GASTROINTESTINAL TRACTlecture 4
The Department of PathologySmall and Large Intestines -1
Congenital anomalies 1- Atresia and stenosis
Congenital intestinal obstruction
-Complete: Atresia
-Incomplete: Stenosis
Duodenal: most common
-Jejunum and ileum: equal
-Rectum: rare
Developmental failure
intrauterine vascular accidents, or intussuception
Imperforate anus
2- Meckel’s Diverticulum
Persistence of omphalomesenteric duct (vitelline duct) (on anti-mesenteric side)
True : all layers.
Disease of 2’s
-2% of population (mostly asymptomatic)
- 2:1, M:F
-2 inch in length
-2 ft of ileocecal valve
-2 types of ectopic tissue in 1/2 of cases (gastric and pancreatic)
-2 major complications (pain with inflammation; hemorrhage with ulcer)
3- Congenital Aganglionic Megacolon“Hirschsprung Disease”
Absence of ganglia (failure of migration of the neural crest cells and arrest at some points before reaching the anus).
Loss of both submucosal (Meissner) and myenteric (Auerbach) in a segment and loss of neural coordination and functional obstruction.
M:F 4:1. and can be in sporadic or familial cases.
1 in 5000 to 8000.
Down syndrome (10% of HD) and (5%) serious neurologic abnormalities.
Genetic defects:
Endothelin 3
GCDGF
Receptor tyrosine kinase.
Acquired in Chagas disease (typanosomiasis), neoplastic obstruction, toxic megacolon, and functional.
Clinical features
Presents in neonatal period (failure to pass meconium; abdominal distention)
Risk of perforation, sepsis, enterocolitis, fluid disturbances and rupture in advanced cases.
Alternating obstruction and diarrhea
The rectum is always affected, with variable involvement of proximal segments,
Aganglionic segment causes functional obstruction with distention proximal to aganglionic segment, which may be massive reach to 15-20 cm in diameter.
Vascular diseases:a. Ischemic bowel diseaseb. Angiodysplasiac. Hemorrhoids
Ischemic bowel disease:
Acute obstruction of one artery may lead to infarction of mm. 50-75% death rate.
Old individuals, pain and tenderness, bloody diarrhea, rigid abdomen and paralytic ileus.
Insidious loss has no effect (anastomosis), and present with chronic ischemic colitis, with episodes of bloody diarrhea.
Transmural infarction result from mechanical obstruction of major artery.
Mucosal or mural infarction more often results from hypoperfusion (acute or chronic).
The predisposing conditions of ischemia are:
1- arterial thrombosis: in severe atherosclerosis, at origin of aa. Or arteritis, surgical accidents, dissecting aneurysm, hypercoagulable state.
2- arterial embolism.
3- venous thrombosis.
4- Non occlusive ischemia HF, shock, dehydration, drugs.
5- Miscellaneous as radiation, volvulus, stricture or hernia.
Embolus: superior mesenteric artery branches, source: embolus of heart (mural thrombus, valvular vegetation)
Vascular diseases:a. Ischemic bowel diseaseb. Angiodysplasiac. Hemorrhoids
Angiodysplasia
-tortuous dilatation of the veins in the submucosal and mucosal blood vessels with ectasia of veins.
Prone to rupture, and presents with massive GIT-bleeding (20% of significant massive lower GIT bleeding),
Prevalence:<1%
Sixth decade, pathogenesis, mechanical, with vascular degenerative changes in aging.
Osler-Weber-Rendu syndrome (hereditary hemorrhagic telangiectasia)
Hemorrhoids
dilated veins of hemorrhoidal plexus
-Internal
-External
-(BPR or streaks on stool), thrombosis, pain
5% of population
elevated venous pressure
constipation
straining venous stasis of pregnancy
collateral channels in portal HTN
rare under 30 except in pregnant women
Enterocolitis
Infectious
Necrotizing
Pseudomembranous
Infectious
-Viral (Rotavirus, Norwalk)
-Bacterial
E. coli; Shigella; V. Cholerae; C. difficile
-Parasites and protozoa (nematodes; flatworms; protozoa -Giardia lambdia; E. histolytica)
Diarrhea
Secretory Diarrhea more than 500 ml per day fluid which is isotonic with plasma and persist in fasting.
Osmotic diarrhea output more than 500 ml per day osmotic forces by luminal solutes that abate on fasting.
