CHRONIC
PERIODONTITIS
dr . Hussein AL dabbgh
CONTENT
Periodontal disease
Classification
Introduction
Definition
Major clinical and etiologic factor
Prevalence
Clinical features
Symptoms
Types
Disease severity
Disease progression
Clinical diagnosis
Radiographic features
Risk factors for disease
Treatment
Prognosis

Periodontal disease
Definition:
Periodontal disease comprises of a group of
inflammatory condtions of the supportive tissues
of the teeth that are caused by bacteria.
-Carranza

The Periodontal Disease Classification System of the
American Academy of Periodontology (AAP), 1999
I
.
Gingival Diseases
A. Dental plaque-induced gingival diseases
B. Non-plaque-induced gingival lesions
II. Chronic Periodontitis (slight: 1-2 mm CAL; moderate: 3-4 mm CAL;
severe: > 5 mm CAL)
A. Localized ( < 30% of sites are involved)
B. Generalized (> 30% of sites are involved)
III. Aggressive Periodontitis
A. Localized ( < 30% of sites are involved)
B. Generalized (> 30% of sites are involved)
IV. Periodontitis as a Manifestation of Systemic Diseases
A. Associated with hematological disorders
B. Associated with genetic disorders
C. Not otherwise specified
.
V. Necrotizing Periodontal Diseases
A. Necrotizing ulcerative gingivitis
B. Necrotizing ulcerative periodontitis
VI. Abscesses of the Periodontium
A. Gingival abscess
B. Periodontal abscess
C. Pericoronal abscess
VII. Periodontitis Associated With Endodontic Lesions
A. Combined periodontic-endodontic lesions
VIII. Developmental or Acquired Deformities and
Conditions
A. Localized tooth-related factors that modify or
predispose to plaque-induced gingival
diseases/periodontitis
B. Mucogingival deformities and conditions around
teeth
C .Mucogingival deformities and conditions on
edentulous ridges
D. Occlusal trauma

INTRODUCTION
Chronic periodontitis, formerly known as
adult
periodontitis
or
chronic adult periodontitis
, is the
most prevalent form of periodontitis.
It is generally considered to be a
slowly
progressing disease
.
Although chronic periodontitis is most frequently
observed in adults, it can occur in children and
adolescents in response to chronic plaque and
calculus accumulation.
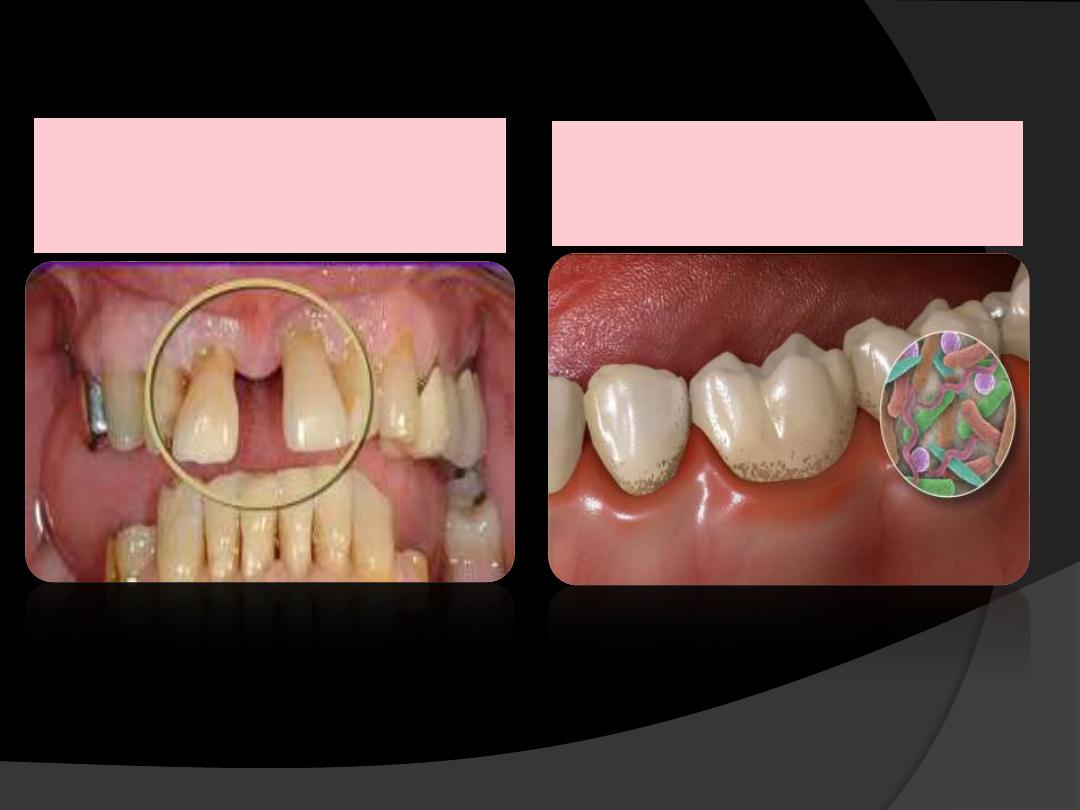
DEFINITION
Chronic periodontitis has been defined
as “
an infectious disease resulting in
inflammation with in supporting tissues
of the teeth, progressive attachment loss
and bone loss
”.
Major clinical and etiologic
characteristics of the disease
:
1.
Microbial plaque formation.
2.
Periodontal inflammation, and
3.
Loss of attachment and alveolar bone.

PREVALENCE
Effects
both sexes
equally.
Increases with
age
.
Age associated disease
not age related and
occurs depending on disease duration.

