Classification of diseases and conditions affecting the periodontium
DR.HUSSEIN AL DABBAGH
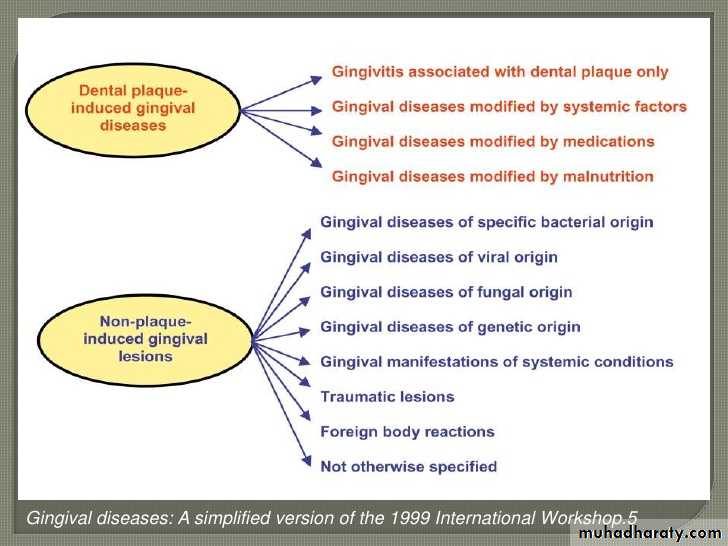
Classification of gingival disease
A-Dental Plaque-induced Gingival DiseasesThis group of gingival diseases is caused by plaque (biofilm)
1-Gingivitis Associated with Dental Plaque Only
Gingivitis – can be best described as a bacterial infection of the gingival tissue caused by plaque (biofilm) at the gingival margin. Dental plaque-induced gingival diseases are characterized as gingivitis associated with dental plaque only with or without other local contributing factors. Local contributing factors may include:
Crowded or malpositioned teeth
Dental restorations
Orthodontic appliances
These factors do not cause gingivitis but act as plaque/biofilm traps that make oral hygiene techniques more difficult and less effective.
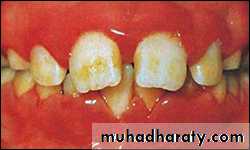
Gingivitis presents as:
Redness of the marginal gingiva
Gingival bleeding
Edema or enlarged gingiva
Gingival sensitivity and tenderness
No clinical attachment loss
Reversible to health once the causative plaque (biofilm) is removed
2-Gingival Diseases Modified by Systemic Factors
Plaque/biofilm is responsible for the initiation of the disease process and systemic factors modify the host’s immune system response. These systemic factors do not cause gingivitis but may act to intensify it.Changes in hormone levels allow for an exaggerated response to plaque/biofilm. Hormonal-influenced gingivitis (puberty-, menstrual cycle- and pregnancy-associated gingivitis and pyogenic granuloma) and poorly controlled blood glucose levels (diabetes mellitus-associated gingivitis) may increase the inflammatory response of the gingiva to plaque/biofilm.
Pregnancy Gingivitis
3-Gingival Diseases Modified by MedicationsDrug Influenced Gingival Diseases
Commonly used drugs can lead to gingival changes including hyperplasia (overgrowth) and gingivitis. There are no specific bacteria or risk factors other than poor plaque/biofilm control associated with these gingival diseases.
Drug Influenced Gingival Enlargement
Medications taken for certain conditions can cause gingival hyperplasia. Those medications include:
Phenytoin – used to control convulsive disorders
Cyclosporine – used for immunosuppressive therapy in organ transplant patients
Calcium channel blockers such as nifedipine, amlodipine and diltiazam – used for cardiovascular conditions such as hypertension, angina and arrhythmias.Oral Contraceptive Associated Gingivitis
The use of oral contraceptives causes gingival inflammation similar to that seen in pregnancy.
Drug influenced gingival enlargement
4-Gingival Diseases Associated with Blood DyscrasiasBlood dyscrasias are an abnormal function or number of blood cells. There are a number of blood dyscrasias that present problems for the patient.
Leukemia-associated gingivitis. leukemia-associated gingivitis, there is an abnormal increase in leukocytes (white blood cells) in the blood and bone marrow. Patients with leukemia may exhibit gingival bleeding and enlargement that starts in the interdental papilla and spreads to the attached gingiva.
Gingivitis associated with leukemia
4-Gingival Diseases Modified by MalnutritionAscorbic Acid Deficiency GingivitisVitamin deficiencies may produce changes in the oral cavity. The most studied relationship is ascorbic acid or Vitamin C. Deficiency of this vitamin is called scurvy and results in defective collagen formation and maintenance. This type of gingivitis can rapidly progress to periodontal disease.
Gingivitis as a result of Vitamin C deficiency
Non-plaque-induced Gingival Lesions
Gingival Diseases of Specific Bacterial Origin
These gingival diseases are caused by a specific bacterium this is not usually associated with plaque/biofilm. These atypical periodontal pathogens overwhelm the host’s resistance and cause an infection. Gingival impact includes painful ulcerations, mucous patches or highly inflamed gingiva.1-Neisseria Gonorrhea Associated Lesions
. Diffuse erythema, small erosive pustules and edema may be seen in the oropharyngeal region as well as on the tonsils or uvula. Stomatitis, sore throat and lymphadenopathy may also be present.2- Treponema Pallidum Associated Lesions
This bacterium causes syphilis. In a primary syphilis infection, the lips, gingiva, tongue, tonsils and palate may be affected. While these lesions generally heal without intervention, they may lead to scarring. In secondary syphilis, white mucous patches may be present. In both stages, lesions are contagious. In tertiary syphilis, may cause perforation of the tongue or palate3-Streptococcal Species Associated Lesions
These bacteria cause an upper respiratory infection with a fever. Diffuse gingivitis, tonsillitis, pharyngitis and ulcers of the oral mucosa may be present.