Exudative diarrhea
(WBC & RBC in stool) that persist in fasting.
Malabsorptive: long term weight loss, voluminous bulky stools with increased osmolarity of it due to unabsorbed nutrients, and excess fat.
Diseases
Viral enterocolitis
Rota virus , self limiting.
Adenovirus (dsDNA)
ETEC Cholera-like toxin (Food, water )
Watery diarrhea, traveling diarrhea
EHEC(STEC) Shiga-like toxin (Undercooked beef products)
Hemorrhagic colitis, hemolytic-Uremic syndrome
EIEC (Cheese, water)
Fever, pain, diarrhea, dysentery
Salmonella enteritidis:
Milk, beef, eggs, poultry
Self limiting diarrhea, dysentery pain, bacteremia.
Shigella:
Person-to-person. Milk, poultry,
Produce mucosal ulcer ,Fever, pain, Exudative diarrhea ,dysentery, epidemic spread
Vibrio cholera:
Water borne,
Watery diarrhea, cholera, pandemic spread
Giardiasis
Morphology, clinical features: malabsorptive diarrhea.
Staphylococcus aureus:
Milk product and fatty food.
Acute explosive Exudative diarrhea.
Clostridium difficile :
Following antibiotic use, nosocomial acquisition Fever, pain, bloody diarrhea,
Campylobacter :
Milk, poultry, animal (dog) contact.
Fever, pain, Secretory Diarrhea, dysentery
Clostridium perfringens:
Produce gas gangrene
Others
Tuberculous infection→
Transverse ulcer and Caseating granuloma
Pseudomembranous colitis→
C. difficile.,
Gross and Micro: pseudomemnrane
Amebiasis→
Bloody exudative diarrhea
Flask shaped ulcer, complications: liver abscess
Necrotizing enterocolitis
Acute, necrotizing inflammation of small and/or large intestines
Most common acquired GI emergency in premature or low birth weight neonate
Mild GI symptoms or fulminant illness
Multifactorial - immaturity of the gut’s immune system
Release of cytokines and endotoxins damages mucosa and blood supply
Edema to necrosis to gangrenous bowel
Terminal ileum or ascending colon
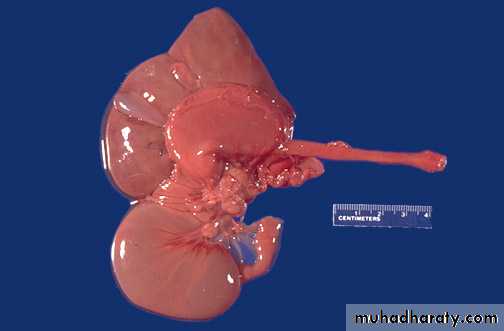
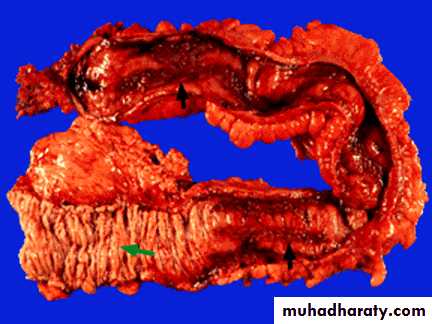
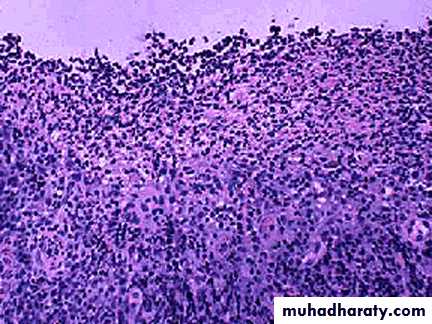
Necrotizing EnterocolitisMorphology
NEC typically involve the terminal ileum, cecum, & right colon. The involved segment is
Distended, friable, and congested, or it can be gangrenous. Peroration with peritonitis is
May be seen.
