د. بنان امراض 12\4\2018
عدد الاوراق ( 8 ) م\3\موصل lec: 6Breast pathology
Tumors of the breast :
Tumor is the most important lesion of the female breast, it is classified in to : 1- primary
A- Benign tumors :
Fibroadenoma.
Phyllodes tumors.
Papilloma (intraductal papilloma).
Adenoma .
Others, e.g. Lipoma, Fibroma,….ect.
B- Malignant tumors:
Carcinoma of the breast (most important)
Others e.g. Sarcomas, lymphoma.
2- secondary(Metastases) to the breast are rare.
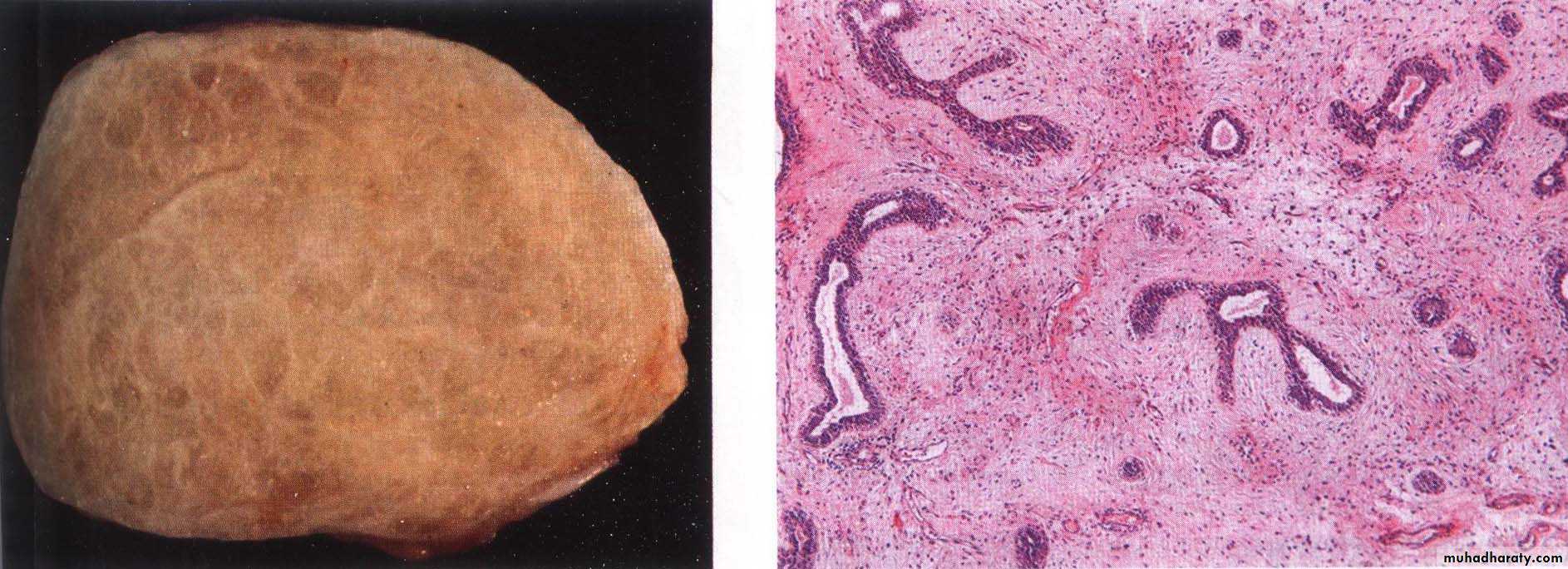
Fibroadenoma :
1- It is the most common benign neoplasm of the female breast.2- It is peak incidence in the third decade of life.
3- It is composed of epithelial and stromal elements that originated from the TDLU.
4-Clinically: it is usually solitary painless, well-demarcated from adjacent breast tissue freely movable mass.
5- Morphologically: it is well-defined
firm mass, with uniform tan-white
color on cut section, microscopically
there is delicate fibrous stroma
encloses the epithelial component
which consist of gland-like or duct-like
(some time slit like) spaces lined by cuboidal or columnar cell.