Gingival Diseases of Viral OriginThese gingival diseases may resemble plaque/biofilm – induced gingivitis
1-Herpes Virus Infections
These include primary herpetic gingivostomatitis, recurrent oral herpes and Varicella-zoster infections. While not technically gingival diseases, these infections are important to understand because they are very common, highly contagious and can be transmitted to the dental hygienista- primary herpetic gingivostomatitis (Figure A), the patient may present with an elevated temperature, general malaise and vesicle formation on the gingival or oral mucosa. Many vesicles may coalesce into ulcerative lesions.
b- recurrent oral herpes (Figure B), lesions commonly known as ‘fever blisters’ or ‘cold sores’ appear around the mouth.
c- Varicella-zoster virus (Figure C) is responsible for chickenpox (varicella). The virus becomes latent but can be reactivated as herpes zoster or shingles. In addition to the skin lesions, oral lesions may be present. This is generally a condition found in older adults.
Primary herpetic gingivostomatitis
Recurrent oral herpes
Varicella-Zoster of the tongue.
A
C
B
Gingival Diseases of Fungal OriginThere are several fungi species associated with gingival conditions. The most common of these is Candida albicans
1-Generalized Gingival Candidosis
Candida has been isolated from the gingiva of healthy patients with periodontitis and is more recently associated with patients with immunosuppression such as HIV. The gingival tissue and oral mucosa is erythematous with a removable white coating and appears fragile.
2-Linear Gingival Erythema
This was formerly called HIV-related gingivitis and presents as a red line at the gingival marginGingival Diseases of Genetic OriginSome gingival changes may occur as the result of genetic predisposition
1-Hereditary Gingival Fibromatosis
Gingival enlargement, completely cover the tooth.
Gingival Manifestations of Systemic Conditions
Systemic conditions can be reflected in the gingival and oral conditions. These include mucocutaneous disorders, allergic reactions to dental restorative materials and reactions to oral hygiene products or foods/additives.A- Mucocutaneous Disorders
1- Lichen Planus –the common reticular form and the more rare erosive and bullous forms. In the erosive form, alternating patches of white lesions and raw red areas may be present and tender for the patient. This form may transform to squamous cell carcinoma and so these lesions should be carefully and periodically examined.2-Pemphigoid – Similar to Lichen, it is different in that it is more common in older adults and women. Symptoms include blistering and sloughing of the surface of the gingival epithelium exposing the underlying connective tissue. These areas can be quite painful. Lesions can appear on the buccal mucosa and inner surface of the lips.
3-Pemphigus vulgaris –involves blistering and erosions.
painful blisters occur orally as the first sign of the disease. Severe cases may require hospitalization for wound management similar to burn patients.4-Erythema multiforme – Oral manifestations include swollen lips and gingival lesions that involve bullae that rupture and leave ulcers.
5-Lupus erythematosus – are characterized by a well-defined central red area surrounded by a raised white radiating border.
6- Drug Induced
When a drug, such as aspirin, is placed locally, it can irritate the area ("aspirin burn"). The most common area affected is the gingivaAspirin burn
B- Allergic ReactionsAllergic reactions to dental restorative materials, components of oral hygiene products and foods or additives occur and are most common in patients with a history of allergic conditions such as allergic skin rashes, hay fever or asthma.
1- Dental Restorative Materials
Mercury, nickel and acrylic. Gingival lesions as the result of a contact allergy to various dental materials do occur. Allergies to precious alloys are extremely rare
Acrylic allergy
2- Reactions Attributable To Toothpastes, Mouth Rinses, Chewing Gum Additives and Food Additives
Desquamative gingivitis may occur with the use of tartar control toothpastes or mouth rinses. The pyrophosphates and the flavoring agents used to mask their flavor have been identified as the main causative agents.
contact allergy
Traumatic LesionsThese lesions can occur as a result of an unnatural event (factitious), a dental procedure (iatrogenic) or an unforeseen event (accidental). Factitious lesions tend to be more chronic in nature while iatrogenic and accidental lesions tend to be more acute and self-limiting. Permanent gingival defects may result from trauma and may need periodontal plastic surgery. Oral manifestations include burns, ulcers or areas of recession.
1-Chemical Injury
The improper use of aspirin or peroxide in the mouth can cause oral injury
Phenol burn
2-Physical InjuryMalocclusion, removable partial dentures/retainers, improper flossing; toothbrush trauma; and self-inflicted injuries are common causes of physical injury to the oral tissues.
Floss cut
3- Thermal Injury
The most common cause of thermal injury to the oral region is hot foods/liquids such as pizza, burritos, coffee or soup.
Burn
Foreign Body ReactionsThe presence of a foreign body in or near the oral tissues can cause injuries resembling the burns, ulcers or recessed areas of traumatic lesions. Introducing amalgam during an extraction or abrasive agents during a polishing procedure may cause a local reaction.