pathology of Renal System
Dr.Shatha Th.Ahmedassistant professor/Ninevah college
PhD pathology/UK
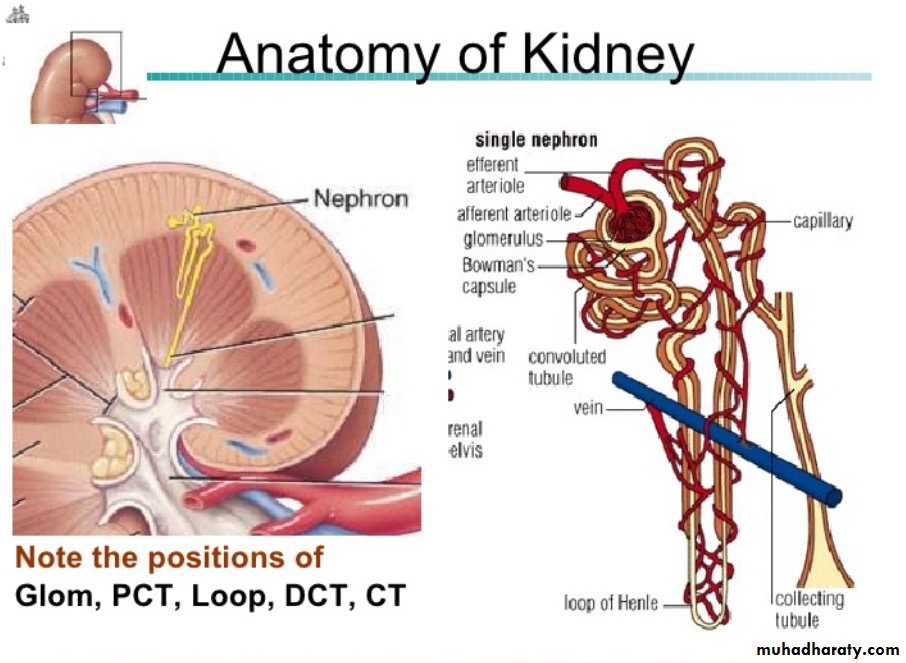
The kidneys function to:1. Excrete the waste products of metabolism.2. Regulate the body's concentration of water and salts.3. Maintain the appropriate acid-base balance of plasma.4. Serve as an endocrine organ secreting some hormones as erythropoietin, renin and prostaglandins.
Each human adult kidney weighs about 150 gm.
Anatomically the ureter forms the pelvis which is divided into 2 or 3 major calyces, each one giving 3 or 4 minor calyces.
The kidney is divided into the cortex 1.2-1.5 cm and medulla.
The medulla consists of renal pyramids, the apices of which are called papillae, each related to a calyx.
the functional unit of the kidney is the nephron. Each kidney contain about one milion nephron
Definition of Some Clinical terms in Renal Diseases
Azotemia: is an "elevation of Blood Urea Nitrogen(BUN) i and creatinine levels". It is largely related to a decreased glomerular filtration rate (GFR). Azotemia is divided into1. Prerenal azotemia, encountered with hypoperfusion of the kidneys, which decreases GFR as in shock states.
