Dermatosis Resulting from Physical Factors
-Heat Injuries.-Cold injuries.
-Light injuries.
1
Heat Injuries.
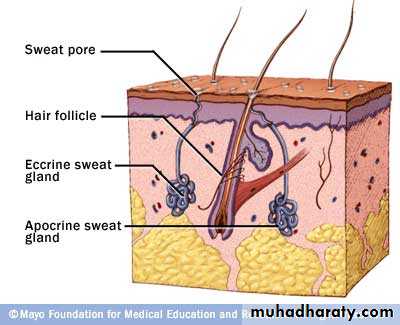
MiliariaOcclusion of eccrine sweat gland--- backed-up pressure-- rupture of sweat gland or duct--- Escape of sweat into adjacent tissue produces miliaria---- Different forms of miliaria --- depending on the level of injury to the sweat gland.
Common in hot, humid climates.
2
• Miliaria crystalina:
Small, clear, superficial vesicles without inflammation (like dewdrop). Lesions are asymptomatic Appears in bedridden patients Self-limited; no treatment is required.3
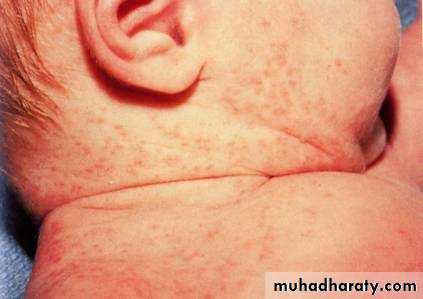
2. Miliaria rubra:
Discrete, extremely pruritic, erythematous papulovesicles.Site of injury is prickle cell layer.
The sites: antecubital and popliteal fossae, trunk, inframammary area, abdomen (at the waistline), and inguinal regions.
4
3. Miliaria pustulosa:
Always preceded by some injury, destruction, or blocking of sweat duct.Pustules are independent of hair follicle and sterile.
Seen in intertriginous areas, flexure surfaces of extremities, scrotum.
5
4. Miliaria profunda:
Nonpruritic, flesh-colored, deep-seated, whitish papulesConcentrated on the trunk and extremities.
Occlusion is in the upper dermis
6
Erythema Ab Igne “toasted skin” syndrome:
Reticulated erythema, leaving pigmentation.Produced by long-continued exposure to excessive heat with
7
Cold Injuries
Diseases of cold exposure (normal reaction to abnormal cold)1)Frostbite
2)Trench foot (Immersion foot):
89
Frostbite:
Soft tissue is frozen and locally reduction of blood supply.
Frozen part is painless and becomes pale and waxy.
Site: toes, feet, fingers, ears, nose and cheeks.
Trench Foot
It was exist in World War I, Now mostly among homeless.Results from prolonged exposure to cold, wet conditions.
Affected legs and feet are cold and anaesthetic. There is erythema, oedema, tenderness.
Tx-removal from environment
10
11
Diseases of abnormal susceptibility to cold (abnormal reaction to normal cold)
1)Chilblains(Pernio or Perniosis):
Are terms used to describe localized inflammatory lesions on acral skin, as an abnormal reaction to cold in susceptible individuals.Aetiology: Genetic, Poor nutrition, anorexia nervosa, systemic disease (lupus erythematosus, and haematological malignancy).
There is pain, itching, or burning on rewarming, caused by arteriolar and venular constriction.
Treatment; *Calcium channel blockers;Nifedipine 20mg (3 times\day). vasodilators {nicotinamide 100 mg (3 times\day) or dipyridamole 25 mg (3 times\day),pentoxifylline}. *Smoking forbidden.
12
13
14
It is a persistent blue discoloration of the entire hand or foot worsened by cold exposure.
2) Acrocyanosis
• It may be idiopathic or secondary to a number of systemic disorders: connective tissue disorders; neoplastic diseases; anorexia nervosa; orthostatic disorders; neurologic disorders).• Acrocyanosis is distinguished from Raynaud syndrome by its persistent nature (as opposed to the episodic nature of Raynaud), and lack of tissue damage (ulceration, distal finger tip resorption).
15
Acrocyanosis
persistent blue discoloration16
3) Erthrocyanosis
• It is a persistent, dusky erythema occurring at sites with a thick layer of underlying subcutaneous fat, such as thighs and lower legs.
17
4) Livedo reticularis
• It is a mottled, cyanotic discoloration of the skin, which has a characteristic network pattern. Most commonly occurs on the extremities, especially the legs.