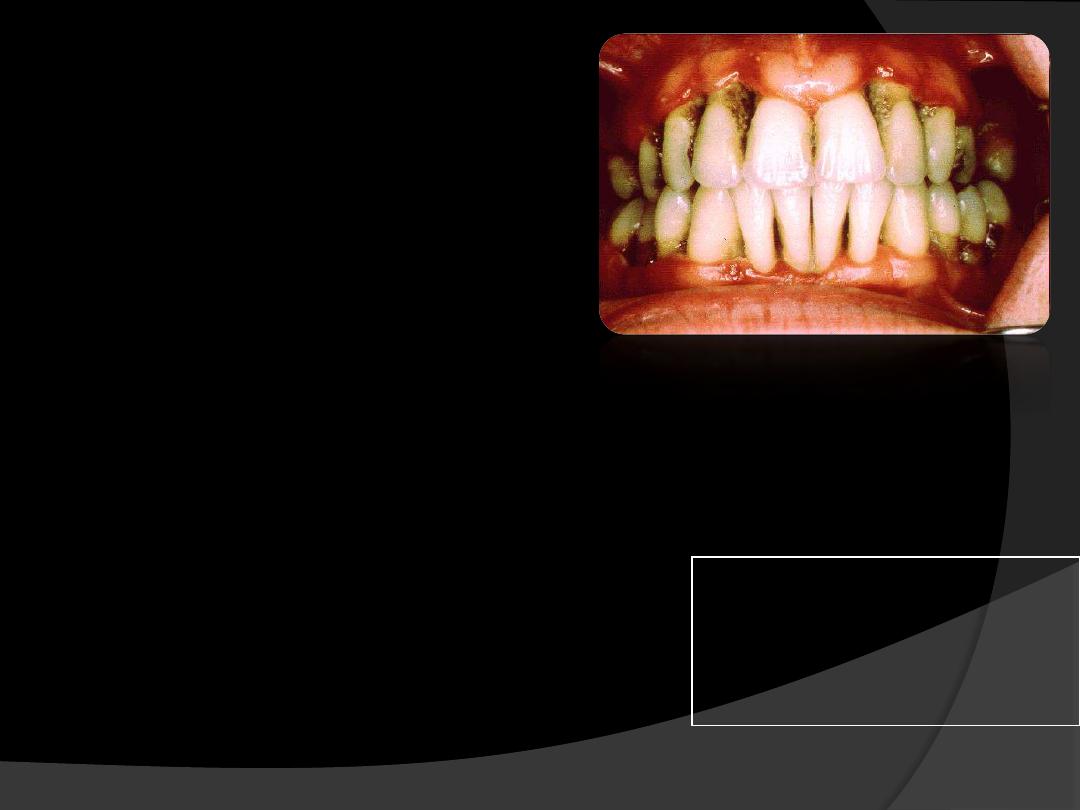
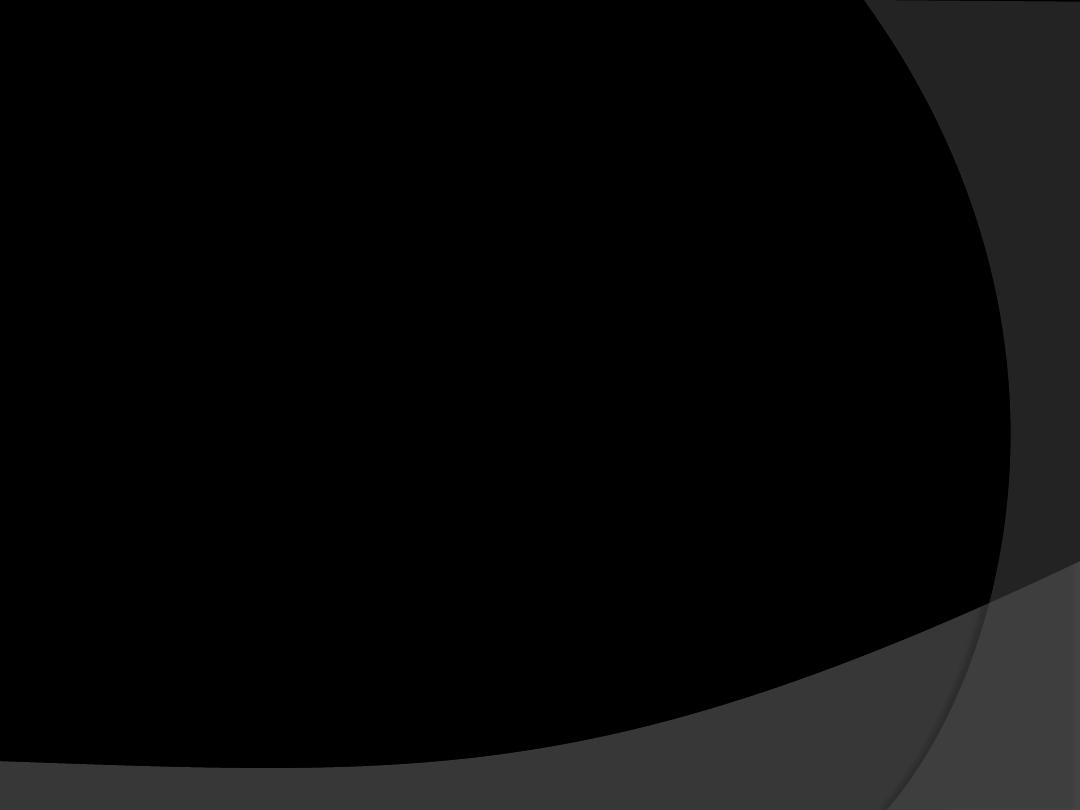
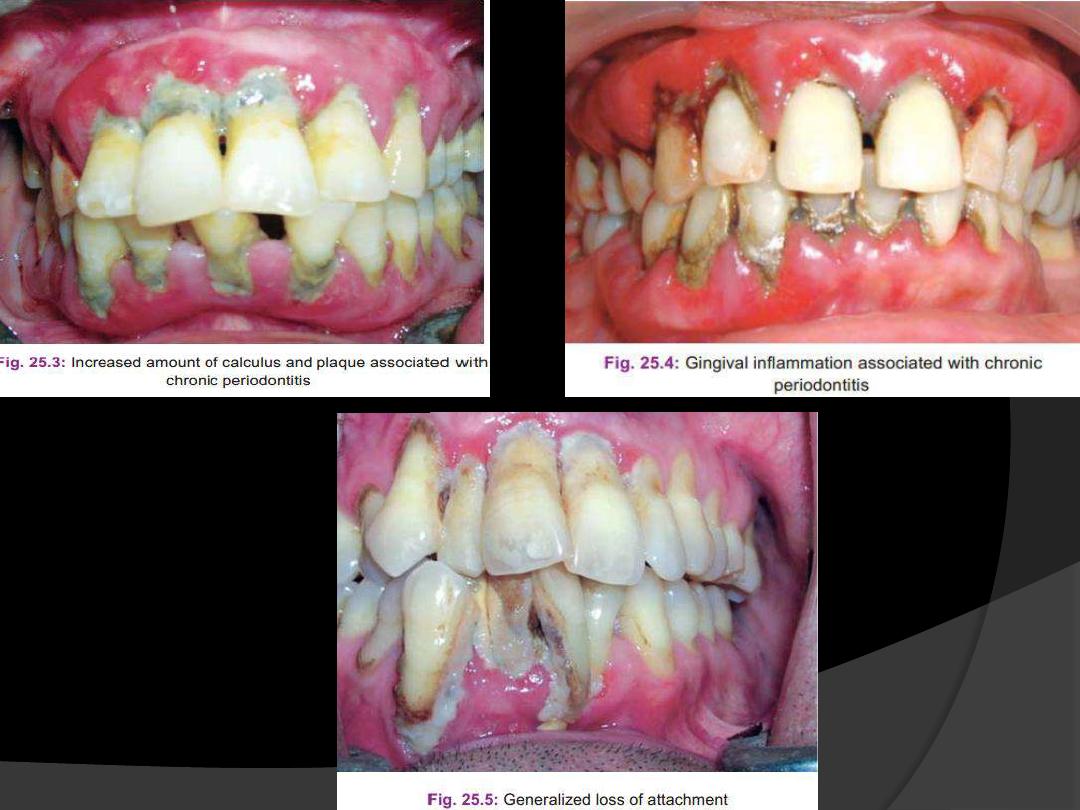
CLINICAL FEATURES
Most prevalent in adults but can occur
in children and adolescents.(age‐35+yrs)
Supragingival and subgingival plaque
accumulation (frequently associated with
calculus)
Gingival inflammation
Pocket formation
Loss of periodontal attachment
Occasional suppuration
Poor oral hygiene – gingiva is typically
may be slightly to moderately swollen
.
Color-
pale red to magenta
Consistency –
soft or firm
Surface topography –
loss of
stippling
Blunted or rolled gingival margin
Flattened or cratered papillae.
Tooth mobility.
Furcation involvement.
Spontaneous gingival bleeding.
Pocket depths are variable and
both
suprabony and intrabony
pockets
can be found.

Attachment loss with and without deep
periodontal pocket.
Pocket depths
are variable, and both horizontal
and vertical bone loss can be found.
