HEPATIC NODULES AND TUMORS
Focal Nodular HyperplasiaDefinition: It is a localized, well-demarcated consisting of hyperplastic hepatocyte nodules with a central, stellate fibrous scar.
It is not a true neoplasm but rather represents a response to abnormal vascular flow through a congenital or acquired vascular anomaly.
FNH may range in size from 1 cm to many centimeters across.
It usually is an incidental finding
Most commonly in women of reproductive age .
carry no risk for malignancy .
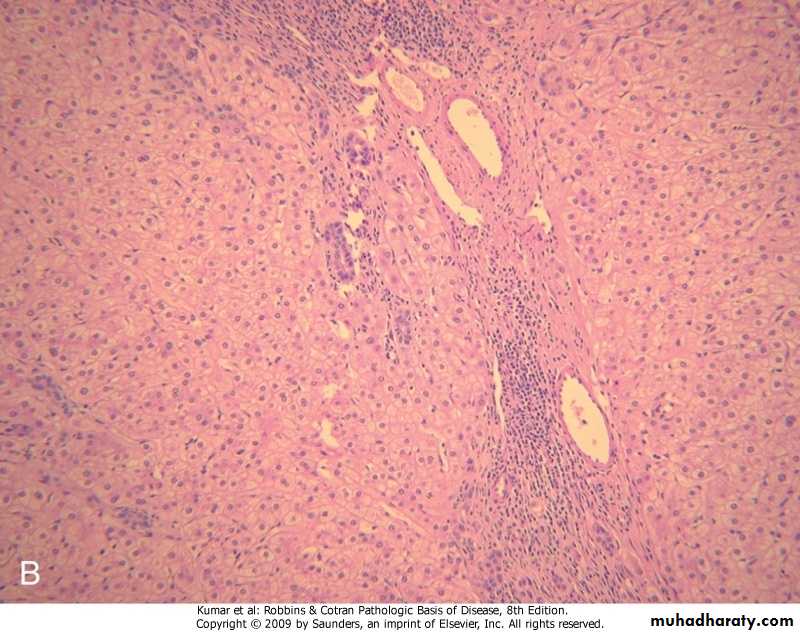
Morphology :
Gross yellowish with central gray-white, depressed stellate scar from which fibrous septa radiate to the periphery.Focal nodular hyperplasia
Focal nodular hyperplasia, hyperplastic hepatocyte nodules with a central fibrous septa contain dilated blood vessels and bile ducts.
Benign Neoplasms
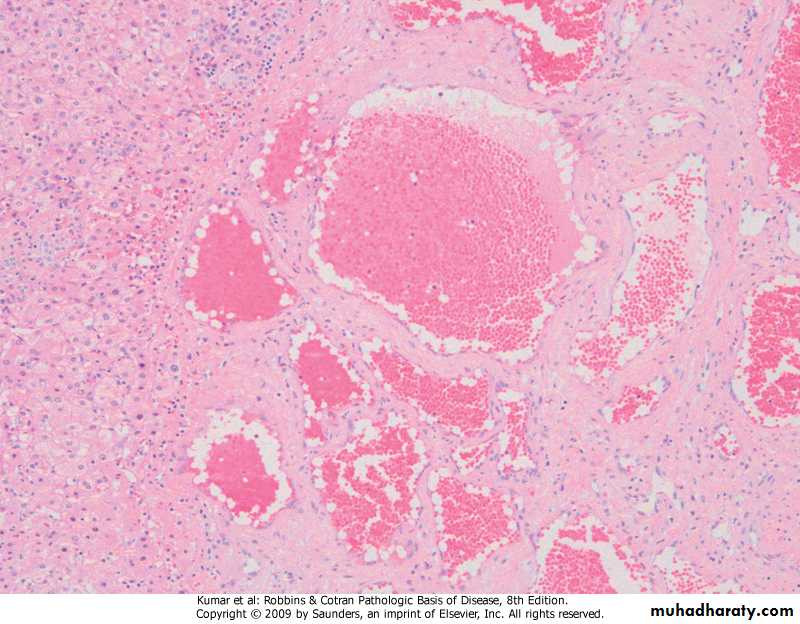
The most common benign lesions of the liver are cavernous hemangiomas.Haemangioma of the liver is seen beneath the capsule as a dark almost black lesion (typically 2-3 cm in size) which histologically, is composed of vascular channels in a collagenous stroma
Cavernous Hemangioma
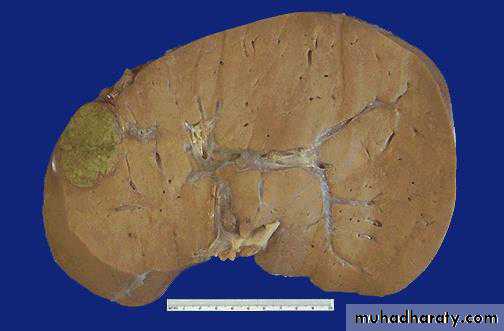
• Definition : benign hepatocellular neoplasm that usually occurs in women of child-bearing age who have used oral contraceptive pills, and it may regress on discontinuanceof hormone use.Liver cell adenomas are significant for three reasons: -Mistaken for hepatocellular carcinoma -Subcapsular adenomas may rupture, life threatening intraperitoneal hemorrhage -Rarely may transform into carcinomaHepatic Adenoma