• It may be physiological, idiopathic or secondary {occlusive diseases, arthritis (SLE, Dermatomyositis); infections (TB, Syphilis, Hepatitis)}
18
• 5) Raynaud Phenomenon:
• Raynaud Phenomenon----connective tissue disease (most common with scleroderma) and the term Raynaud’s disease--- absence of other conditions.
• There are three stages during a single episode: pallor (white), due to vasospasm; cyanosis (blue), due to relaxation of vasospasm; and hyperemia (red) in which relaxation results in reactive hyperemia and the fingers turn red.
19
6) Cryoglobulinemia
• Presence of immunoglobulin complexes which precipitate in vitro when cooled below body temperatures. The most usual skin manifestation is purpura on the lower legs.
7) Cold urticarial.
8) Cold erythema.
9) Cold panniculitis
10) Neonatal cold injury
Light InjuryParts of solar spectrum important to photomedicine:
*Visible light 400 to 760 nm, has little biologic activity, except for stimulating the retina
*Infrared radiation beyond 760 nm, experienced as radiant heat.
*Below 400 nm is the ultraviolet spectrum, divided into three bands:-UVA, 320 to 400 nm
-UVB, 290 to 320 nm
-UVC, 200 to 290 nm
Virtually no UVC reaches the earth’s surface, because it is absorbed by the ozone layer.
20
21
UVA. It is constant throughout the day and the year.
• Causes immediate and delayed tanning.
• Chronic exposure to UVA radiation causes the connective tissue degeneration seen in photoaging, photocarcinogenesis, and immunosuppression.
• UVA augments the carcinogenic effects of UVB.
• UVA penetrates window glass and interacts with topical and systemic chemicals and medication.
• It produces photoallergic and phototoxic reactions.
22
UVB. Produces the most harmful effects . Snow and ice reflect UVB radiation. It is most intense when the sun is directly overhead between 10 AM and 2 PM.
• Responsible for sunburn, suntan, inflammation, delayed erythema, and pigmentation changes.
• It produces tanning more efficiently than does UVA.
• Chronic effects include photoaging, immunosuppression, and photocarcinogenesis.
• It is absorbed by window glass.
• Prior exposure to UVA enhances the sunburn reaction from UVB.
Classification of skin phototypes (SPT):
PTSBasic skin color
Response to sun exposure
1
Pale white
Do not tan , burn easily
11
White
Tan with difficulty, burn easily
111
White
Tan easily but may burn initially
1V
Light brown
Tan easily, hardly burn
V
Brown
Tan easily, usually do not burn
V1
Black
Become darker, do not burn
23
Normal cutaneous effects of ultraviolet radiation (UVR) exposure:
24
Early effects:
• Inflammation
• Suntan
Immediate; immediate, often grayish, tanning of irradiated skin, lasting for a minute or to hours, may occur within seconds of exposure to UVA.
Delayed; delayed tanning is the process by which UVR-induced melanin synthesis is transferred from melanocytes to adjacent keratinocytes. This tan typically persists for weeks to months, and gradually appears over hours to days after cutaneous exposure to UVB, UVA, UVC.
• 3)Sunburn and Solar Erythema:
UVB is 1000 times more erythemogenic than UVA, so most solar erythema is caused by UVB.UVA is 100 times greater than UVB radiation during the midday hours.
Sunlight early and late in the day contains more UVA.UVA is reflected from sand, snow, or ice to a greater degree than UVB.
Amount of ultraviolet exposure increases at higher elevation, is greater in tropical regions, and temperate climates in summer.25
Clinical signs and symptoms:
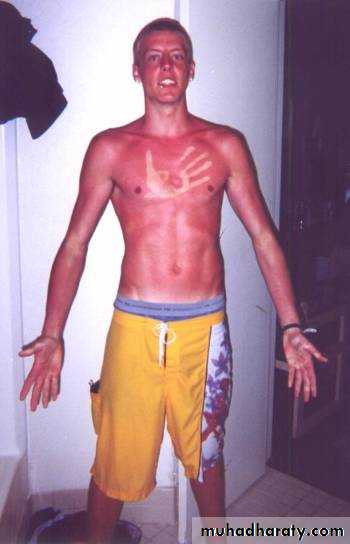
Sunburn is normal cutaneous reaction to sunlight in excess of an erythema dose (the amount that will induce reddening).
erythema is followed by tenderness, and in severe cases, blistering.
edema in the extremities and face; chills, fever, nausea, tachycardia, and hypotension may be present
Desquamation is common about a week after sunburn even in non-blistering areas.
Treatment:
Cool compresses
Topical steroids
Prophylaxis:
Avoid sun exposure between 10 am and 2 pm.Barrier protection with hats and clothing.