Furcation involvement
in the molars
are common in advance cases of
chronic periodontitis.
Tooth mobility
often appears in
advanced cases when bone loss has
been considerable.

SYMPTOMS
Bleeding gums during brushing or eating
Increasing spacing between teeth as a result of tooth movement
Loose teeth
Usually painless, but sometimes localized dull pain radiating deep
into the jaw
Sensitivity to heat, cold, or both due to exposed roots
Food impaction
Halitosis
Gingival tenderness or itching
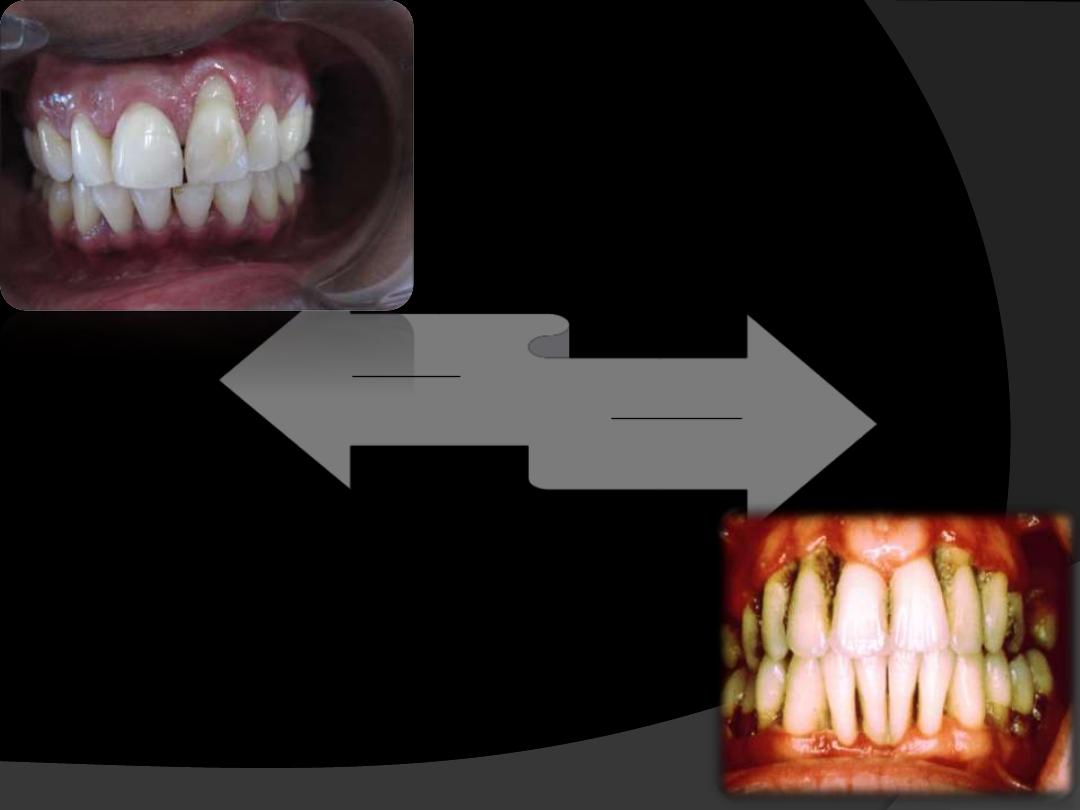
TYPES
DISEASE DISTRIBUTION
Chronic periodontitis is considered to be as
“site
specific disease”
Inflammation, pockets, attachment loss and bone
loss
are due to direct site-specific effects of
sub-
gingival plaque
accumulation as a result of this
local effect, attachment loss and pockets may
occur.
It may occur on
one surface of the tooth while the
other surface remain normal.
In addition to being site specific, chronic
periodontitis may be described as:
Localized:
Periodontitis is considered localized when
<30% of the
sites