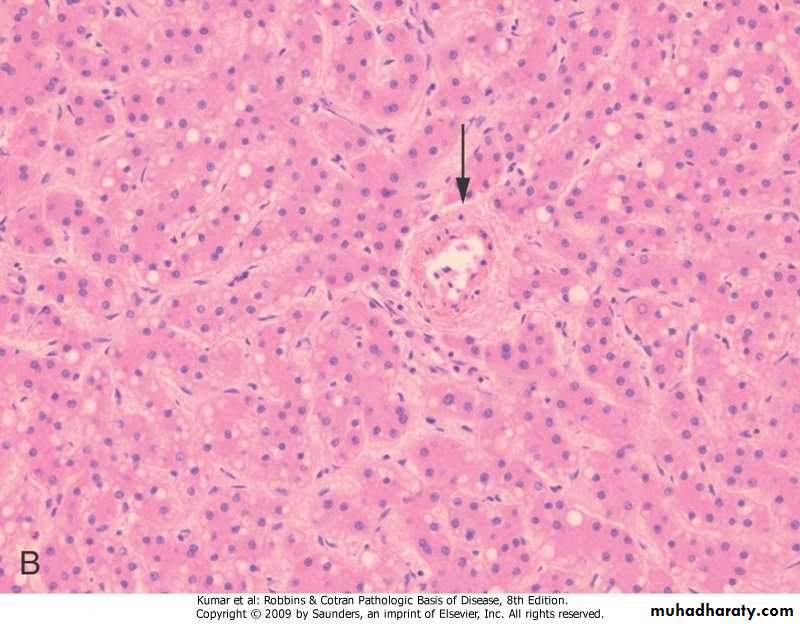
• Morphology -Grossly .well demarcated solitary or multiple nodules up to 30 cm in diameter .yellow-tan & frequently bile-stained . -Microscopy .sheets & cords of hepatocytes .no portal tracts, instead, prominent solitary vessels are present
Liver cell adenoma, yellow-tan, bile-stained nodule
Liver cell adenoma, sheets & cords of hepatocytes
MALIGNANT NEOPLASMS
Malignant tumors of liver can be primary or metastatic.• Metastatic Tumors
• More common than primary ones, the most common primaries: -breast -lung -colon
• Typically, multiple nodules .
• Primary cancers of liver
• Most arise from hepatocytes and are termed hepatocellular carcinoma (HCC).• Less common are cancers that arise from bile duct known as cholangiocarcinomas.
• Two rare primary liver cancers are: hepatoblastomas and angiosarcomas.
Hepatocellular Carcinoma (HCC)
Definition : malignant tumor derived from hepatocytes.Predominantly in males with a M:F ratio of 2.4:1.
Pathogenesis: It is multifactorial disease and complex in pathogenesis.
Major risk factors
1. Chronic hepatitis : HBV/ HCV
2. Alcoholic cirrhosis
3. Aflatoxin B1
4. Non-alcoholic steatohepatitis (NASH)
Minor risk factors
1. Hereditary hemochromatosis
2. Wilson's disease
3. α1-Antitrypsin deficiency
4. Glycogen storage disease
5. Oral contraceptives
6. Cigarette smoking
Morphology
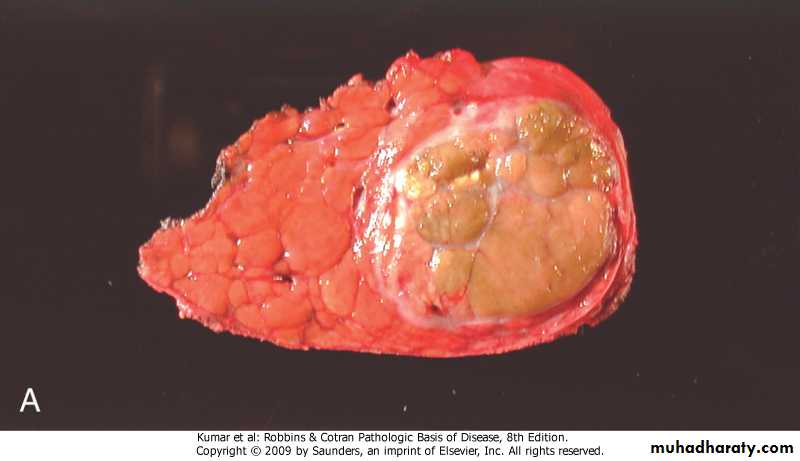
Gross :Enlargement of liver.
Areas of necrosis and hemorrhage .
light brown, yellowish-white or gray in color.