2. Renal, which is due to renal parenchymal damage
3. Postrenal that results from urine out flow obstruction below the level of the kidney.
Uremia: = Azotemia + Clinical signs and symptoms + Biochemical abnormalities
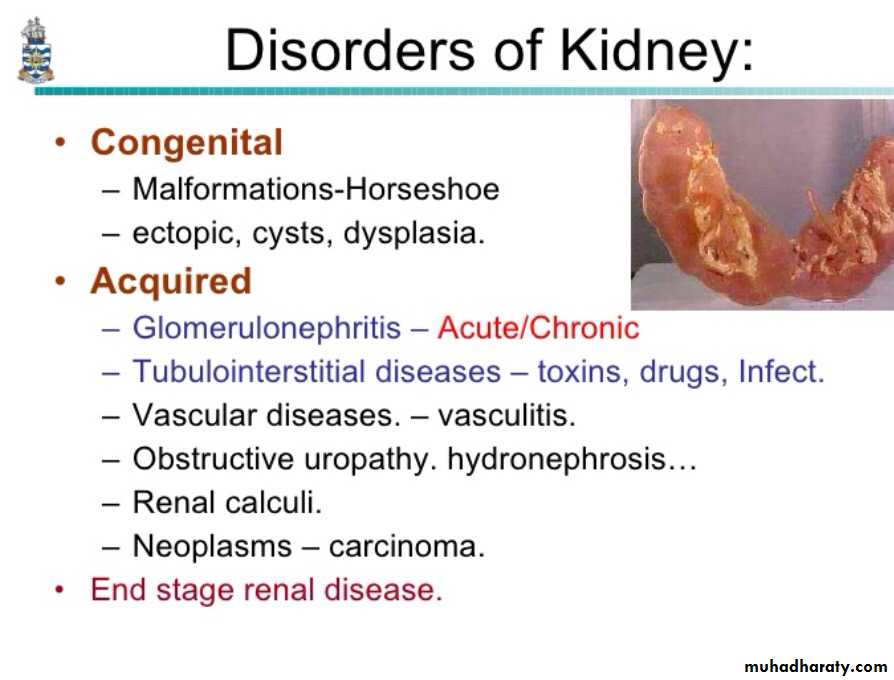
– There is secondary presence of uremic gastroenteritis, peripheral neuropathy and uraemic pericarditis.Cystic Diseases Of The Kidney
They are heterogeneous group comprising hereditary, developmental and acquired disorders.They are important for several reasons;
1. They are reasonably common and often represent diagnostic problems for clinicians, radiologists and pathologists.
2. Some forms are major causes of chronic renal failure.
3. They can occasionally be confused with malignant tumors.
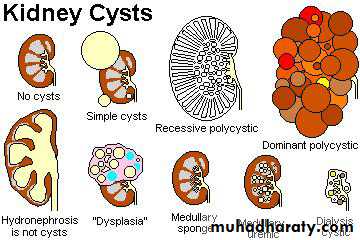
Classification;
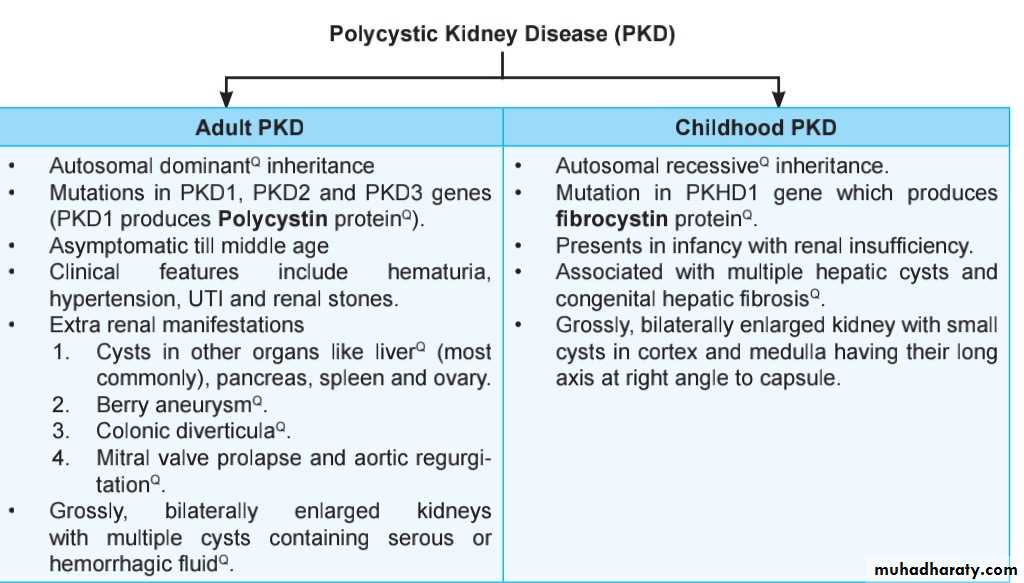
1. Simple renal cyst.2. Cystic renal dysplasia
3.polycystic kidney disease a. Autosomal dominant (adult) type. b. Autosomal recessive (childhood) type.4.Medullary cystic disease. a. Medullary sponge kidney. b. Nephronophthisis.