assessed in oral cavity demonstrate
attachment loss
and bone loss.
Generalized
:
Periodontitis is considered generalized when
>30% of
the sites
assessed demonstrate attachment loss and bone
loss.
The pattern of bone loss in chronic periodontitis can be
vertical or horizontal.
.
Localized-
less than 30%sites
are involved
Generalized-
When 30% or more sites
shows CAL & bone loss
• Localized ≤ 30% of the sites are affected
•Generalized > 30% of the sites are affected
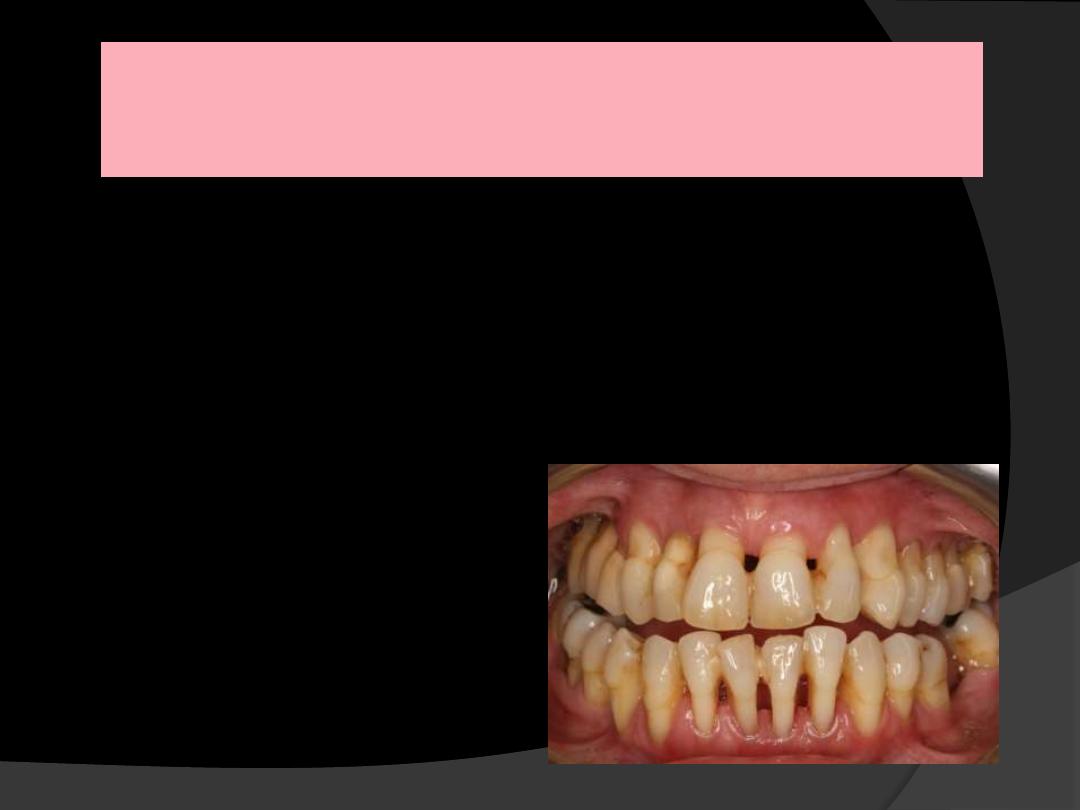
MILD PERIODONTITIS
1 to 2 mm CAL
MODERATE PERIODONTITIS
3 to 4 mm CAL
SEVERE PERIODONTITIS
≥ 5 mm CAL
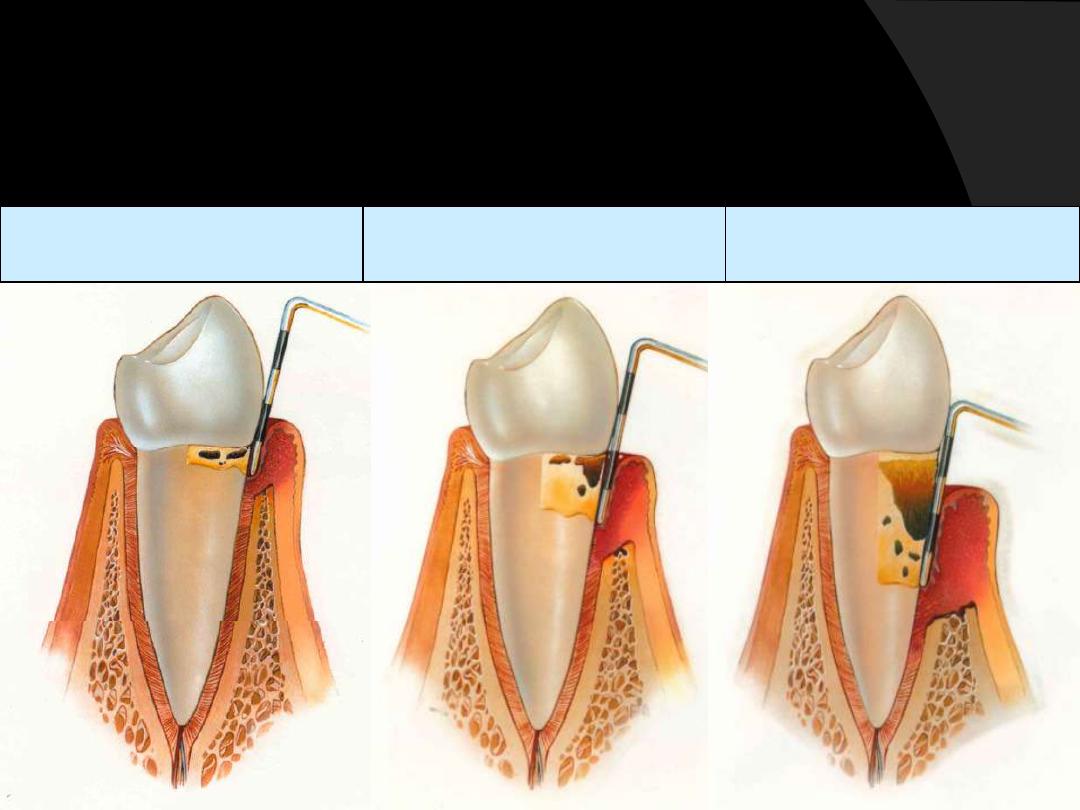
DISEASE SEVERITY
Severity can be categorized on the basis of the amount of
Clinical
attachment loss (CAL)
as follows
:

EARLY PERIODONTITIS
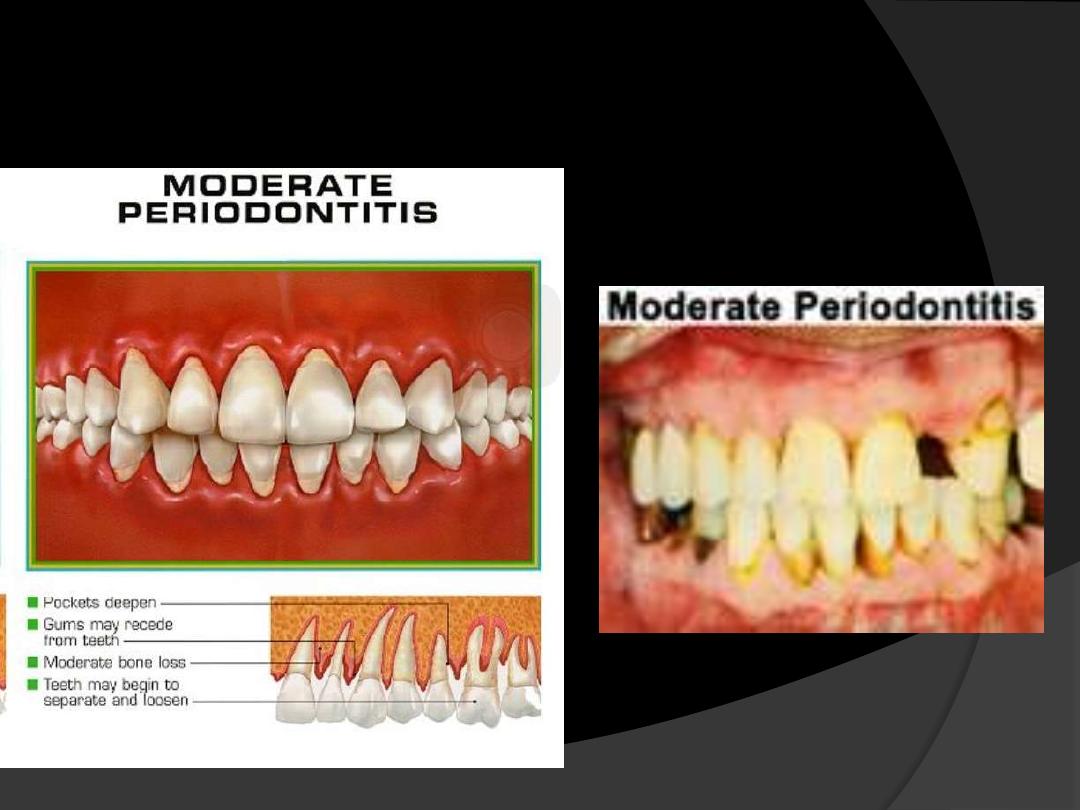
MODERATE
PERIODONTITIS
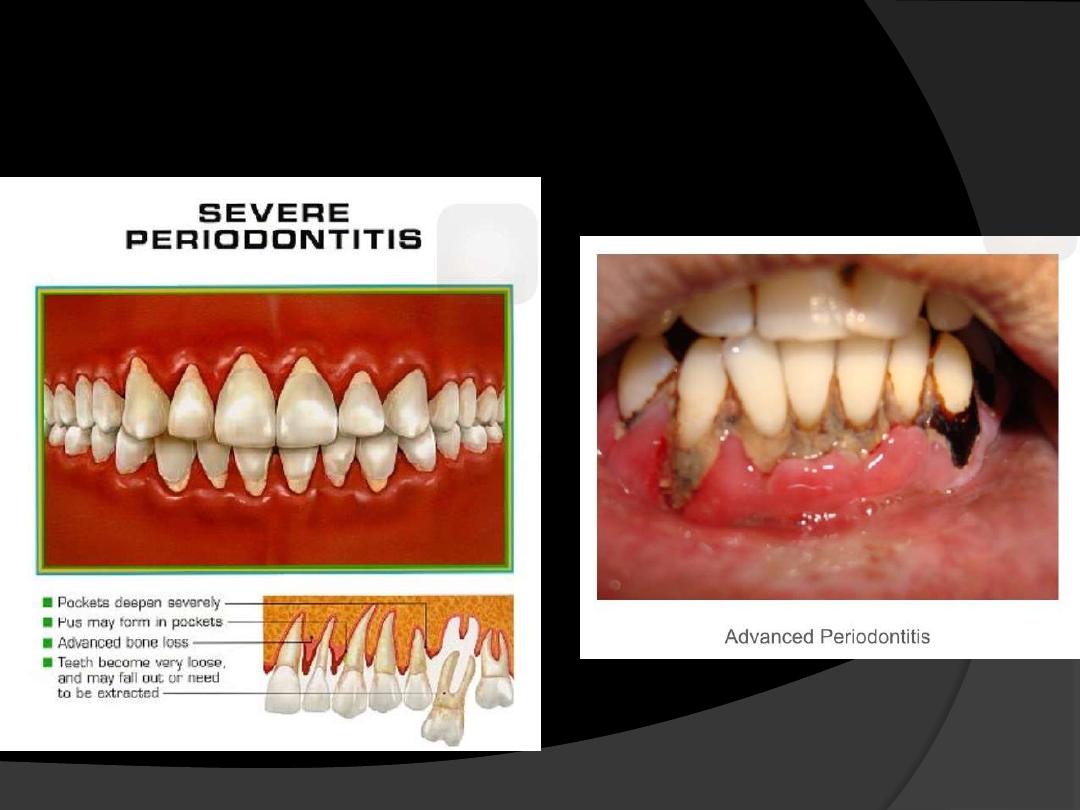
SEVERE
PERIODONTITIS

DISEASE PROGRESSION
The
rate of disease progression is usually slow
but
may be modified by systemic and/or environmental
and behavioral factors.