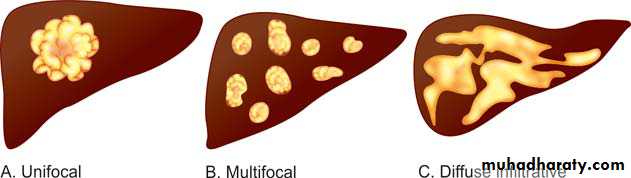
Three patterns.
A. Unifocal (usually large): Tumor appears as large circumscribed single mass .B. Multifocal: This multiple nodules of variable size widely distributed.
C. Diffusely infiltrative: large part of the liver or sometimes entire liver infiltrated by homogeneous indistinct tumor nodules.
Microscopy :
HCC range from well-differentiated, moderately differentiated, and undifferentiated (pleomorphic) forms.Hepatocellular carcinoma
Hepatocellular carcinoma
• Natural course -progressive enlargement seriously disturbing hepatic function. -Metastasizes, to lungs & other sites -five year survival of large tumors is dismal (death within first 2 years) -Death occurs from: .liver failure .rupture of tumor with fatal hemorrhage .cachexia .G-I or esophageal variceal bleeding
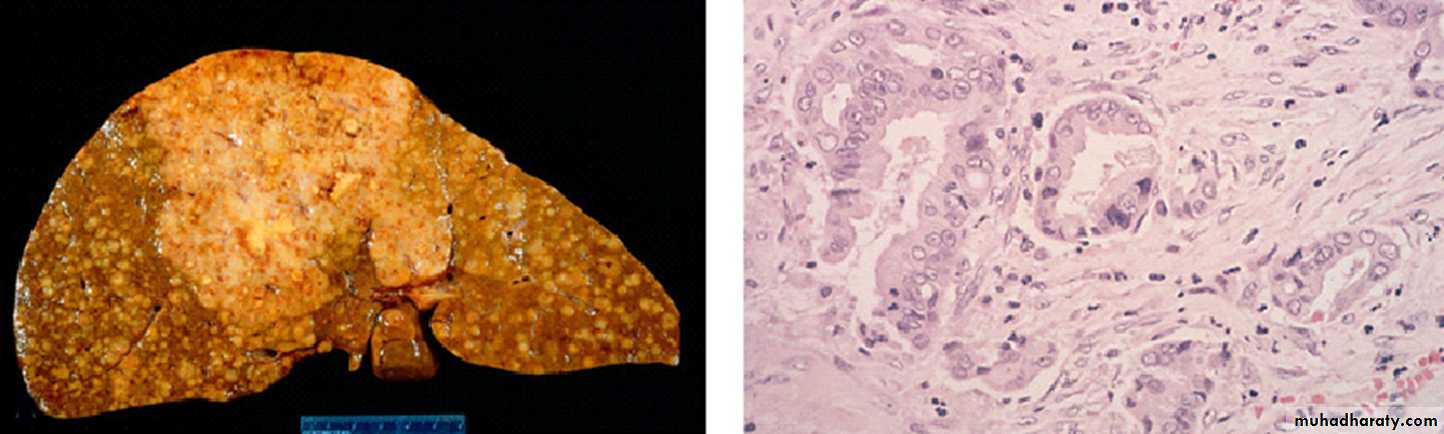
CHOLANGIOCARCINOMA (CCA)
It is the second most common hepatic malignant tumor.Site: It may arise anywhere in the biliary tree.
Classification:
Intrahepatic (about 10%)
Extrahepatic forms (about 80–90%)
Risk Factors
Primary sclerosing cholangitis (PSC).
Congenital fibropolycystic diseases of the biliary system such as choledochal cysts.
HCV infection.
Previous exposure to Thorotrast (formerly used in radiography of the biliary tract).
Chronic infection of the biliary tract by the liver fluke.
Morphology
GrossExtrahepatic CCAs: These are usually small lesions and appear as firm, gray nodules within the bile duct wall.
Intrahepatic CCAs: They develop in the intrahepatic portal tract.