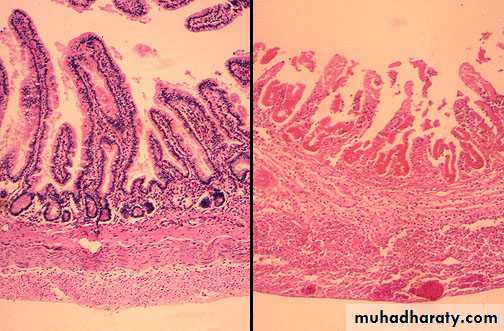
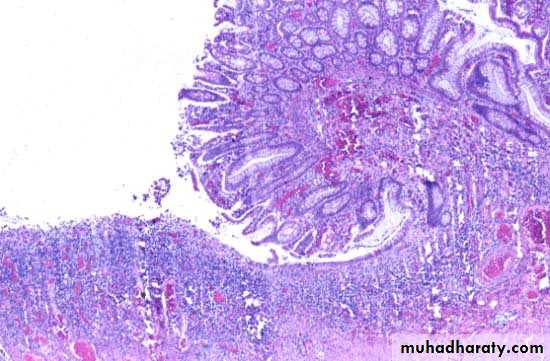
Necrotizing EnterocolitisMorphology
Necrotizing enterocolitis, mucosal surface (and comparison with normal) .The bowel is
distended, congested, and often frankly necrotic. (Compare the involved segment ofintestine below with the more normal segment above.)
Necrotizing EnterocolitisMorphology
Compared to normal bowel at the left, bowel involved by NEC at the right shows
hemorrhagic coagulative necrosis, beginning in the mucosa and extending to involve the
muscular wall, with the potential for perforation.
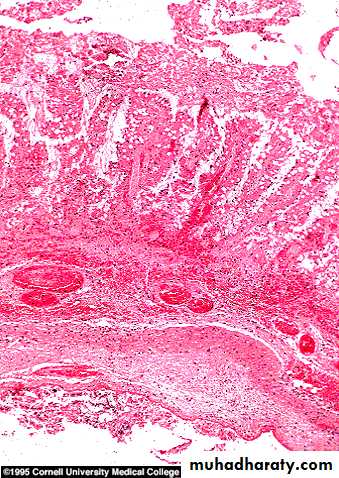
Necrotizing EnterocolitisMorphology
Transmural necrosis: when severe, the necrosis may progressively involve all layers of the bowel through to the serosa (transmural).
This type of involvement, which begins at the luminal aspect of the bowel, is typical of ischemic injury.
The necrosis is accompanied by variable amounts of inflammation and hemorrhage.
Necrotizing EnterocolitisMorphology
Pneumatosis intestinalis, necrotizing enterocolitis .Pneumatosis intestinalis, which is
present in many but not all cases, is represented by submucosal or subserosal gas-filled
cysts.
Pseudomembranous colitis (antibiotic associated)
Yellow green false membrane (mixture of mucous and neutrophils)
Toxin produced by Clostridium difficile (acquired nasocomially in 20% of pxs in long term hospitalization)
Antibiotics allow overgrowth of C. difficile
Sudden onset of fever and diarrhea in a patient who is seriously ill or post operative who is receiving antibiotics
diarrhea, dehydration, shock death
Exotoxin A and B
binds to enteric receptors
inactivates RhO cytoplasmic proteins
causing injury to actin filaments and
cell retraction
Malabsorption
Defect in the assimilation of food (digestion and absorption)
Intraluminal stage
a. Secretory Phase (Chronic pancreatitis/insufficiency)
b. Biliary Phase (Biliary obstruction due to calculus of or tumor)
Intestinal Stage (terminal digestion)
a. Surface Phase (Celiac disease; bowel resection)
b. Cellular Phase (Disaccharidase deficiency)
Removal Stage (transepithelial transport)
a. Delivery Phase (Whipple diease)
Celiac sprue
Etiology and pathogenesis:
Gluten, gliadin protein in wheat, oat, barley, and rye
hypersensitivity (immunologic) reaction to gluten
90-95% - HLA DQ heterodimer in Ch 6
Whites - rare in native Africans, Japanese, Chinese
Gluten - malabsorption -gluten free - improvement
Long term risk of malignancy -lymphoma (2X normal)
Distinct from Tropical sprue
Infant
Failure to thrive
Apathy
Pallor
Anorexia
Abdominal distention/pain
Developmental Delay
Muscle wasting
Hypotonia
Stools soft, bulky, malodorous, clay-colored
Child
Anemia
Rickets
Low weight
Small stature
Irritability
Adult
Diarrhea/ steatorrhea
Weight loss
Cheilosis / glossitis / Apthous ulcers
Anemia
Anorexia/nausea/vomiting
Flatulence/increased borborygmi
Lactose/sucrose intolerance
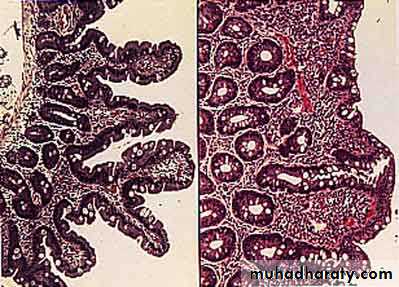
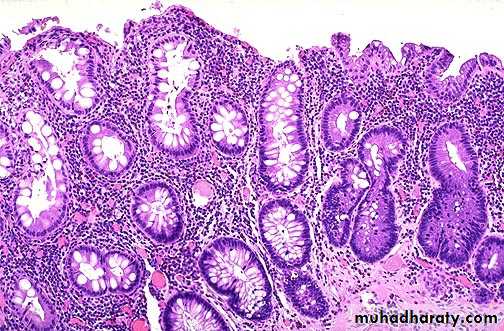
Morphology
Pathology
Excess lymphoctesHypertrophic crypts
Flattened villi
Hypoplasia
Blood tests
Antigliadin IgG and IgA
Endomysium IgA
Tissue transglutaminase IgA by ELISA
Total IgA
Tropical sprue
Occur in people living or visiting the tropics. (Caribbean, central and south Africa, India, south east Asia, central and south America).
