Odontogenic infections and pyogenic infections of the
soft tissuesInfection: is the invasion and the multiplication of pathogenic microorganisms into the body or tissue which may produce subsequent tissue injury and progress to overt disease through a variety of cellular or toxic mechanisms.
The pathogenic organisms can be Bacteria, Viruses, Fungi or Protozoa.
The body's response to infectious agents is inflammatory response which is essentially protective, it consists of:
• • Hyperemia caused by vasodilatation of the arterioles and capillaries, and release of permeability factors to allow for the passage of nutrients and leukocytes.
• • Precipitation of a network of fibrin to wall off the infected region.
• • Phagocytosis of bacteria and other organisms as well as dead cells.
• Disposal by macrophages of necrotic debris. Depending on the duration and severity of the infection,
• the inflammatory response is divided into:
Acute inflammation; with rapid progression and typical signs and symptoms. (usually with sudden onset, marked by classical signs of heat, redness, sawelling, pain and loss of function )
Subacute inflammation; considered as transition between acute and chronic inflammation.
Chronic inflammation; associated with longer duration and slight clinical symptoms.
Infections could be local; confined to one body system, or generalized like Septicemia.
Signs and Symptoms of infection
These include systemic signs and symptoms like; fever, malaise and anorexia. There are also local signs and symptoms, which are present to some degree in all patients:
Redness, it results from vasodilatation.
Swelling, in infection it results from accumulation of tissue fluid or pus.
Heat, results from the inflow of warm blood from deeper tissues, increased velocity of blood and increased metabolic rate.
Pain, results from pressure on the nerve endings, also from the action of liberated or activated factors such as Kinins, Histamine and Bradykinin on nerve endings.
Loss of function, caused by mechanical factors and reflex inhibition of muscle movement associated with pain.
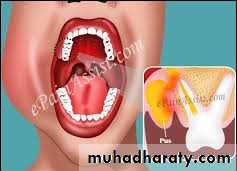
Odontogenic Infections
They are almost always bacterial in origin, they consist of Periapical, Periodontal or Pericoronal in infections.Periapical infections
These infections arise from necrotic pulp which arise from a carious tooth or contaminated traumatic exposure of the pulp invade the periapical tissues through the apical foramen,sometimes the bacteria gain access through an accessory canal or through bifurcation area leading to infection that presents on the lateral surface of the tooth.
These infections manifest themselves as primary acute infections or as an exacerbation of a preexisting chronic periapical infection.
The main clinical features include; (signs and symptoms)
• a non vital tooth,
• the tooth is tender to bite and to percussion, the periapical region is tender to pressure,
• the tooth is slightly raised in the socket due to the acute inflammation and swelling of the periodontal ligament ,
• the tooth may be mobile.
• There is an intense throbbing pain,
• if treatment is delayed bone resorption will allow the pus to drain under the periosteum with diminution of pain intensity.
A periapical radiograph may show no significant changes except for widening of the periodontal space especially in acute infections or it may reveal the presence of periapical radiolucency.
Periodontal infections
Arise from preexisting periodontal pocket, in some cases food impaction or repeated occlusal trauma are the precipitating factors.Signs and symptoms:
The teeth involved are not necessarily non vital, an acute infection produces redness and swelling near the gingival margin, the pain is continuous, dull or throbbing but usually less than that experienced in acute periapical infections, pus may discharge from the gingival margin or may produce sinus. The tooth may be mobile.
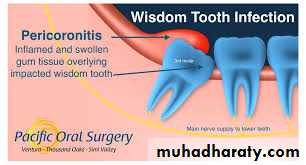
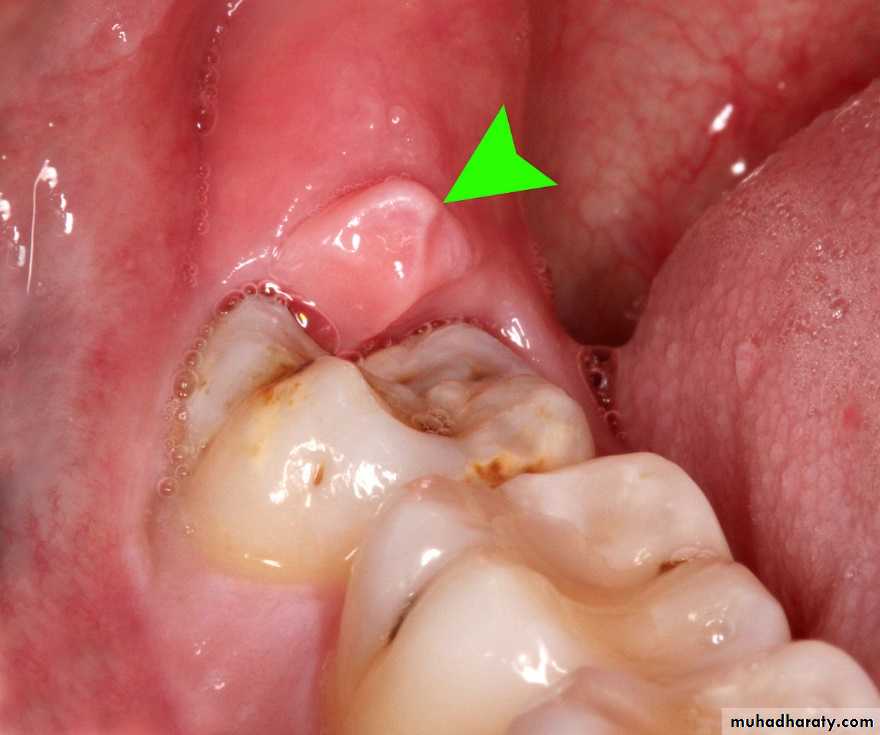
Pericoronal infections
Also called pericoronitis is an infection of the soft tissue covering the crown of a partially erupted tooth, it is almost always associated with partially erupted impacted lower third molars.Etiology involves:
• Food impaction between the crown and the overlying gum (operculum) which is a favorable site for bacterial proliferation and inflammation.