5.. Acquired (dialysis-associated) cystic disease.6. Renal cysts in hereditary malformation syndromes (e.g. Tuberous sclerosis).7. Glomerulocystic disease.8. Parasitic cysts (e.g. hydatid cyst).
Simple Cyst
These occur as single or multiple, usually cortical.The size range from 1-10cm or more.
They are translucent and filled with clear fluid.
They are lined by a single layer of cuboidal or flattened epithelium.
They are common postmortem findings. On occasion, hemorrhage into them may cause sudden pain, and calcification may be visible radiologically.
The main importance of these cysts is in their differentiation from kidney tumors.
clinical features of APCK :"b"
signs: bloody urine complicationsbigger kidneys Berry aneurysm
bilateral loin pain Biliary cysts
bloodpressure up Bilateral valve prolapse
Accelerators:
boysblack
blood pressure high
Acquired (Dialysis-Associated) Cystic Disease
The kidneys of patients on chronic dialysis, sometimes exhibit numerous cortical and medullary cysts. The cysts measure 0.5-2cm,contain clear fluid, are lined by either hyperplastic or flattened tubular epithelium
and often contain calcium oxalate crystals.They probably form as a result of tubular obstruction due to interstitial fibrosis or by oxalate crystals.
The most ominous complication is the development of renal cell carcinoma in the walls of these cysts in about 7% of patients during 10 years period.
Glomerular Diseases:
Glomerulonephritis(GN) is a group of diseases that injure the part of the kidney that filters blood (called glomeruli)
Other terms you used are "nephritis" "glomerulonephritidis" and"glomerulopathy".