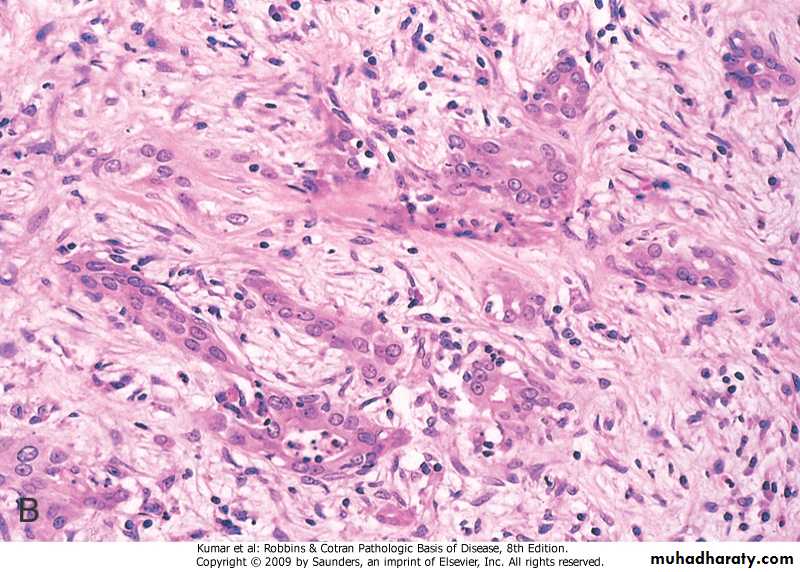
Microscopy
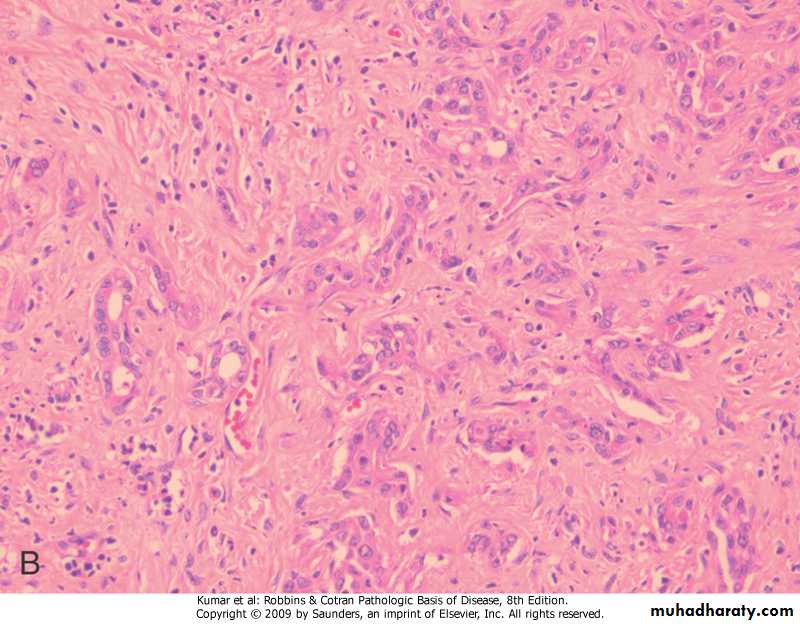
Adenocarcinomas: consist of well-defined glandular and tubular structures lined by cuboidal to low columnar epithelial cells.
Marked desmoplasia: It is characterized by dense collagenous stroma separating the glandular structures.
Cholangiocarcinoma
Gall Bladder
A storage organ for bile, with a capacity of 50 mL in adults Cystic duct joins common hepatic duct, common bile duct courses head of pancreas, duodenum through Ampulla of VaterACUTE CHOLECYSTITIS
Definition: an acute diffuse inflammation of the gallbladder.Types:
Acute calculous cholecystitis: It is associated with gallstone and is the most common
serious complication of gallstone.
Acalculous cholecystitis: It is not associated with gallstones and may occur in severely ill patients
Pathogenesis -calculous (chemical inflammation) -acalculous (ischemia)
MorphologyBoth acute acalculous and calculous cholecystitis are morphologically similar, except that stones are not seen in the acalculous form
Gross
Size: Gallbladder is usually enlarged, tense and edematous.Serosa: fibrinous exudate with subserosal hemorrhage.
Wall: It is thickened .
Mucosa: It is red or purple and may show ulcerations.
Lumen: In calculous cholecystitis, the lumen may contain one or more stones. The lumen is filled with turbid fluid.
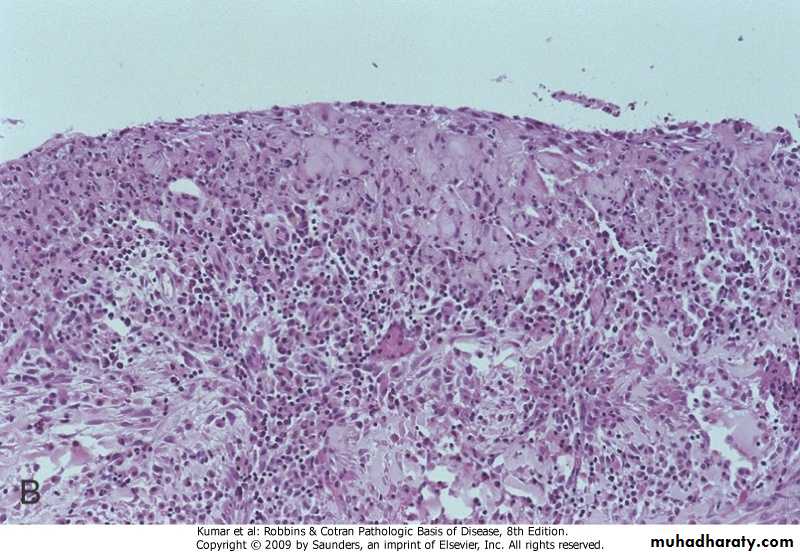
Microscopy
Mucosa shows focal ulcerations.