Chronic periodontitis does not progress at an equal
rate in all affected sites throughout the mouth.
More rapidly progressive lesions occur:
1.
Interproximal areas
2.
Areas of greater plaque accumulation
3.
Inaccessibility to plaque control measures
(e.g., furcation areas, overhanging margins, sites of
malposed teeth, or areas of food impaction)
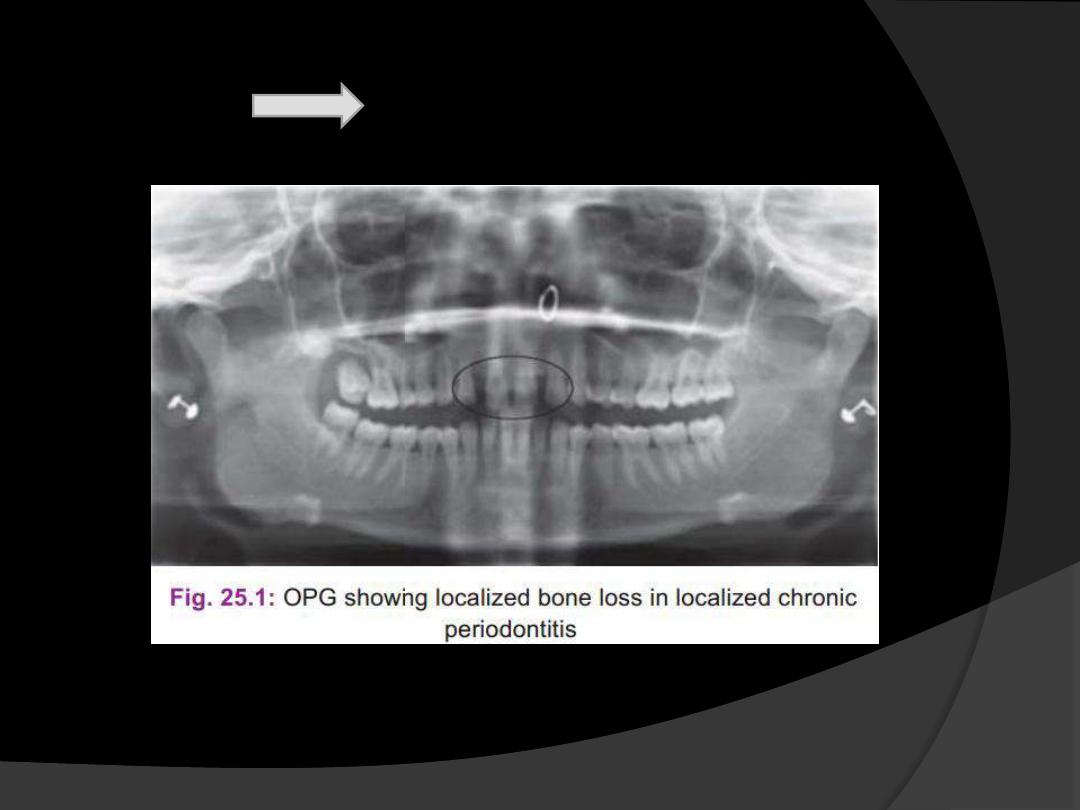
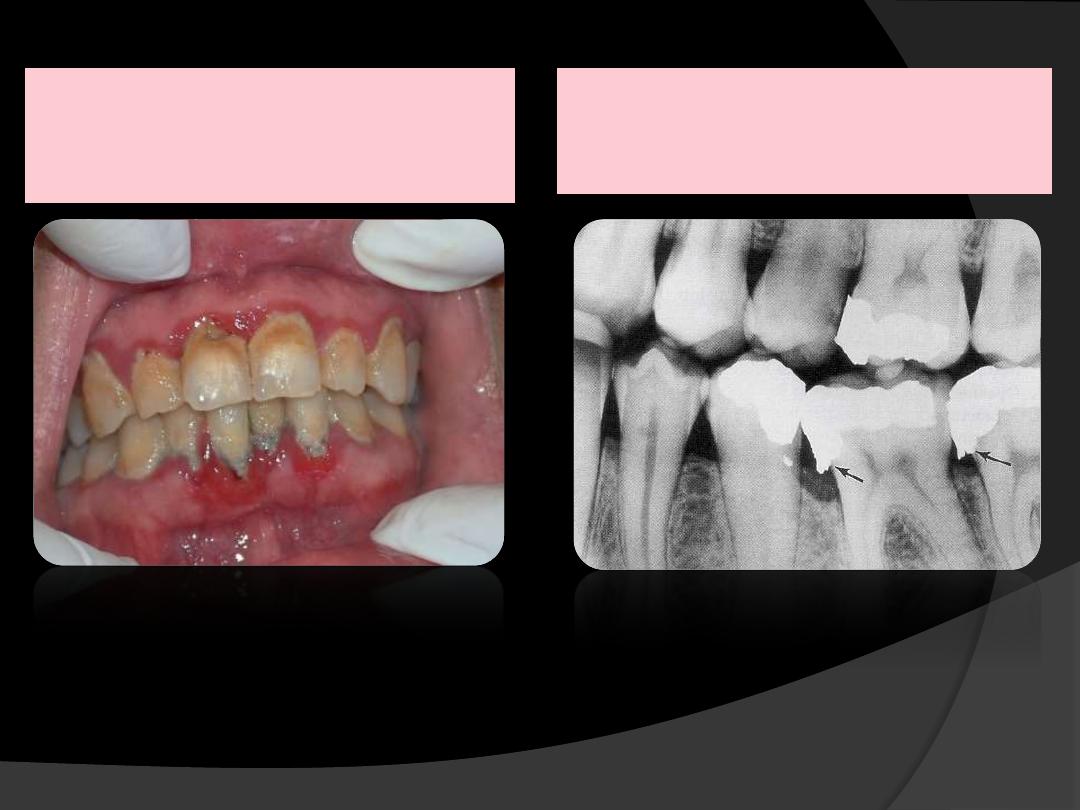
Clinical Diagnosis
Inflammation of the marginal gingiva
extent to the attached gingiva.
Clinical attachment loss.
Radiographs(in case of bone loss).

