Infection
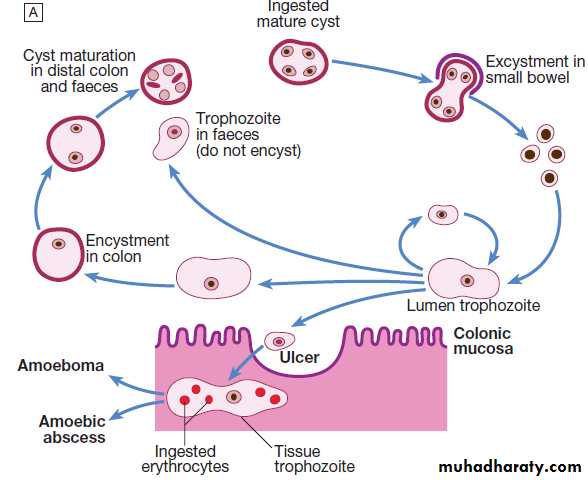
Amoebiasis is caused by Entamoeba histolytica, which is spread between humans by its cysts.
only E. histolytica causes amoebic dysentery or liver abscess
Pathology
Cysts of E. histolytica are ingested in water or uncooked foods contaminated by human faeces (feco-oral rout).In the colon, trophozoite forms emerge from the cysts.
The parasite may invade the mucous membrane of the large bowel, producing lesions that are maximal in the caecum (flask-shaped ulcers)/ may cause severe haemorrhage
S.T. A localised granuloma (amoeboma), presenting as a palpable mass in the rectum
DDX : colonic carcinoma.
Amoebic trophozoites can be carried to the liver in a portal venule. They can multiply rapidly and destroy the liver, causing an abscess.
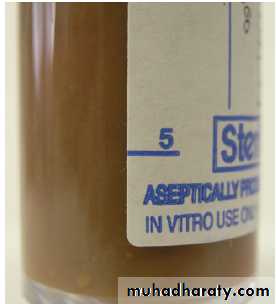
The liquid contents at first have a characteristic pinkish colour, which may later change to chocolate-brown (like anchovy sauce).
Cutaneous amoebiasis..rare
Clinical features
• Intestinal amoebiasis – amoebic dysenteryMost amoebic infections are asymptomatic. The incubation period (2 weeks to many years) , followed by a chronic course with abdominal pain and two or more unformed stools a day (Offensive diarrhoea alternating with constipation, and blood or mucus in the stool
A dysenteric presentation occurs particularly in older people or in the puerperium
DDX : bacillary dysentery or ulcerative colitis
• Amoebic liver abscess
usually found in the right hepatic lobe Early symptoms may be local discomfort; later, a swinging temperature and sweating may developAn enlarged, tender liver, cough and pain in the right shoulder are characteristic
A large abscess may penetrate the diaphragm and rupture into the lung (hepaticobronchial fistula)
Investigations
The stool and any exudate should be examined for motile trophozoites containing red blood cells.Sigmoidoscopy may reveal typical flask-shaped ulcers, which should be scraped and examined immediately for E. histolytica
An amoebic abscess of the liver: there is often a neutrophil leucocytosis and a raised right hemidiaphragm on chest X-ray/ultrasonic scanning. Aspirated pus ….. the characteristic anchovy sauce or chocolate-brown appearance
Serum antibodies are detectable by immunofluorescence in over 95%
Management
Intestinal and early hepatic amoebiasis responds quickly to oral metronidazole (800 mg 3 times daily for 5–10 days)
or other long-acting nitroimidazoles like tinidazole or ornidazole
Either diloxanide furoate or paromomycin, in doses of 500 mg orally 3 times daily for 10 days after treatment, should be given to eliminate luminal cysts.
If a liver abscess is large or threatens to burst, or if the response to chemotherapy is not prompt, aspiration is required and is repeated if necessary
Prevention
Personal precautions against contracting amoebiasis consist of not eating fresh, uncooked vegetables or drinking unclean water.
GiardiasisGiardia lamblia
common in the tropics. It particularly affects children, tourists and immunosuppressed individualsinfection usually occurs by ingesting contaminated water. Its flagellar trophozoite form attaches to the duodenal and jejunal mucosa, causing inflammation
Clinical features and investigations
incubation period of 1–3 weeks, there is diarrhoea, abdominal pain, weakness, anorexia, nausea and vomiting. On examination, there may be abdominal distension and tenderness.Stools obtained at 2–3-day intervals should be examined for cysts. Duodenal or jejunal aspiration by endoscopy gives a higher diagnostic yield.
Management
Treatment is with a single dose of tinidazole 2 g, metronidazole 400 mg 3 times daily for 10 days, or nitazoxanide 500 mg orally twice daily for 3 daysINFECTIONS CAUSED BY HELMINTHS
Intestinal human nematodes
There are two types:
• the hookworms, which have a soil stage in which they develop into larvae that then penetrate the host
• a group of nematodes which survive in the soil merely as eggs that have to be ingested for their life cycle to continue.