Wall of the gallbladder shows edema, hemorrhage and acute inflammatory cells. Secondary bacterial infection may lead to suppuration in the gallbladder wall.
Widespread necrosis is found in gangrenous cholecystitis.
Complications
1. Empyema of the gallbladder
2. Gangrenous cholecystitis
3. Acute gaseous or emphysematous cholecystitis
4. Perforation of the gallbladder
5. Bile peritonitis:
6. Pericholecystic abscess, abscesses in the liver or abdominal cavity.
7. Fistula into the intestine or duodenum
8. Gallstone ileus
CHRONIC CHOLECYSTITIS
Most common disease of the gallbladder.Associated with gallstones in ~90% of the cases.
May also develop following recurrent attacks of acute cholecystitis.
Morphology
Extremely variable and depends on the severity and the duration of the disease.Gross
Size: Gallbladder may be normal or may be shrunken in severe cases.
Serosa: It is usually smooth and glistening but may be dull due to fibrosis.
Cut section: The wall is thickened, opaque and gray-white.
Lumen: It usually shows stones.
Microscopy
Mild cases: The inflammation is scanty and show lymphocytes, plasma cells, and macrophages in the mucosa and in the subserosal fibrous tissue.
Advanced cases: It shows marked subepithelial and subserosal fibrosis, associated with mononuclear cell infiltration.
B
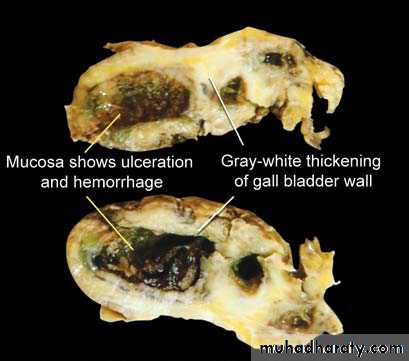
CHRONIC CHOLECYSTITIS : Grey white thikening of the blader wall with ulceration of the mucosa
Chronic cholecystitis
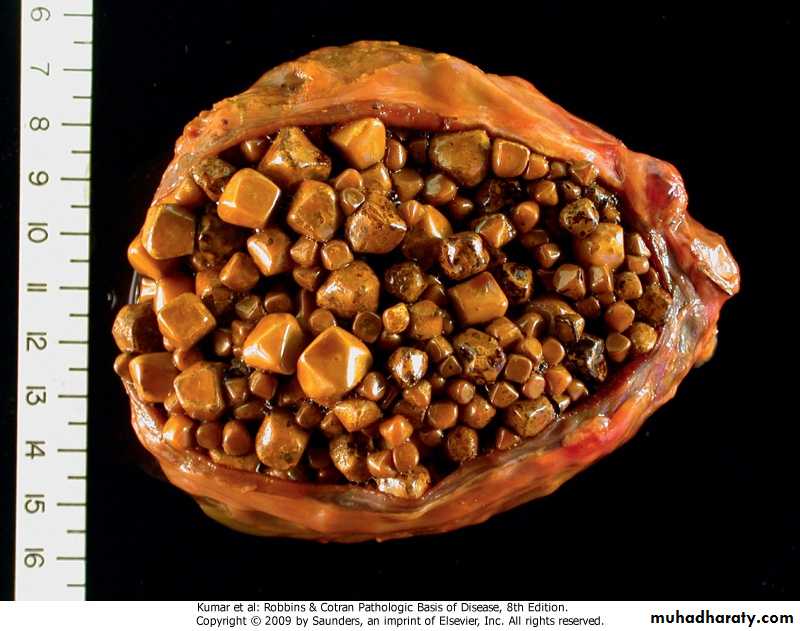
CHOLELITHIASIS (GALLSTONES)
Cholelithiasis is a common disorder and found in ~10 to 20% of adult populations in developed countries.Majority (> 80%) are “silent”.
Classification of Gallstones
Cholesterol GallstonesThey contain more than 90% of cholesterol + calcium bilirubinate + calcium carbonate.
Radiolucent.
Pigment Gallstones
They are composed of calcium bilirubinate + calcium carbonate + less than 20% of cholesterol.
Pigment stones are sub classified as:
– Black pigment stones (40%).
◆ patients with older age, chronic hemolytic states.
◆ arise in sterile gall bladder
◆ Contains 10 to 90% calcium bilirubinate + other calcium salts .
They have very low cholesterol concentration.
◆ 50 to 75% are radiopaque because of calcium salts.
– Brown pigment stones:
◆ They form in the bile duct and are associated with bile stasis and infections in the gallbladder and biliary tree. They are rare in the gallbladder.
◆ Usually radiolucent.
Risk factors for gallstones
CHOLESTEROL STONES1. Advancing age
2. Female sex hormones: Female, pregnancy, parity and oral contraceptives
3. Environmental factors: Drugs (ceftriaxone), obesity and metabolic syndrome, rapid weight reduction, diet high in calories and cholesterol.