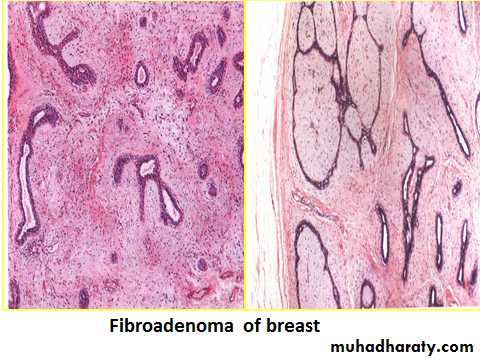
Phyllodes tumors :
These tumors are much < common than fibroadenomas, usually grow to large,possibly massive size(4-10 cm). They are thought to arise from periductal stroma and not from preexisting fibroadenoma,Like fibroadenomas, phyllodes tumors are biphasic, being composed of neoplastic stromal cells and epithelium-lined glands. However, the stromal element is more cellular and abundant, often forming epitheliumlined leaflike projections (phyllodes is Greek for “leaflike”)
Most of these tumors remain localized "benign" and are cured by excision. The malignant changes in Phyllodes tumors occurs in < 5% of cases; however it usually remains localized and only 15% may metastasize.
Malignant tumorsCarcinoma of the breast
The breast carcinoma in the USA ranks second only to lung cancer as a cause of cancer death in women; in our country it probably ranks first.Epidemiology
* The incidence of breast cancer has slowly increased over the last 20 years, this is related to the introduction of mammographic screening.* Death rates have been decreased during the last 25 years because of earlier detection and more effective treatment modalities.
*Breast cancer is 5 times more frequent in western countries than in developing countries.
* Breast cancer rarely develops in men.
Pathogenesis
* The pathogenesis of breast cancer is poorly understood, but epidemiologic, molecular and genetic studies outline complex risk factors where genetic changes, hormonal influence, environmental variables seem to be importance.
* Breast cancers exhibit diversity in histopathology molecular features, and overall patient outcomes therefore, the disease can be viewed as a multifaceted and complex epithelial malignancy.
Breast Cancer Risk Factors
1- Geographic Variations: breast cancer is significantly higher in north America and north Europe than in Asia and Africa.2- Age: Breast cancer is rare in women younger than age 25, but the incidence increases rapidly after age 30
3- Germline mutations and a positive family history of breast cancer:
-Mutations in tumor suppressor genes → > 90% risk of breast cancer
-About 15% to 20% of women with breast cancer have an affected first degree relative ,this is due to inherited mutation which are :
a- About half of the women with hereditary breast cancer have mutation in BRCA I (breast cancer I).
b- One third have mutation in BRCA II (breast cancer II).
Both act as tumor suppressive genes.
c. less common mutation in P53 .
4-Endogenous estrogen excess: early menarche (<12 Y), late menopause (>55 Y), late first pregnancy (after 35 Y), nulliparity and functioning ovarian tumors that elaborate estrogen.5-Prolonged exposure to exogenous estrogens: hormonal replacement therapy for post menopausal symptoms.
6- Benign breast disease: as atypical hyperplasia or proliferative changes.
7-Ionizing radiation to the chest increases the risk of breast cancer.
8- Many other, less well-established risk factors, such as obesity, alcohol consumption, and a diet high in fat.
**Breast feeding: the longer women breastfeed, the greater the reduction in breast cancer risk.
**Oral contraceptives have not been shown to affect the risk of breast cancer, even in women who have taken the pill for a long time.
Women who carry a breast cancer susceptibility gene(BRCA1 &or BRCA2) are more likely :
to develop breast cancer before menopause.
to have bilateral breast cancer
to have other familial forms of cancer (e.g. ovarian cancer)
to have a positive family history (i.e., multiple first-degree relatives affected before menopause)
Morphology and histological subtypes of breast cancer (Classification):
*Cancer of breast affects the left one slightly more common than the right breast.
*About 4% of women with breast cancer have bilateral primary tumors.
*The locations of tumors within the breast are mainly in upper out quadrant (50%).
