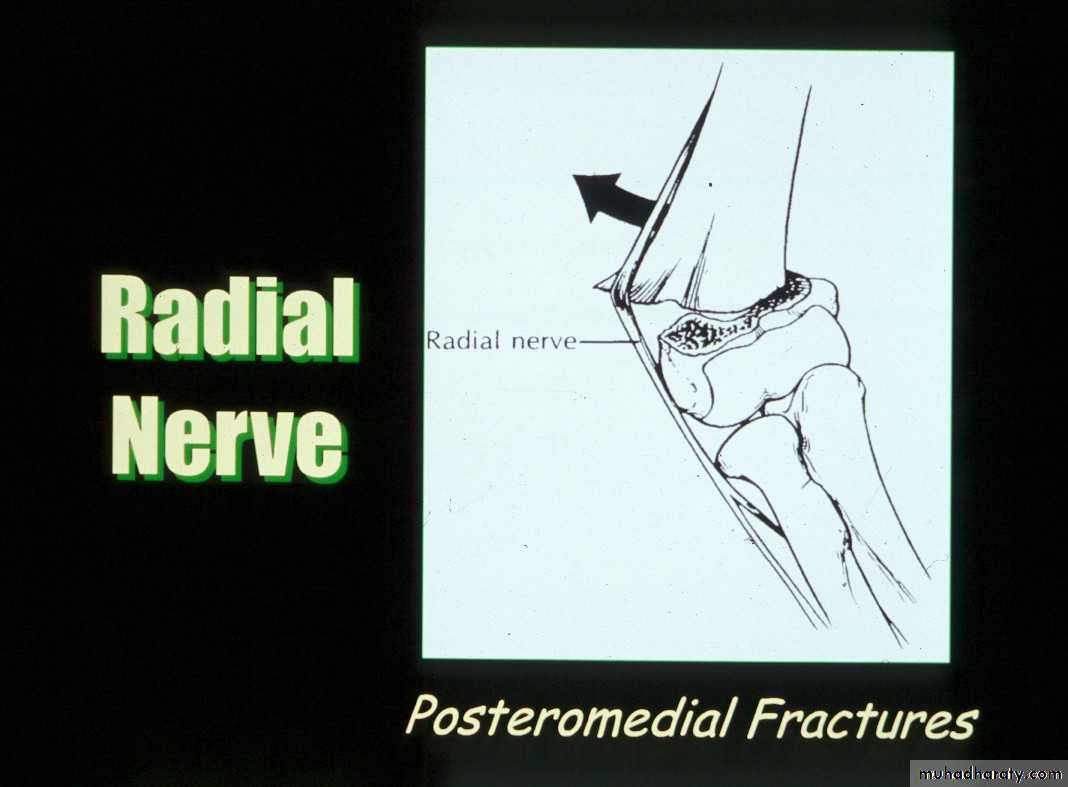
Posteromedial vs. Posterolateral
• Nerve, Vessel Injured
• Surgical Approach
• Rate of Complications
In what aspects is there a difference?
What type has a greater
potential for complications?
The rate of complications is greater with the posterolateral fractures.
What is the major concern
with the posteromedial fractures ?The radial nerve
is more vulnerableto injury.
Treatment
How are Type III fracturesbest treated?
Simple
1. Obtain the reductionthen
2. Maintain the reduction
It consists of four steps:
Reduction of the fractureWhat does the manipulative
process entail ?
With the elbow in extension, align the distal fragment
to the proximal fragment in the coronal plane.1. Correct coronal plane alignment
2. Re-establish Length
TractionCounter-Traction
This usually requiresan assistant.
3.Correct Angulation
andPosterior Displacement
Apply longitudinal traction
with the elbow semi- flexed,while applying posterior
pressure on the proximal fragment.
Then, slowly flex the elbow to bring
the distal fragment into alignment.4. Temporary stabilization and assessment
to lock the distalfragment to the
proximal fragment.
Once the fragments are reduced,
hyper-flex the elbow
withhyper-pronation
Then, confirm the reduction
in full external rotationon the monitor.
Warning!!
If unable to obtainfull flexion
STOP!!
There may be
interposed tissue
between the fragments!!
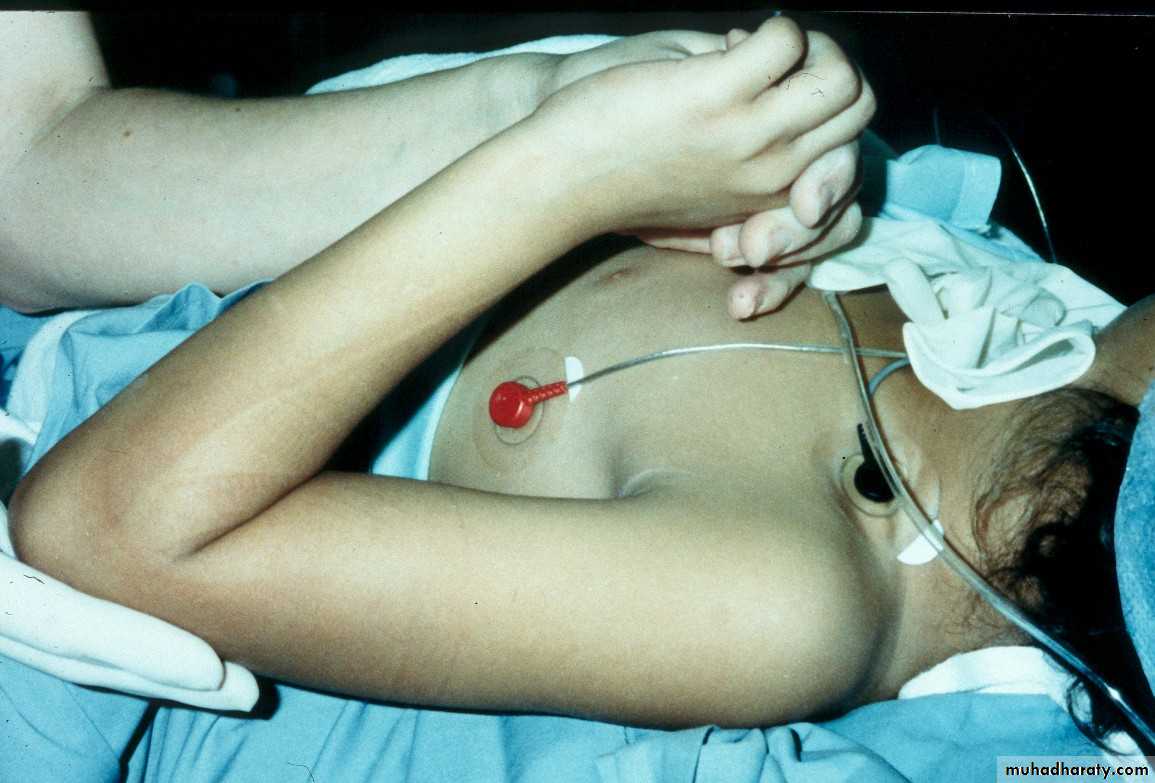
Percutaneous
pin
fixation
If a cast is inadequate,
then what is the standard for maintaining the reduction?