Widening of PDL space
Loss of corticated interdental crestal margin
Localised or generalized loss of alveolar supporting bone.
Blunting of the alveolar crest due to beginning of bone resorption
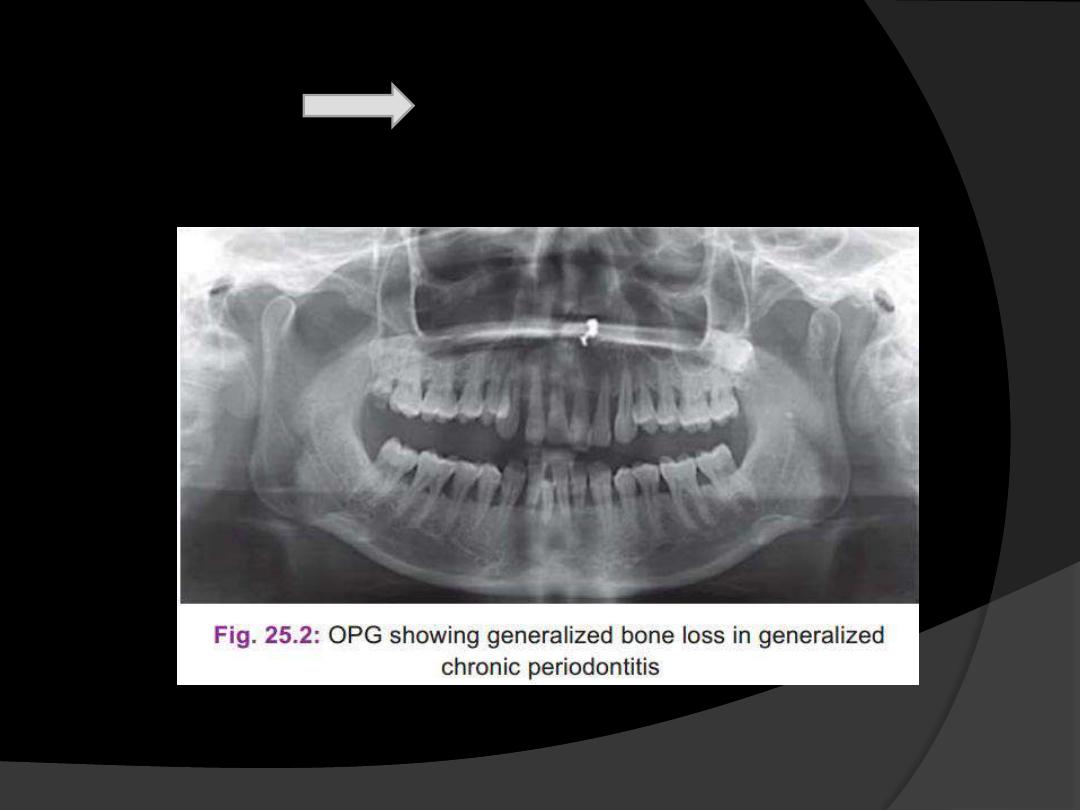
RADIOGRAPHIC
FEATURES
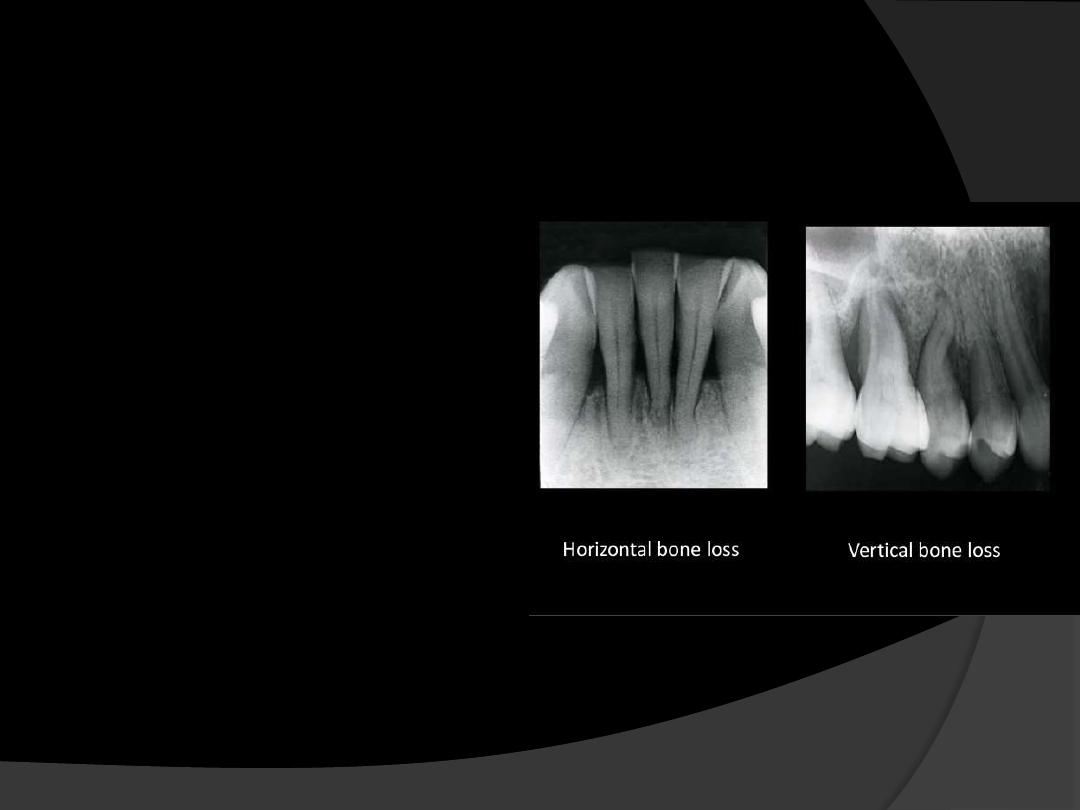
RADIOGRAPHIC
FEATURES
Pattern of bone loss
may
be
:
Vertical,
Horizontal,
Vertical bone loss is
usually associated with
intra bony pocket
formation.
Horizontal bone loss is
usually associated with
supra bony pockets.