No specific cause.
Characterized by bacterial overgrowth by enterotoxigenic organisms, e.g. E.coli, Hemophilus.
Morphology: variable, injury in cells, with increase in size of cells.
Malabsorption after the infection.
Treated by broad spectrum antibiotics.
Whipple disease
Rare systemic disease, affecting intestine, CNS and joints.Gram positive rod shaped actinomycete: Tropheryma whippleli
Engulfed by macrophages (PAS positive diastase resistant)
Electron microscopy
Seen in intestinal mucosa, mesenteric lymph nodes, joints and other systemic areas.
M:F 10:1, in fourth to fifth decade.
Mala, polyathritis, obscure CNS complaints.
Treated by antibiotics.
Bacterial overgrowth
The proximal small bowel is inhabitated by bacteria as in colon (aerobic and anaerobic).
The small bowel is not sterile but the peristalsis prevents overgrowth, which occur in:
1- Luminal stasis: stricture, fistula, diverticula, blind loop or pouch, reduplication, motility disorders, post-surgical.
2- Hypochrlohydria or achlorhydria, by gastric mucosal atrophy or anti-acid ingestion.
3- Immune deficiency.
The etiology of malabsorption will be multi-factorial:
1- bacterial deconjugation and dehydroxylation of luminal bile salts.
2- mucosal damage by bacterial enzymes.
3- bacterial inactivation of luminal lipase.
4- competition of nutrients.
Treated by appropriate antibiotics.
Disaccharidase deficiency
congenital = rare.
Acquired = common, by osmotic diarrhea.
Bacterial fermentation of unabsorbed sugar will cause hydrogen production = pH of stool will be decreased.
Abetalipoproteinemia:
Autosomal recessive disease= no lipoprotein B accumulation of triglyceride in mucosal cells.
Idiopathic Inflammatory Bowel disease
Inflammatory bowel disease (IBD) - single term to collectively refer to either Crohn’s disease or ulcerative colitis
Consists of two inflammatory disorders - Crohn’s disease (CD) and ulcerative colitis (UC)
Both are chronic, relapsing conditions of uncertain etiology
Both have systemic, extraintestinal inflammatory manifestations
Idiopathic Inflammatory Bowel disease: etiology and pathogenesis
Normally steady state of inflammation, balance between luminal factors and host defense.Etiology unknown, unexplained = idiopathic.
Genetic predisposition: HLA B27 & 10 fold increase risk of first degree relative
Abnormal host immunoreactivity:
impaired function of antigen presenting cells in bowel. 2- abnormal elaboration of cytokines. 3- abnormal function of natural killer cells. 4- induction of antiepithelial antibodies.
C. infectious causes, viruses, chlamydia, and mycobacterium.
structural changes, increased intestinal permeability to polyethylene glycol and alterations in mucin glycoproteins.
inflammation: products of inflammatory cells cause tissue injury.
Crohn disease: Regional enteritis GROSS EXAMINATION
1. Chronic inflammation involving all layers (transmural) of the SI
may occur at any point along the GI tract
primarily involving SI and LI.