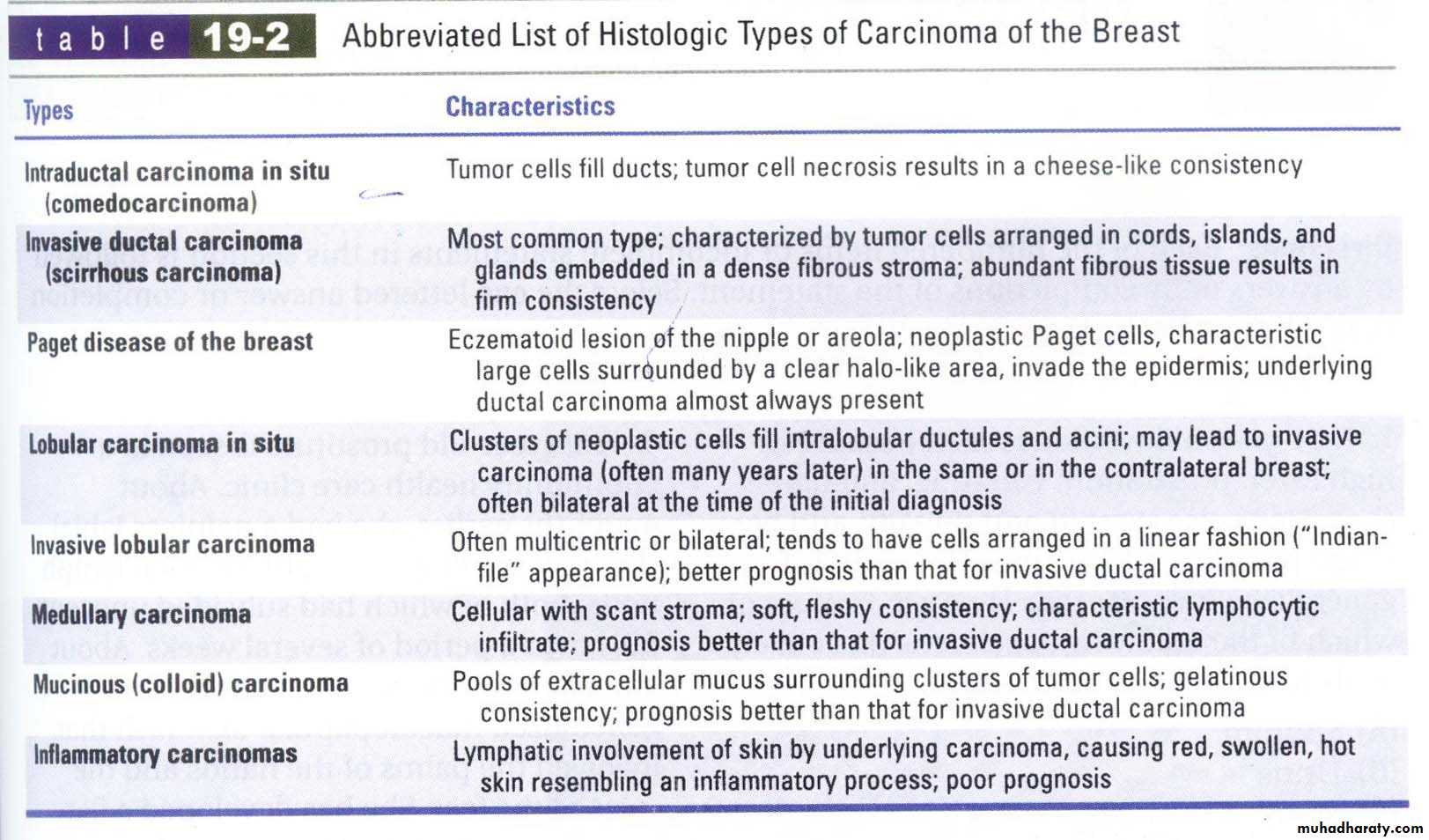
Classification of breast carcinoma:
A- Non–invasive (Carcinoma in situ): It can be divided into:1- Ductal carcinoma in situ (DCIS) (intradcutal carcinoma).
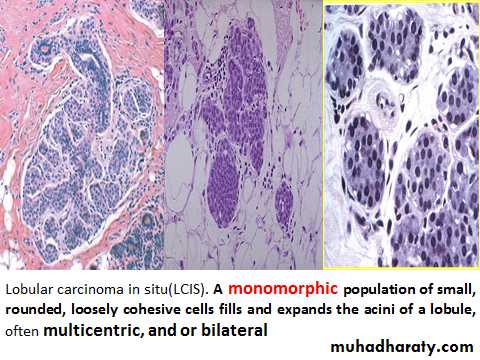
2- Lobular carcinoma in situ (LCIS).