When the kidney is injured, it cannot get rid of wastes and extra fluid in the body. If the illness continues, the kidneys may stop working completely, resulting in kidney failure.
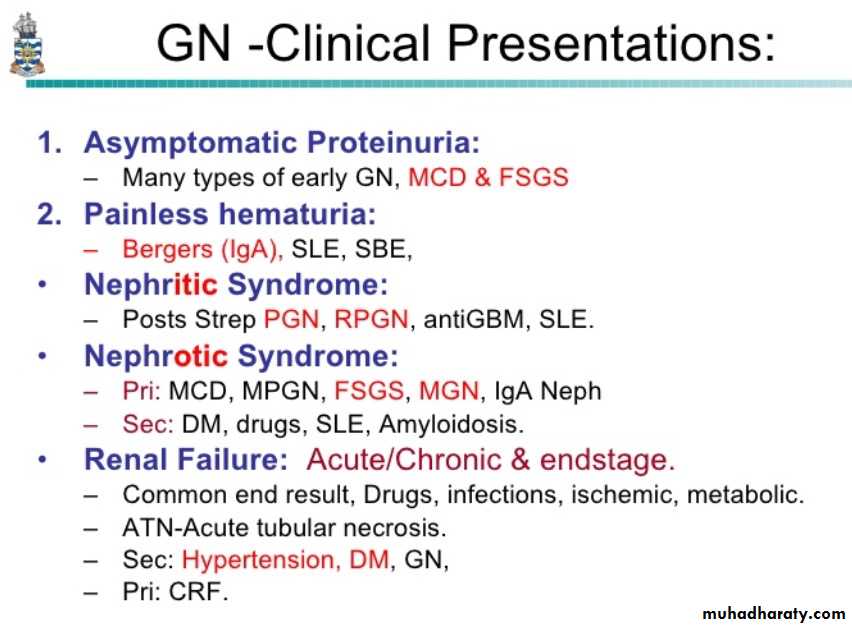
GLOMERULAR DISEASES
Primary Glomerulonephritisacute proliferative GN (APGN).Rapidly progressive RPGNMembranous MGNLipoid nephrosis (minimal change disease)MCDFocal segmental glomerulosclerosis FSGMembranoproliferative MPGNIgA NephropathyChronic GN
Secondary (Systemic) DiseasesSystemic lupus erythematosusDiabetes mellitusAmyloidosisGoodpasture’s syndromePolyarteritis nodosaWagener’s granulomatosisHenoch-Scholein purpuraBacterial endocarditis
. Hereditary Disorders Alport’s syndrome Fabry’s disease
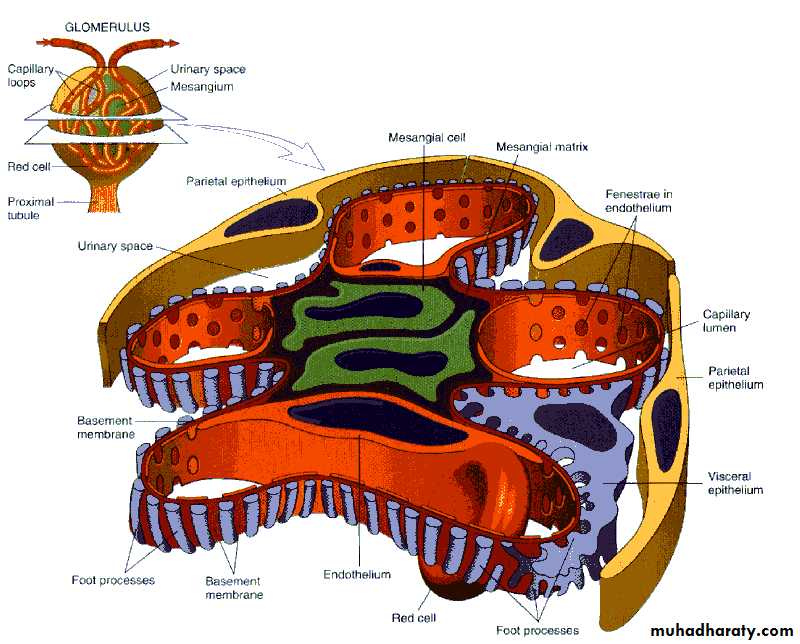
The glomerular basement membrane shows selective permeability, which is size- dependent and charge-dependent. The major characteristics of glomerular filtration are
1. A high permeability to water and small solutes
2. Almost complete impermeability to molecules of the size and molecular charge of albumin.
3. More permeability to cations than anions.
4. it depends on hydrostatic pressure differences.
The podocyte is supportive to the glomerular barrier function by providing a distal resistance to the flow of water and a barrier to the filtration of proteins. It is also largely responsible for synthesis of GBM components.
descriptive terms for GN
• all glomerulidiffuse >50%
focal < 50%
• individual glomeruli
global : if all or almost all of the glomerular tuft is affected.
segmental : if only part of the glomerulus is affected.