40% SI Alone, 30% SI&LI, 30%colon alone. (may involve, duodenum, stomach, esophagus and even mouth.
2. Mucosa shows linear ulceration and fistula
3. Segmental involvement/sparing
Serosal creeping fat
terminal ileitis as it was 1st described in 1930’s, regional ileitis, granulomatous colitis.
4. Serosa is granular, dull and gray.
Gross: contd.
5. Wall is thick and rubbery.
6. Lumen is narrowed.
7. Sharp demarcation of diseased bowel segment from adjacent un-involved bowel wall. (when multiple segments involved = skip lesions).
8. Cobble stone appearance.
9. Narrow fissures develop, penetrate deeply cause bowel adhesion with fistula formation, or sinus tract formation.
10. free perforation or localized abscess.
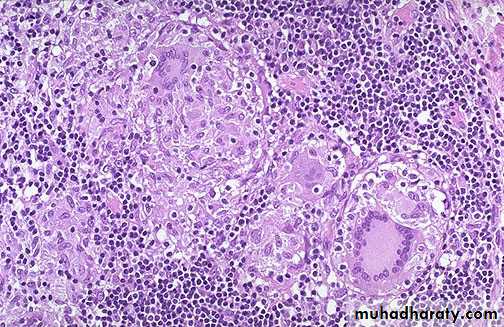
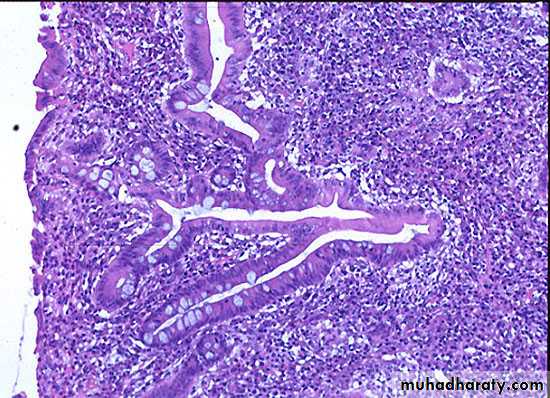
Crohn disease: microscopy:
Inflammation (transmural) spread through the bowel wall to adjacent mesenteric fat.Mucosal inflammation : neutrophils, and crypt abscess.
Ulceration in severe active disease.
Chronic mucosal damage (crypt distortion) with villous blunting in SI, atrophic changes, and metapalsia.
-characteristic non-caseating granulomas ( seen in half of cases, in all tissue layers, and involved and un involved areas).
CLINCAL FEATURES:
tends to occur in young adultsdiarrhea, crampy abdominal pain, fever
complications: 1-fistula, obstruction. 2- occult blood loss, Fe++ def anemia. 3- malabsorption, malnutrition, weight loss. 4- fistula and stricture. 5- extra intestinal manifestations: polyarthritis, sacro iliitis, ankylosing spondilitis, erythematic nodosum, clubbing of fingers, uveitis, amyloidosis, and increased incidence of cancer of SI and colon in 5-6 fold increase in risk.
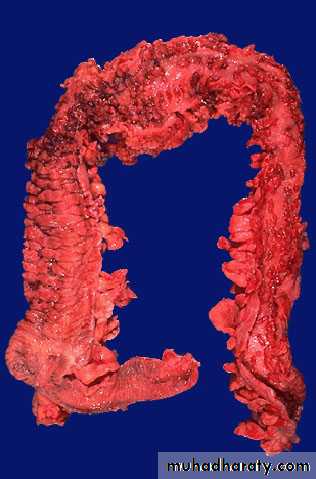
Ulcerative colitis
1. Inflammation primarily involving the mucosa of the colon.
2. Diffuse, continuous inflammation that begins in the rectum and progresses proximally. Pancolitis in 20%, 10% of these have backwash ileitis, remaining 40-50% rectosigmoid.
3. Pseudopolyp formation.
4. With chronic disease, there is atrophy.
5. Serosa normal.
6. Bloody diarrhea, from ruptured vessels in inflamed mucosa
Toxic megacolon - rare complication - prominent dilatation and septic shock.