4. Acquired disorders: Gallbladder stasis.
5. Genetic predisposition: Familial predisposition, inborn disorders of bile acid metabolism
6. Metabolic abnormalities: Diabetes, genetic hyperlipoproteinemias .
PIGMENT STONES
1. Chronic hemolysis
2. Chronic biliary tract infections
3. Gastrointestinal diseases: Ileal disease (e.g. Crohn disease), ileal resection or bypass, cystic fibrosis with pancreatic insufficiency
• Pathogenesis -cholesterol stones super-saturation of bile with bilirubin & cholesterol -pigment stones disorders associated with elevated levels of unconjugated bilirubin in bile.
Gall bladder, cholesterol stones(pale yellow, round to ovoid)
Gall bladder, pigment stones
clinical features -silent -biliary colic -complication in gall bladder (empyema,
perforation, fistulas, cholecystitis,carcinoma)
-cholangitis & cholestasis
-pancreatitis
-intestinal obstruction
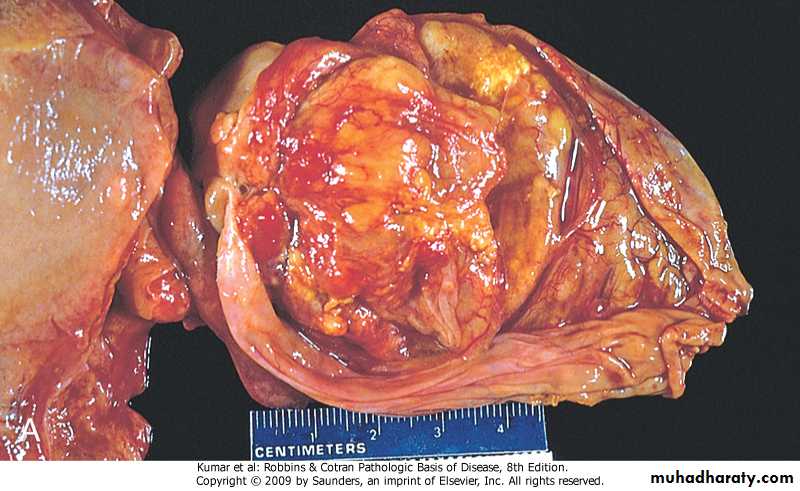
Tumors Of Gall Bladder
BENIGN TUMORS AND TUMOR-LIKE LESIONS- Adenoma- Inflammatory polyp- Adenomyosis
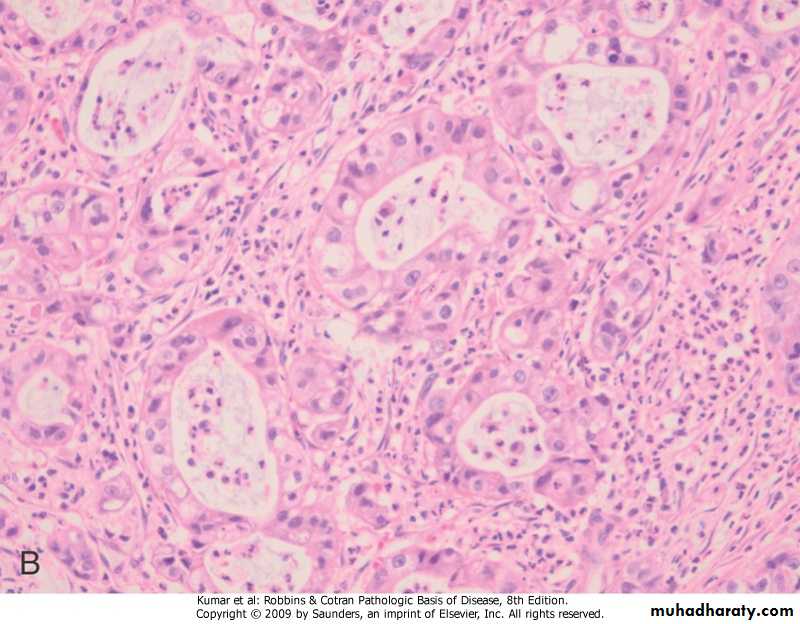
CARCINOMA OF THE GALLBLADDER- slightly more common in females- most frequently in the 7th decade of life - only rarely is surgically resectable - mean 5-year survival rate is about 1% Predisposing factors -stones -infection Morphology -grossly (infiltrative, exophytic) -microscopically (adenocarcinoma)Gall bladder, Adenocarcinoma
Gall bladder, Adenocarcinomawell-defined glandular and tubular structures lined by cuboidal to low columnar epithelial cells.