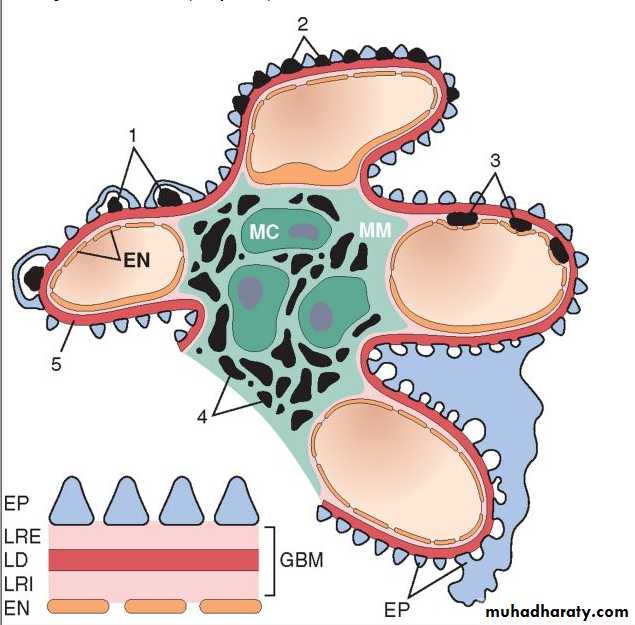
Localization of immune complexes in the Glomerulus
1. Subepithelial humps,
2. Epimembranous deposits,
3. Subendothelial deposits,
4. Mesangial deposits,
5. Basement membrane.
EN, endothelium; EP, epithelium; LD, lamina densa; LRE, lamina rara externa; LRI, lamina rara interna; MC, mesangial cell; MM, mesangial matrix.
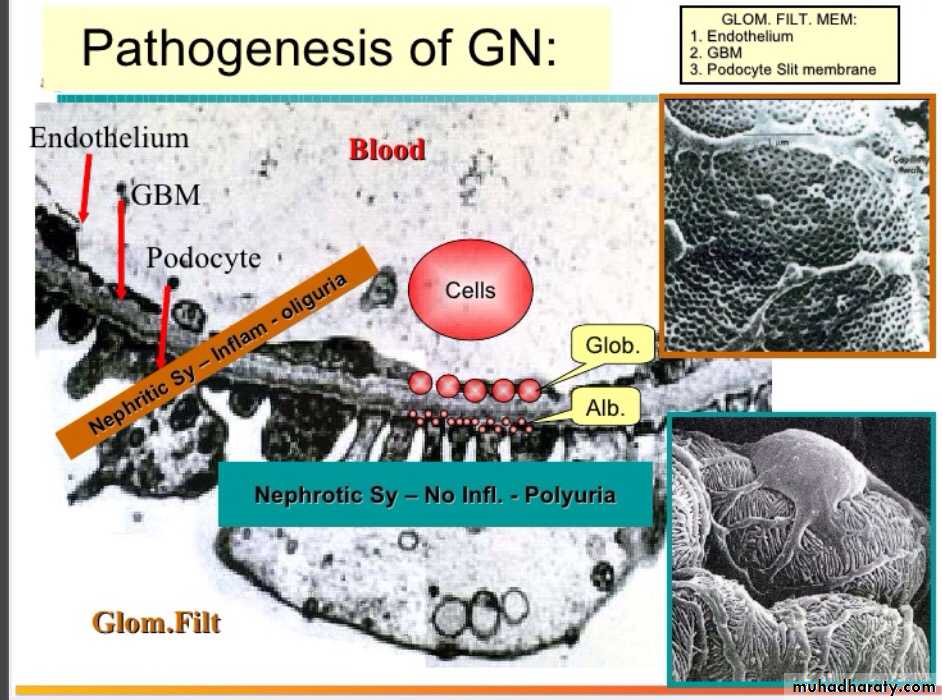
Pathogenesis
Although little is known about etiologic agents and triggering events, it is clear that immune mechanisms underlie most forms of primary glomerulopathies, and many of the secondary forms.I. Immune-mediated mechanisms; 1. Ab-mediated, a. Insitu immune complex deposition,
Fixed intrinsic antigens
Planted antigens (exogenous as infectious agent or drug and endogenous as DNA, immunoglobulins)
b. Circulating immune complex deposition
Endogenous Ag (DNA, tumor)
Exogenous Ag (infectious products)
c. Cytotoxic Ab
Pathogenesis-cont
2. Cell-mediated.3. Activation of alternative complement pathway.
II. Non-immune mechanism (adaptive changes secondary to renal ablation). like podocyte injury and nephrone loss