Ancylostomiasis (hookworm)
caused by parasitisation with Ancylostoma duodenaleThe adult hookworm is 1 cm long and lives in the duodenum and upper jejunum. Eggs are passed in the faeces.
In warm, moist, shady soil, the larvae develop, then penetrate human skin and are carried to the lungs.
After entering the alveoli, they ascend the bronchi, are swallowed and mature in the small intestine, reaching maturity 4–7 weeks after infection. The worms attach themselves to the mucosa of the small intestine and withdraw blood.
An allergic dermatitis, usually on the feet (ground itch), may be experienced at the time of infection.
The passage of the larvae through the lungs in a heavy infection causes a paroxysmal cough with blood-stained sputum, associated with patchy pulmonary consolidation and eosinophilia.
When the worms have reached the small intestine, vomiting and epigastric pain resembling peptic ulcer disease may occur
Anaemia with high-output cardiac failure may result.
Investigations
Eosinophilia, anaemiafaecal occult blood testing will be positive and many ova will be present
Management
A single dose of albendazole (400 mg) is the treatment of choice
Alternatively, mebendazole 100 mg twice daily for 3 days may be used
oral iron
Strongyloidiasis
parasitises the mucosa of the upper part of the small intestine, causing persistent eosinophilia.
The classic triad of symptoms consists of abdominal pain, diarrhoea and urticaria
occurs in association with immune suppression
Systemic (super)infection:pneumonia, meningoencephalitis, death
Investigations
eosinophilia. Serology (ELISA) is helpful butdefinitive diagnosis depends upon finding the larvae in the faeces or juj. Aspiration
Management
A course of two doses of ivermectin
Alternatively, albendazole is given
(roundworm) Ascaris lumbricoides
Humans are infected by eating food contaminated with mature ova. Ascaris larvae hatch in the duodenum, migrate through the lungs, ascend the bronchial tree, are swallowed and mature in the small intestine.Clinical features
local and general hypersensitivity reactions, with pneumonitis, eosinophilic granulomas, bronchial asthma and urticariaIntestinal ascariasis causes symptoms ranging from occasional vague abdominal pain through to malnutrition.
obstructive complications in intestine /blockage of the bile or pancreatic duct
Investigations
The diagnosis is made microscopically by finding ova in the faeces
Eosinophilia
Management
A single dose of albendazole (400 mg), pyrantel pamoate , ivermectin or mebendazole is effective for intestinal ascariasis.
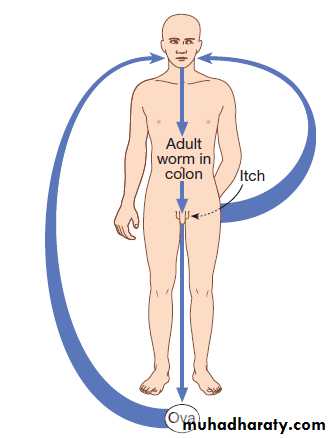
Enterobius vermicularis
This helminth is common throughout the world and affects mainly children.After the ova are swallowed, development takes place in the small intestine, but the adult worms are found chiefly in the colon.
Clinical features
The gravid female worm lays ova around the anus, causing intense itching, especially at night.The ova are often carried to the mouth on the fingers and so re-infection or human-to-human infection takes place
Investigations
Ova are detected by applying the adhesive surface of cellophane tape to the perianal skin in the morning. This is then examinedManagement
A single dose of mebendazole (100 mg), albendazole (400 mg), pyrantel pamoate or piperazine is given and may be repeated after 2 weeks to control auto-reinfection.
If infection recurs in a family, each member should be treated as above. During this period all nightclothes and bed linen are laundered
Tissue-dwelling human nematodes
Lymphatic filariasis
W. bancrofti is transmitted by night-biting culicine or anopheline mosquitoes in most areas
The adult worms, 4–10 cm in length, live in the lymphatics
Toxins released by the adult worm cause lymphangiectasia; this dilatation of the lymphatic vessels leads to lymphatic dysfunction and the chronic clinical manifestations of lymphatic filariasis, lymphoedema and hydrocele.
Clinical features
Acute filarial lymphangitis presents with fever, pain, tenderness and erythema along the course of inflamed lymphatic vesselsInflammation of the spermatic cord, epididymis and testis is common
Progressive enlargement,coarsening, fissuring and bacterial infection of the skin and subcutaneous tissue develop gradually, causing irreversible ‘elephantiasis’.
Investigations
In the earliest stages of lymphangitis, the diagnosis is made on clinical grounds, supported by eosinophiliaMicrofilariae can be found in the peripheral blood at night, and either are seen moving in a wet blood film or are detected by microfiltration
Indirect fluorescence and ELISA detect antibodies in over 95%
Management
Treatment of the individual is aimed at reversing and halting disease progression. Diethylcarbamazine orally 3 times daily for 12 days, or as a single dose) kills microfilariae and adult wormsAntihistamines or corticosteroids may be required to control these allergic phenomena.