Sunscreen agents
26
27
28
• Late effects
Photoaging (Dermatohelioisis):
The characteristic changes induced by chronic sun exposure are called photoaging or dermatoheliosis. Common in skin type 1-blue-eyed.
29
• Individuals with photoaging may have genetic susceptibility.
• The site: V area of the neck and chest, back and sides of the neck, face, backs of the hands and extensor arms, in women the skin between the knees and ankles.• The skin become atrophic, scaly, wrinkled, inelastic, or with a yellow hue,
• Hyperplastic sebaceous glands, telangiectasis, nonmelanoma skin cancer
• Hyperpigmentation and white atrophic macules ,actinic purpura.
• Solar lentigines.
30
• Solar elastosis.
• Small yellowish papules and plaques develop along the sides of the neck.
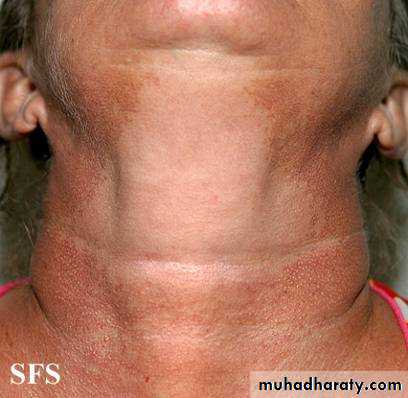
• Poikiloderma of Civatte
• Cutis rhomboidalis nuchae (sailor’s or farmer’s neck)
• Nodular elastoidosis
• Actinic purpura minimal trauma on the extensor arms leads to ecchymosis.
• Colloid milium: is a translucent, flesh-colored, or slightly yellow 1-5mm papule.
Poikiloderma of Civatte:
reticulate hyperpigmentation with telangiectasia, and slight atrophy of sides of the neck, lower anterior neck and V of chest. Submental area is spared.
Frequently presents in fair-skinned
31
Cutis rhomboidalis nuchae (sailor’s neck or farmer’s neck):
Characteristic of long-term, chronic sun exposure.Skin on back of neck becomes thickened, tough, and leathery and normal skin marking become exaggerated.
32
Favre-Racouchot syndrome :
Thickened yellow plaques studded with comedones and cystic lesions.33
Abnormal cutaneous effects of UVR exposure (the photodermatoses)
Acquired disorders with a probable autoimmune basis.34
35
1) Polymorphous light eruptions (PLE)
Most common form of sensitivity.
All races and skin types affected.
Typically in first three decades.
Females outnumber males.
Unknown pathogenesis; Some patients (10-20%) have positive antinuclear antigens (ANAs).
Different morphologies seen, although in the individual the morphology is constant. Most common papular or erythematopapular variant.
Usually affects exposed skin; scarring and atrophy do not occur. Generally symmetrical and itchy.
PMLE
the edematous papules and plaques is characteristic.36
37
2) Actinic prurigo: a rare, persistent, pruritic, excoriated, papular, or nodular eruption of sun-exposed and usually begins in childhood, may remit at puberty, is generally worse in summer, and normally fades in winter.
38
3) Hydroa vacciniforme: a very rare, chronic, scarring photodermatoses of uncertain etiology. Characterized by papulovesicles and vesicles, most commonly on the face and dorsa of the hands. Usually begins in childhood.
The effect of sunlight on some skin disorders.
HelpsAtopic eczema
Cutaneous T-cell lymphoma
Parapsoriasis
Pityriasis lichenoides
Pityriasis rosea
Pruritus of renal failure, liver disease
AIDS
psoriasis
Worsens
Darier’s disease
Herpes simplex
Lupus erythematosus
Pellagra
Photoallergy\Phototoxicity
Porphyrias
Xeroderma pigmentosum
39
40
• Photosensitivity may be phototoxic or photoallergic.
• Phototoxicity and photoallergy are different expressions of an abnormal skin reaction from the exposure to light, usually enhanced by endogenous or exogenous substances that are selectively activated by solar radiation.
Phototoxic and Photoallergic Reactions
Feature
Phototoxic reactionPhotoallergic reaction
Incidence
High
Low
Amount of agent required
Large
Small
Onset of reaction
Minutes to hours
24-72 hours
More than one exposure to agent required
No
Yes
Distribution
Sun-exposed skin only
Sun-exposed; may spread to unexposed areas
Clinical characteristics
Resembles exaggerated sunburn or blisters
Dermatitis
Immunologically mediated
No
Yes; type 1V
Occurrence after first exposure
Yes
No
Diagnosis
Clinical and phototests
Photopatch tests; clinical
41