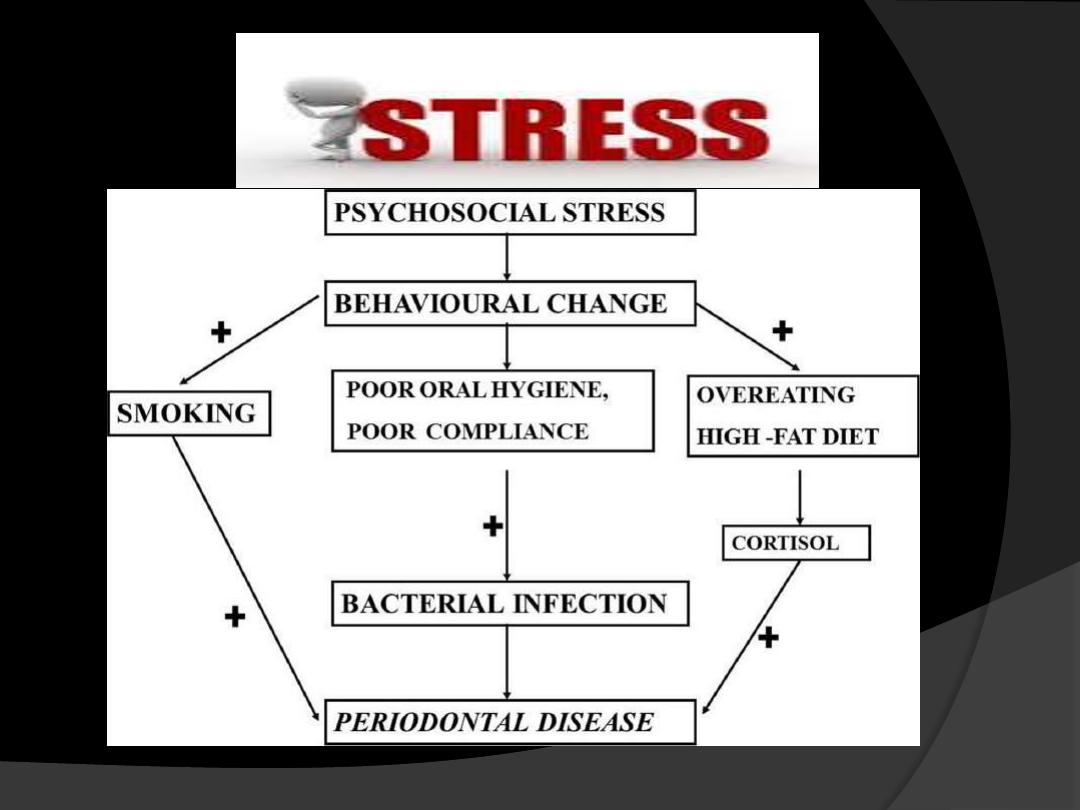
RISK FACTORS FOR DISEASE
•Prior History of Periodontitis
•Local Factors
•Systemic Factors
•Environmental and Behavioral Factors
•Genetic Factors
Risk factor - is a characteristic, an aspect of behavior, or an environmental
exposure that is associated with destructive periodontitis
Prior History Of Periodontitis
Although not a true risk factor for disease but rather a
disease
predictor
, a prior history of periodontitis puts
patients at greater risk for developing further loss of
attachment and bone, given a challenge from bacterial
plaque accumulation.
Patient present with persistent gingivitis or
periodontitis with pocketing, attachment loss, and
bone loss ,may continue to lose periodontal support if
not successfully treated.
LOCAL FACTORS
Plaque and plaque retentive factors.
Microbiological Factors
Causative organisms of chronic periodontitis are:
•
Porphyromonas gingivalis
(P. gingivalis)
•
Prevotella intermedia
(P. intermedia)
•
Treponema denticola
• Capnocytophaga
• A.actinomycetemcomitans
(A.a)
•
Eikenella corrodens
(E. corrodens)
•
Campylobacter rectus
(C. rectus)
Viruses including
cytomegalo , Epstein Barr, Papilloma and
herpes simplex
have been proposed to play a role in the
etiology of periodontal diseases, possibly by changing the host
response to the local subgingival microbiota.
LOCAL FACTORS
Plaque Accumulation
Oral Hygiene
Tooth Malposition
Restoration
Preserve & Quantity of certain bacteria
Host defences
Subgingival Restoration
Environment
Calculus, smoking
Connective Tissue destruction
Genetic influence
Inflammation
Periodontopathic bacteria
Smoking, Calculus
Loss of Attachment
M
O
D
I
F
Y
I
N
G
F
A
C
T
O
R
S
Plaque retentive factors:
Calculus
Overhanging
restorations
Trauma from occlusion
Micro-organisms
SYSTEMIC FACTORS
Non Genetic
-Smoking is a major risk factor
- Diabetes
-Conditions associated with compromised immune
responses (e.g. HIV)
- Nutritional defects
-Osteoporosis
-Medications that cause drug induced gingival
overgrowth (e.g. some calcium channel blockers,
phenytoin, cyclosporine)
Genetic factors
(as yet poorly defined)
SMOKING
•
Undoubtedly one of the main and most prevalent,
risk
factors
for
chronic
periodontitis,
risk
calculations suggesting
40%
of the cases of chronic
periodontitis may be
attributable to smoking.
•
It has been estimated that there are 1.1 billlion are
smokers worldwide and
182 million (16.6%) of them
live in India
.
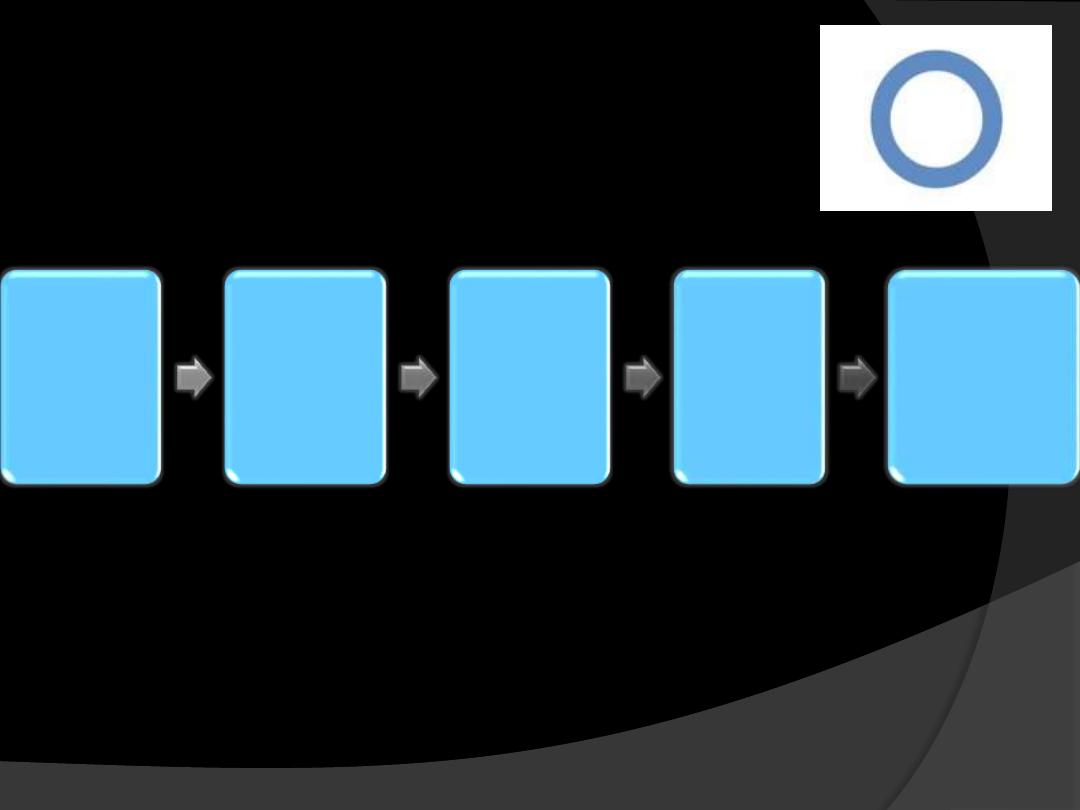
DIABETES
Hyperglyc
emia +
collagen
AGEs
Increases
cross
linking
between
collagen
molecules
Reduced
solubility
and
turnover
of
collagen
Failure in
periodontal
repair and
regeneration
.
AGE
Both the prevalence and severity of
periodontal disease
increases
with age.
Intake of medications,
Decreased immune function, and
Altered nutritional status interaction
NUTRITION
Vitamin C or ascorbic acid
is essential for the
formation of collagen and intercellular material,
bone and teeth.