B- Invasive (inflitrative):
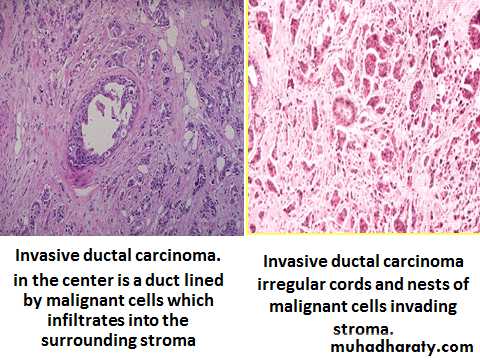
I- Invasive ductal carcinoma (not otherwise specified (NOS)) (the most common one (about 2/3 of cases)
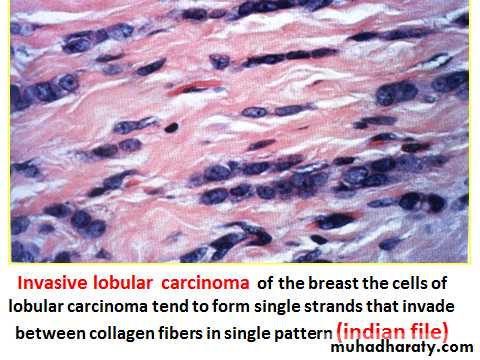
II- Invasive lobular carcinoma (often multicentric and /or bilateral)
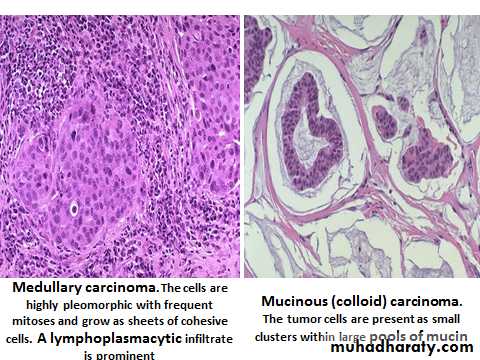
III- Medullary carcinoma .(lymphoplasmacytic infiltrate)
IV- Colloid carcinoma (Mucinous carcinoma).
V- Tubullar carcinoma.
VI- Other types (e.g. Inflammatory, papillary & metaplastic carcinoma).
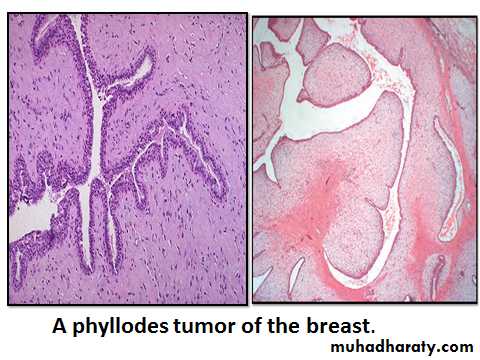
Noninvasive carcinoma(Carcinoma in situ) :
It is classified as DCIS or LCIS based on the resemblance of the involved spaces to normal ducts or lobules.
DCIS and LCIS both arise from TDLU.
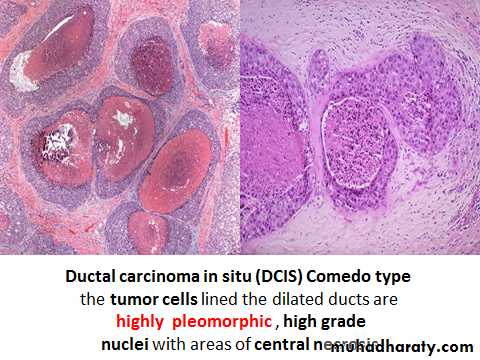
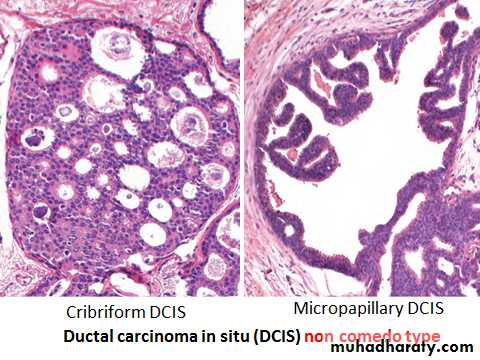
DCIS has wide variety of histological apparances: comedo type (more aggressive) (the tumor cells lined the dilated ducts are highly pleomorphic , high grade nuclei with extensive central necrosis) and non comedo type (Solid, cribriform, papillary, micropapillary).