• Trauma to the overlying gum from the opposing tooth, but it is hard to determine whether the trauma occurs before or after the inflammatory edema of the gum.
• Virulent microorganism.
• Lowering of the host resistance.
Pericoronitis appears to be the result of a combination of the four mentioned etiological factors.
• The clinical presentation depends on the severity of infection:
Chronic pericoronitis is either asymptomatic or there is mild discomfort.
In Subacute pericoronitis there is a dull pain which is well localized, the gum pad may be tender and red and there may be expression of a white material from underneath the gum flap, this material is composed of desquamated epithelial cells, food stuff, dead and living bacteria, there may be slight trismus and lymphadenopathy (LAP).In Acute pericoronitis there is severe pain and limitation of mouth opening, intraoral swelling and there may be extr-aoral swelling as
well as fever, malaise and LAP. Pus may be expressed from underneath the flap, sometimes the pus may track submucosally and is expressed from a sinus in the molar or premolar region, this is termed migratory abscess.
In treating pericoronitis, if is essential to determine if the tooth is likely to achieve full eruption, this is done by full clinical and radiographic examination, consideration should be given to the age of the patient and history of previous attacks.
Treatment of pericoronitis consists of:
• Drainage of abscess if present
• If there is no abscess, gentle irrigation of the pericoronal space with normal saline, sometimes an antiseptic solution can be instilled in this space.
• If the upper third molar irritates the swollen gum flap, the pressure should be relieved by extraction or grinding the offending cusps
• Antibiotics are needed for cases of acute infections.
• Surgical extraction of the impacted teeth should be carried out after the inflammation subsides.
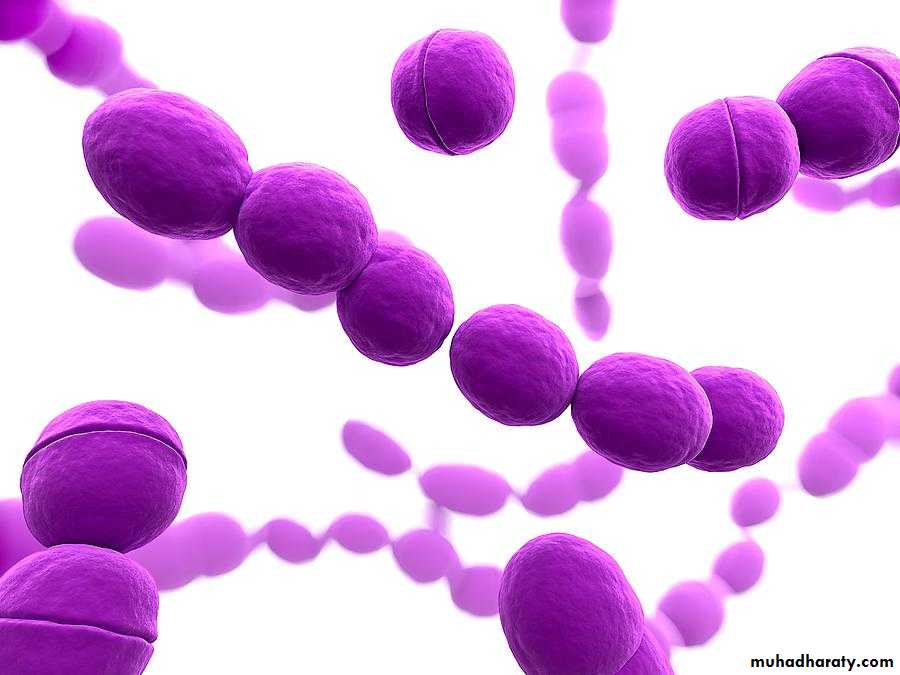
Bacteriology
Odontogenic infections are caused mostly by bacteria that live on or in the host, when such bacteria gain access to the deeper tissues, they cause infection.Most Odontogenic infections are mixed infections, caused by multiple bacteria (aerobic and anaerobic), with an average of five species involved.