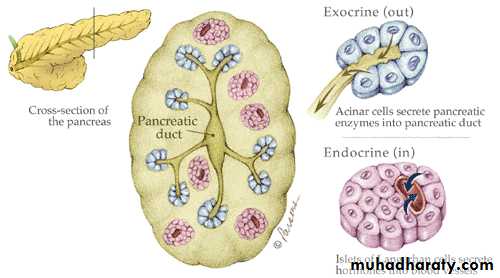
THE PANCREAS
Pancreas has 2 components: -Exocrine, (85% of the gland), produces 2-2.5 L of bicarbonate-rich fluid -Endocrine, (up to 2% of the gland), consists of 1 million clusters of islets of Langerhans, secrete insulin, glucagon & somatostatin
Pancreatic acini (exocrine pancreas)
Acute pancreatitis
Definition: acute inflammation of the exocrine pancreas due to injury to the parenchyma of the pancreas.-Acute pancreatitis is relatively common and reversible .
CausesMetabolic
Alcoholism
Hyperlipoproteinemia
Hypercalcemia.
Mechanical
Gallstones
Trauma -blunt abdominal trauma
Iatrogenic injury during surgery (e.g. endoscopic procedures with dye injection)
Drugs and toxins
Drugs: Furosemide, azathioprine
Toxins: Insecticides, methanol, organophosphates.
Vascular
Shock
Thrombosis and embolism
Infectious
Viral infections: Mumps, coxsackievirus.
Morphology
Morphologically, acute pancreatitis classified into :
• Interstitial
It is mild and reversible with interstitial edema and mild infiltration by polymorphonuclear leukocytes.
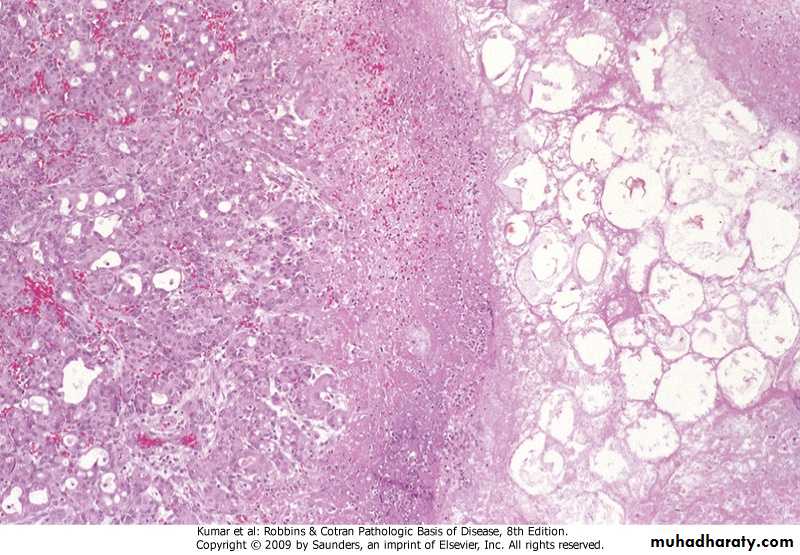
2. Necrotizing
Pancreas is enlarged and swollen, and shows red-black areas of hemorrhage with foci of yellow-white chalky fat necrosis
3. Hemorrhagic
Extensive hemorrhage and fat necrosis within the pancreatic parenchyma. In severe cases, marked hemorrhage may convert the pancreas into a large retroperitoneal hematoma.
• PathogenesisAutodigestion of the pancreatic by inappropriately activated pancreatic enzymes secondary to inappropriate activation of trypsinogen
Acute pancreatitis, hemorrhage & fat necrosis
Acute pancreatitis, fat & parenchymal necrosis
• Complications
Local complications• Sterile pancreatic abscess
•Pancreatic pseudocyst
• Infection by gram-negative organisms from the alimentary tract
Systemic complications
•Shock with acute renal tubular necrosis during the first week
•Acute respiratory distress syndrome
•Acute renal failure
•Hemolysis
•Disseminated intravascular coagulation (DIC)
•Diffuse fat necrosis
Chronic Pancreatitis
Definition: chronic inflammation of the pancreas characterized by the presence of permanent and progressive morphologic or functional damage to the pancreas.- Pancreas shows irreversible damage of exocrine parenchyma, and fibrosis.
• Causes -chronic alcohol abuse (most common) -obstruction of pancreatic duct -hereditary pancreatic enzymes abnormalities -cystic fibrosis -idiopathic (40%)• Pathogenesis -Direct toxic effects on acini (alcohol) -Oxidative stress (free radicals-alcohol) -Ductal obstruction by concretions
Morphology
GrossChronic pancreatitis can be subdivided into two major forms:
- Non-obstructive chronic pancreatitis
It is by far the most common form of chronic pancreatitis (~95%) and about 80% of the patients are alcoholics.
- Obstructive chronic pancreatitis
It is the result of narrowing or occlusion of the pancreatic ducts. It is most commonly due to carcinoma and stones in the ductal system.