If untreated, women with small, low-grade in situ carcinoma develop invasive cancer at a rate of about 1% per year.
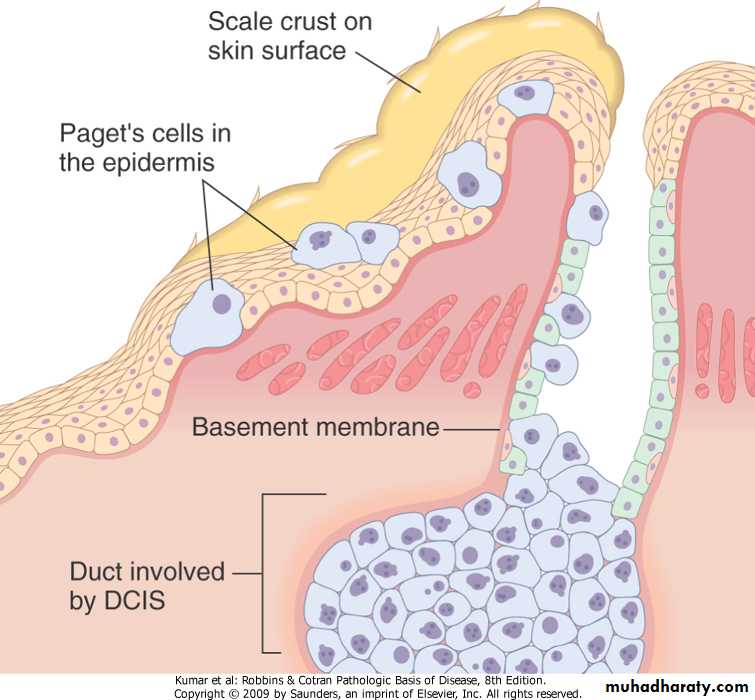
Paget's disease of the nipple
It is a rare manifestation of breast cancer, that presents as a unilateral erythematous eruption , a scale crust with pruritus, the lesion may be mistaken for eczema. The malignant cells (Paget cells) extend from DCIS within the ductal system via the lactiferous duct into nipple skin without crossing the basement membrane.A palpable mass is present in 50% to 60% of women with Paget disease, and almost all of these women have an underlying invasive carcinoma. The prognosis is not worsened by the presence of Paget's disease
Paget's disease of the nipple
Paget's disease of the breast,. The large malignant cells surrounded by clear halo like area infiltrating into the epidermis represent intraepithelial extension of an underlying ductal carcinoma (in situ or invasive)
Pathological diagnosis of breast
Clinical history with examination
Investigation: include
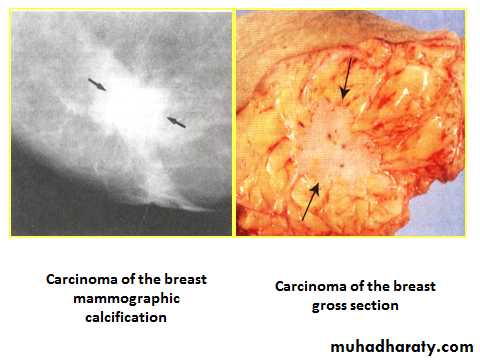
1-Radiological (US & mammograph)
2-FNAC with true cut needle biopsy.
3-Biopsy.
Prognostic and Predictive Factors:
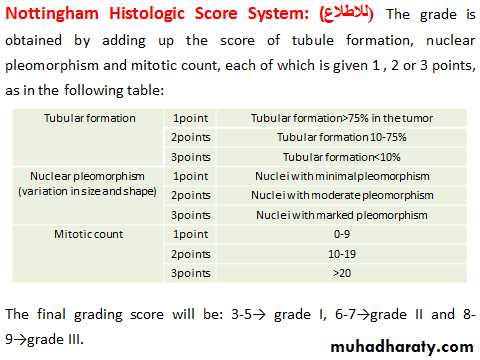
1- Histologic grade: All types of invasive carcinoma are graded using the Nottingham Histologic Score System. In this system carcinomas are scored for tubule formation, nuclear pleomorphism, and mitotic rate and the points added to divide carcinomas into grade I (well differentiated), grade II (moderately differentiated), and grade III (poorly differentiated) types. Grade I has the better prognosis.2- The staging of the breast carcinoma (TNM):
1)T: size of the primary Tumor, the smaller size the better the prognosis.