The most common aerobic bacteria involved in odontogenic infections are Streptococci and Staphylococci (Aureus and epidermidis), other less common aerobic organisms include Neisseria species, Corynebacterium species and Haemophilus Influenzae. While the most common anaerobic bacteria are an aerobic Streptococci species, Peptostreptococcus, Bacteroids and Fusobacterium species.
Spread of odontogenic infections
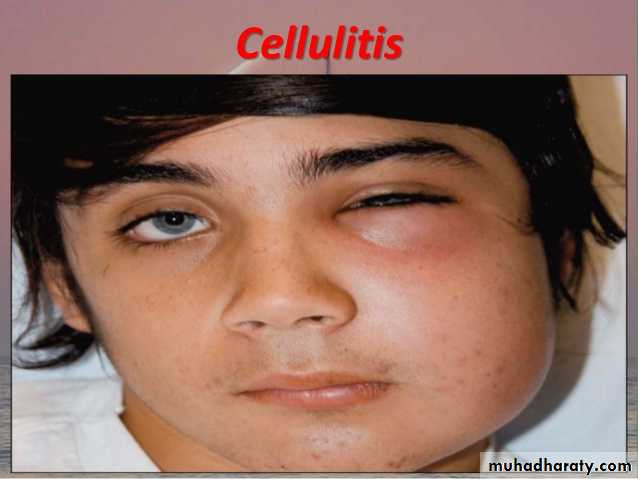
Odontogenic infections may spread beyond the confines of the dentoalveolar bone into the soft tissue, they may be presented as:Cellulitis; which results from spreading of infection into the loose connective tissues (C.T.) it presents as:
• a warm, diffuse, erythematous, indurated and painful mucosal or cutaneous swelling.
• It does not result in the formation of large amount of pus,
• Streptococci are more often associated with cellulitis, and these organisms produce enzymes such as Streptokinase and Hyaluronidase that break down fibrin and C.T. ground substance, facilitating the rapid spread of infection.
• Antibiotics and removal of the cause of infection are usually sufficient.
• Incision and drainage are indicated if there is no improvement or if evidence of purulent collection is identified.
Suppurative infections; characterized by abscess formation, which can be defined as thick walled pocket of tissue containing pus. Pus consists of necrotic tissue dead and living bacteria and dead white cells, it is often associated with Staphylococci and anaerobes such as bacteroids S. aureus produce the enzyme coagulase that coats the bacteria with fibrin and reduces the ability of the cells to phagocytize it. The area of infection may or may not be fluctuant, treatment is by incision and drainage with antibiotics, followed by the treatment of the cause of infection.
Spread of infection can occur through the following routes:
I. By direct continuity through the tissue.2. By the lymphatic to the regional lymph nodes which may result in secondary infection. In acute infections the lymph nodes are enlarged, soft and tender, the surrounding skin may be red and edematous. In chronic infections the enlarged nodes are more firm, not tender with no redness or edema of the surrounding skin.
3. By blood stream, this is uncommon; it occurs along the veins, it can result in serious complications like cavernous sinus thrombosis and septicemia.
The factors that influence the spread of odontogenic infections:
1. Virulence of the organism, it is the disease producing ability of the organisms.2. Status of patient's immune system, several conditions affect the general health of the patient adversely such as diabetes, malnutrition, alcoholism, HIV infections or patients taking immunosuppressive drugs.
3. Anatomical factors influencing the direction of spread of infection such as:
• The site of the source of infection.
• The point at which the pus escapes.
• The natural barriers to the spread of pus such as fascia, muscles or bone.
Physical examination
Include : inspection, palpation and percussion. It aims to identify the signs and symptoms of infection like the presence of swelling, redness or draining fistula.
Palpation is used to examine the size, note the tenderness, assess local temperature and to determine the presence of fluctuation. Trismus should be noted with measurement of the interincisal distance.
Intraorally, the teeth and gingiva should be examined for the presence of caries, restorations or localized swelling. Percussion determines the areas of tenderness. Pulp testing may be needed to assess the vitality of the teeth. The intraoral examination should include the ducts of the parotid and submandibular salivary glands, tongue, soft palate, tonsillar fossa and oropharynx. Manifestations of serious odontogenic infections may include; airway compromise, septicemia, fever, lethargy, fatigue, dehydration, rapid progression, dysphagia, odynophagia and drooling.
Other investigations are radiographs to identify the cause of infection, periapical, occlusal and OPG radiographic views are used. Ultrasound, CT scan and MRI can also be used in deep infections. Laboratory studies are also indicated to evaluate the immune system, white blood cells (WBC) and differential WBC count.