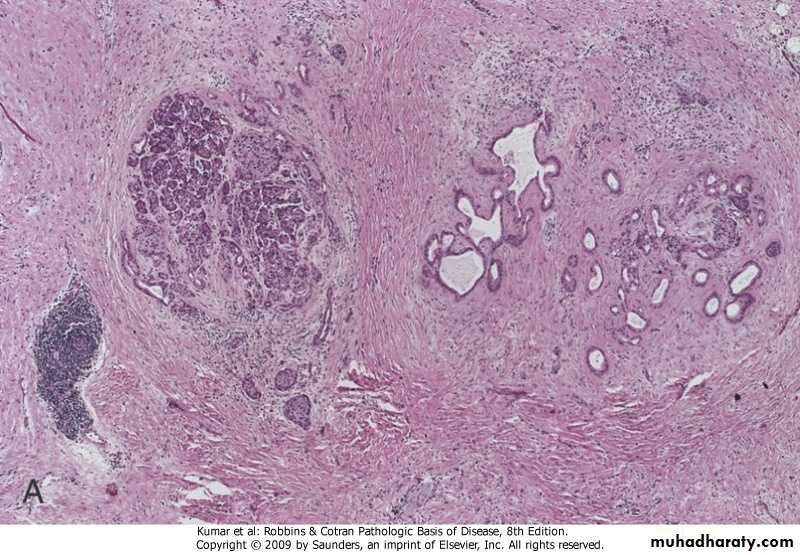
Microscopy
1. Parenchymal fibrosis2. Atrophy of acini
3. Dilation of the pancreatic ducts
4. Alterations in the duct epithelium: It shows atrophy/hyperplasia/squamous metaplasia.
5. Chronic inflammatory infiltrate.
Chronic pancreatitis, interstitial fibrosis with glandular atrophy
Chronic pancreatitis, dilated duct with inspissated eosinophilic concretions
• Clinical features -silent until pancreatic insufficiency & diabetes mellitus develop -repeated attacks of abdominal pain -recurrent attacks of jaundice or vague attacks of indigestion
PSEUDO-CYSTS- Account for 75% of pancreatic cysts- Secondary to acute or chronic pancreatitis, or abdominal injury- Usually solitary, embedded in peri- pancreatic tissue- Resolve, secondarily infected or perforate into adjacent structures
Pancreatic pseudocyst
Pancreatic pseudocyst, lined by granulation tissue
Pancreatic Neoplasms
Benign tumors :Benign tumors of the pancreas are rare.
Cytadenomatas are the main benign tumors of exocrine pancreas, they are painless, slowly growing tumor, multilocular.
mucin-secreting (benign mucinous cytadenoma)
serous –secreting (benign serous cyst adenoma).PANCREATIC CARCINOMAis the most frequent neoplasm of the pancreas (about 85% of all neoplasms)..has one of highest mortality rates of all cancers, 5-year survival of less than 5%.progression from non-neoplastic epithelium>noninvasive lesions in small ducts & ductules>invasive carcinoma (pancreatic intraepithelial neoplasias-PanINs), through multiple mutations
Epidemiology & pathogenesis - Risk factors:
Cigarette smoking and alcohol useConsumption of a diet rich in fats
Chronic pancreatitis
Diabetes mellitus
Inherited genetic defects:
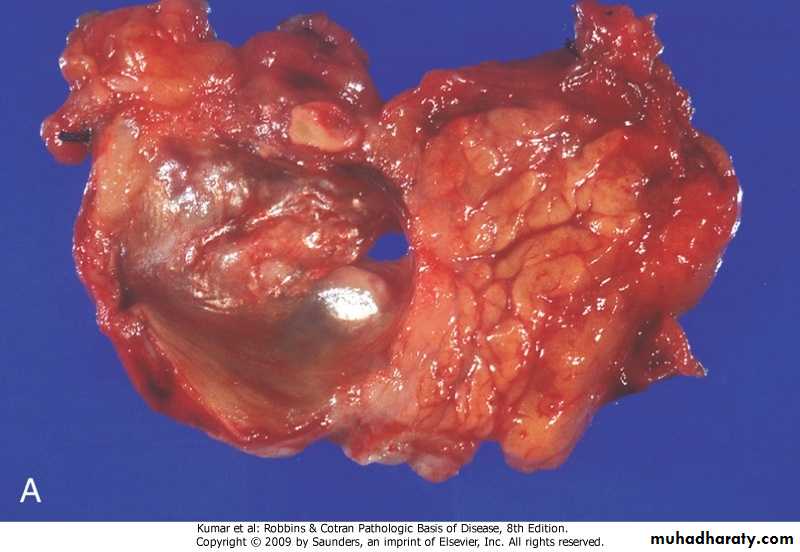
Morphology
About 60% in the head, 15% in the body, and 5% in the tail; in about 20% of cancers diffusely involve the entire pancreas.
• Gross
hard, stellate, gray-white, poorly delineated andfirm masses.
• Microscopy
Pancreatic ductal adenocarcinoma.
The malignant glands are poorly formed and are usually lined by pleomorphic cuboidal-to-columnar epithelial cells.
Clinical features -silent until local extension -obstructive jaundice -non-specific -migratory thrombophlebitis (Trousseau sign)