2)N: extent of lymph Node involvement: Without L-node involvement the 5 year survival rate in close to 90%.
3)M: Metastasis, Cancer with Hematogenous spread rarely curable.
3- The histological type of carcinoma: All specialized type of breast carcinoma (tubullar, medullary, mucinous) have better prognosis than carcinoma of no special type (NOS). A major exception is inflammatory carcinoma, which has a poor prognosis.
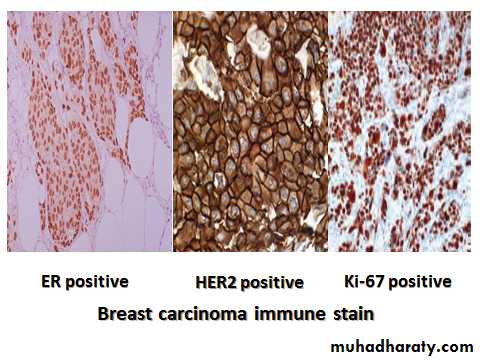
4-The presence or absence of eostrogen (ER) or progesterone receptors (PR):
The presence of hormone receptors confer a slightly better prognosis.
To predict the response to therapy, when tumors show both receptors, about 80% response to antieostrogen therapy (tamoxifen) while 25-45% response seen if only one receptors is present.
5-Over expression of HER2/NEU: HER2 is a cell membrane surface-bound receptor, HER2 over expression triggers intracellular signaling events leading to cell growth, differentiation and survival. So HER2
-It is associated with poor prognosis .
-To predict the response to a monoclonal antibody (Herceptin).
6-Proliferative rate: Proliferation can be measured by mitotic counts or by immunohistochemical detection (e.g. Ki-67)
5-Aneuploidy. Carcinomas with aneuploidy have slightly worse prognosis.
Gene expression profiling can separate breast cancer into 3 molecular subtypes:
1) ER-positive, HER2/NEU- negative (also termed “luminal,” 50% to 65% of cancers) . Based on proliferation rates, it is further divided into two subgroups:
A) ER-positive, HER2/NEU-negative, and low proliferation (40% to 55% of cancers).
B) ER-positive, HER2/NEU-negative and high proliferation (10% of cancers).
2) HER2/NEU-positive (20% of cancers). About half of these cancers are ER-positive and half ER negative.
3) ER-negative, HER2/NEU-negative tumors (“basal-like” or triple negative carcinoma(all cases PR-negative); 15% of cancers).
These subtypes are associated with different outcomes and, in some instances, different therapies.
Spread of breast cancer
Direct: it invade the breast tissue and overlying skin with ulceration and nipple retraction, it may invade underlying muscle and chest wall.Lymphatics: Permeation of the local dermal lymphatics by tumor causing blockage of lymphatics and edema of the skin producing a Peau d orange skin appearance.
Invasion of axillary L-nodes.
Invasion of internal mammary L-nodes.
Invasion of supraclavicular L-nodes .
Blood : spread to lung, liver, long bones, and brain.
The Male Breast
Gynecomastia (enlargement of the male breast):It occurs as a result of an imbalance between estrogens, which stimulate breast tissue, and androgens, which counteract these effects.
It may appear during puberty or at any time during adult life when there is cause for hyperestrinism (e.g. liver cirrhosis, drugs (such as heroin and anabolic steroids), alcohol or in association estrogen secreting tumors) .
Microscopically: an increase in the stroma (dense collagenous connective tissue ) with duct enlargement and sometimes epithelial hyperplasia. a Lobule formation is almost never observed.
Gynecomastia may be associated with a small increased risk of breast cancer.
Gynecomastia
Male Breast CancerThe incidence is < 1% of that in women.
The typical age at diagnosis is between 60 and 70 years
The pathology of male breast cancer is remarkably similar to that of cancers seen in women. However, ER positivity is more common.