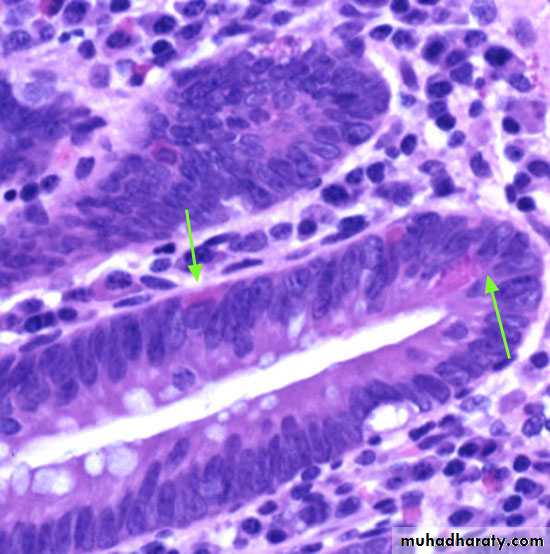
MICROSCOPY:
Early phase: neutrophils accumulate within the depths of the crypts of Leiberkuhn forming crypt abscesses.
Fibrosis cause crypt distortion. Mucous cell depletion.
Later phase: mucosa ulcerates and pseudo-polyps form
Late phase: after many years, mucosa becomes dysplastic, increasing risk of colon carcinoma
Clinical features:
ATTACKS OF BLOODY DIARRHEA.days, weeks, months and then subside.
Recur after months, and then subside.
Could be only single attack.
PROGNOSIS:
60% mild disease.
97% relapse within 10 years.
30 % colectomy in first 3 years (uncontrollable disease).
Rarely fulminant = fatal.
RISK OF CANCER: dysplasia in multiple sites.
High in patients with pancolitis for 10 years or more, (20-30 fold increase risk).
If 35 years, there is 30% cancer development.
Between Crohn and UC, this finding is more commonly seen in: Transmural inflammation--
Pseudopolyp---------------
Granuloma-----------------
Diffuse---------------------
skip lesions----------------
toxic Megacolon-----------
creeping fat----------------
Primary Sclerosing Cholangitis--
fissures and fistulas-------
Cancer----------------------
at any point in GI tract---
Rectum---------------------
Crohn
UC
Crohn
UC
Crohn
UC
Crohn
both but more in UC
Crohn
both but more in UC
Crohn
UC
Non-neoplastic bowel diseasesa. Diverticular diseaseb. Herniasc. Adhesionsd. Intussusceptione. Volvulus
Diverticular disease:
Diverticulosis and Diverticulitis
Acquired herniation
Most common in left colon; particularly sigmoid colon
Acute or chronic inflammation may occur
Perforation, peritonitis, fistula
Acquired
rare under 30
western pop over 60 prevalence: 50%
Non-neoplastic bowel diseasesa. Diverticular diseaseb. Herniasc. Adhesionsd. Intussuceptione. Volvulus
Hernias
-Serosal lined out-pouching of peritoneum
-Loop of intestines becomes trapped (incarcerated) within the hernia sac
-Bowel compressed, twisted at the mouth of hernia, compromising blood supply - infarction (strangulation)
Non-neoplastic bowel diseasesa. Diverticular diseaseb. Herniasc. Adhesionsd. Intussuceptione. Volvulus
Adhesions
-string-like or band-like portions of scar tissue that form during healing after surgery or peritonitis
-may result in obstruction (kinking, compression)
Non-neoplastic bowel diseasesa. Diverticular diseaseb. Herniasc. Adhesionsd. Intussusceptione. Volvulus
Intussusception
-caused by an in-folding or telescoping of one segment of bowel into the adjacent distal segment
Infants and children: spontaneous and reversible
Adults: tumor is usually a lead point
Non-neoplastic bowel diseasesa. Diverticular diseaseb. Herniasc. Adhesionsd. Intussuceptione. VolvulusVolvulus
-obstruction due to rotation or twisting of a loop of bowel around its mesenteric base of attachment
Sigmoid - most common site (cecum next)
Inflammation
1. Miscellaneous
-graft vs. host
-drug induced
-radiation enterocolitis
-neutropenic colitis
-diversion colitis
2. Acute appendicitis
-etiology: bacteria
-fecolith impairing circulation, causing ischemia, necrosis and bacterial contamination
-acute abdomen -RLQ pain- McBurney’s point
-fever and leukocytosis
Inflammation3. Collagenous and lymphocytic colitis
Etiology: unknown
possibly auto-immune
chronic watery diarrhea in middle aged and older women
spectrum of disease ranging from increased intraepithelial lymphocytes to the presence of collagen band under the surface epithelium