• Advantages ?
• Most stable construct• Post-operative, one is able to fully extend elbow to visualize coronal alignment
• Disadvantages ?
• Ulnar nerve injury
Medial-lateral
pins
In what manner may the pins be used?
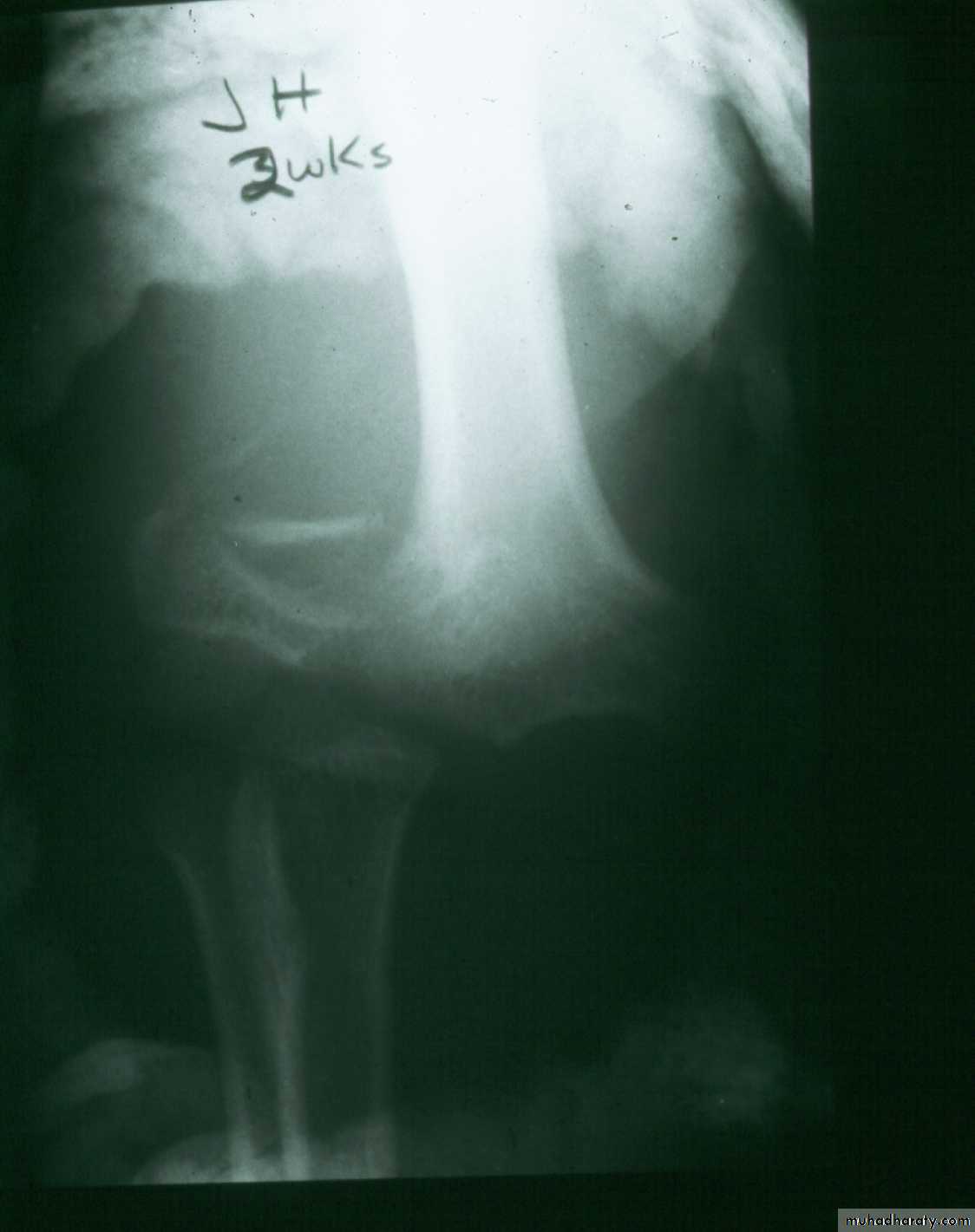
What about late-appearing fractures ?
2 wks. post
closed reductionWhat now?
Repeat
closed reduction?
Open reduction?