↓ phagocytic function of neutrophils and
macrophages
↓ antibody response
↓ cytotoxic T-cell activity
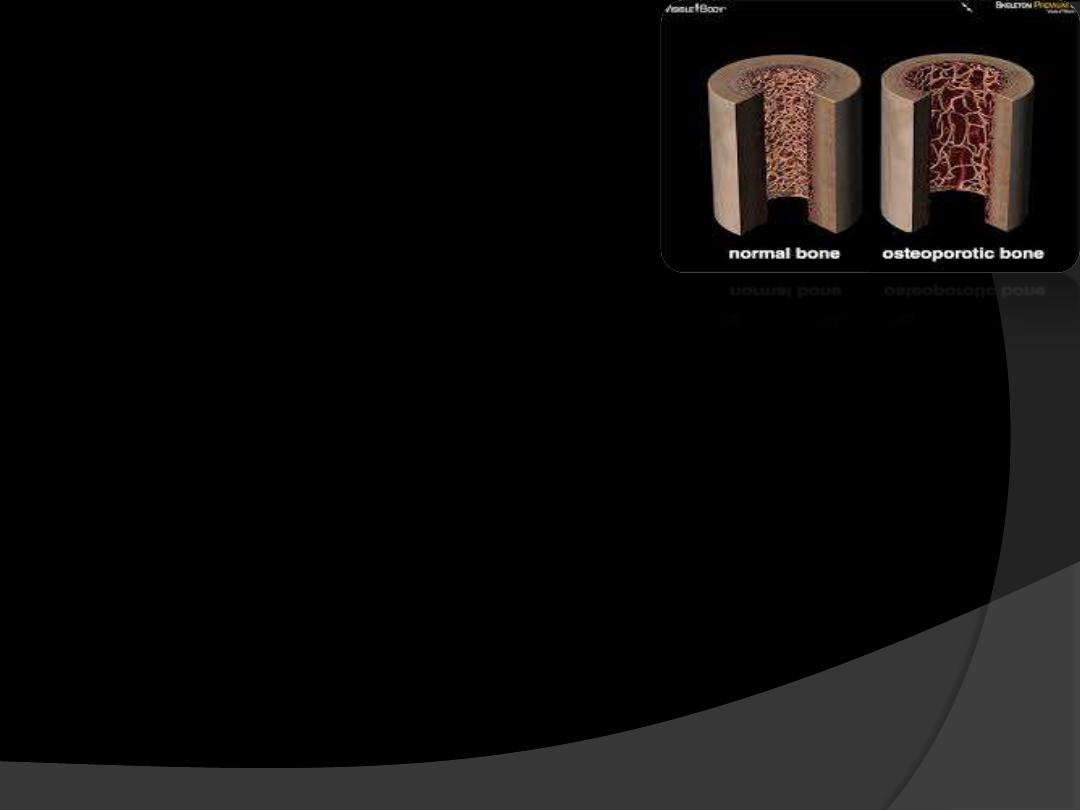
OSTEOPOROSIS
It is a disease characterized by low bone mass and deterioration of bone
structure that causes bone fragility and increases the risk of fracture.
Both osteoporosis and periodontal diseases are bone resorptive diseases
Osteoporosis could be a risk factor for the progression of chronic
periodontal disease.
A
direct association between skeletal and periodontal disease
as
measured by loss of
interproximal alveolar bone
in postmenopausal
women has been reported.

HIV
AIDS epidemics in US suggests HIV positive
patients especially those with AIDS and low
count of
T Lymphocytes(CD4 <200 cells/ml)
were at increased risk of chronic periodontitis.
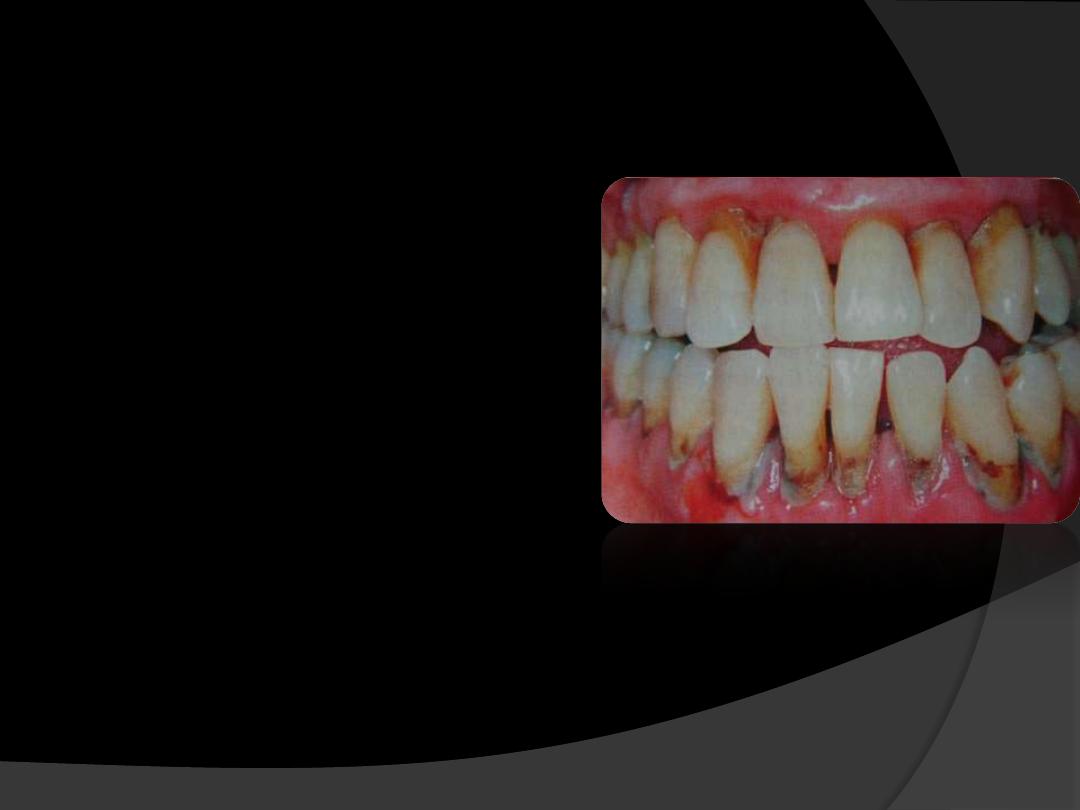
TREATMENT
1.
NON SURGICAL THERAPY
Initial therapy ( scaling and root planing)
Antimicrobial therapy – as an adjunct to routine
periodontal therapy.
Improvement in oral hygiene.
Instruction, reinforcement, evaluation of plaque
control records.
Removal of all the factors contributing to plaque
accumulation, e.g. correction of ill-fitting
appliances, overcontoured crowns, overhanging
restorations, etc.
2. SURGICAL THERAPY
A variety of surgical treatment modalities may be
appropriate in managing the patient.
1. Pocket elimination procedures.
2. Regenerative therapy:
A. Bone replacement grafts;
B. Guided tissue regeneration;
C. Combined regenerative techniques.
3. Resective therapy:
A. Flaps with or without osseous surgery;
B. Gingivectomy.
PROGNOSIS
Slight to moderate periodontitis
, the
prognosis is
usually good
provided , the inflammation can be
controlled through good oral hygiene and the
removal of local plaque retentive factors.
In patients with more
severe disease
, as
evidenced by furcation involvements and
increasing mobility, or in patients who are
noncompliant with oral hygiene practices, the
prognosis may be downgraded from
fair to poor
.

