د. خالد امراض 5\3\2018
عدد الاوراق ( 8 ) م\3\موصل lec: 2Infectious Disorders
VIRAL HEPATITIS.hepatic infection caused by hepatotropic viruses (A, B, C, D, & E)
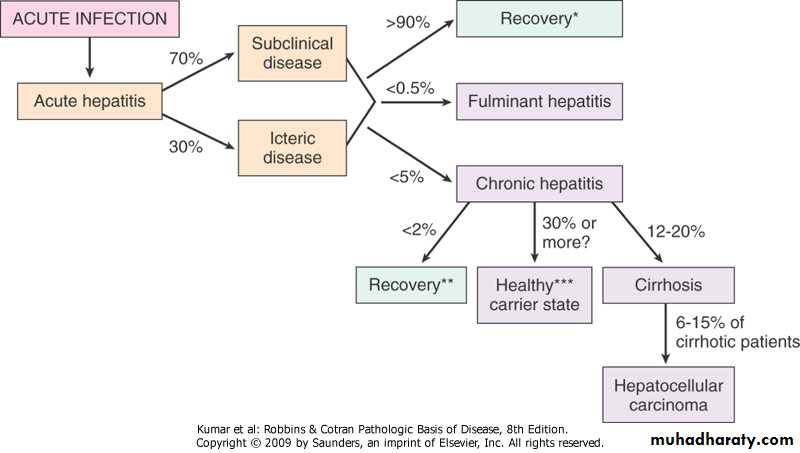
.clinicopathologic syndromes -acute asymptomatic infection with recovery (serologic evidence-HAV & HBV) -acute symptomatic hepatitis with recovery, anicteric or icteric (all types) -chronic hepatitis, without or with progression to cirrhosis (HCV) symptomatic, biochemical, or serologic evidence of continuing or relapsing hepatic disease for more than 6 months -fulminant hepatitis with massive to submassive hepatic necrosis (HBV, HAV)
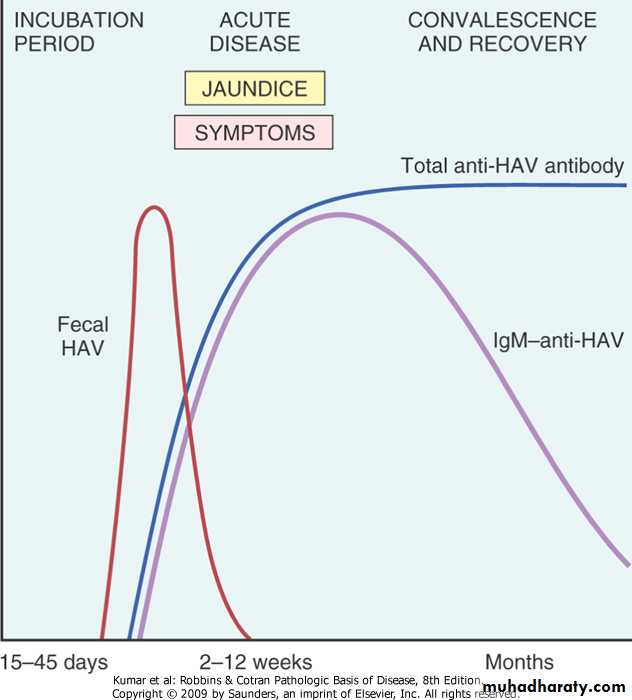
.diagnosis -serological tests -liver biopsy -molecular studiesHepatitis A Virus.single stranded RNA picovirus with incubation period of 3-6 weeks .clinical features -asymptomatic or mild, rare after childhood -rarely fulminant hepatitis (0.1%).occurs worldwide & is endemic in places with substandard hygiene (people may have detectable antibodies by age of 10y).spread is by contaminated water & food (oral route).virus is shed in stool for 2-3 wks before & 1 wk after onset of jaundice.can also be detected in serum & saliva because HAV viremia is transient, blood-borne transmission occurs only rarely; therefore, donated blood is not specifically screened for this virus
.specific anti-HAV IgM antibodies at onset of symptoms (diagnostic marker in acute infection), titer declines in months.IgG persists for years, providing protective immunity against re-infection by all strains of HAV
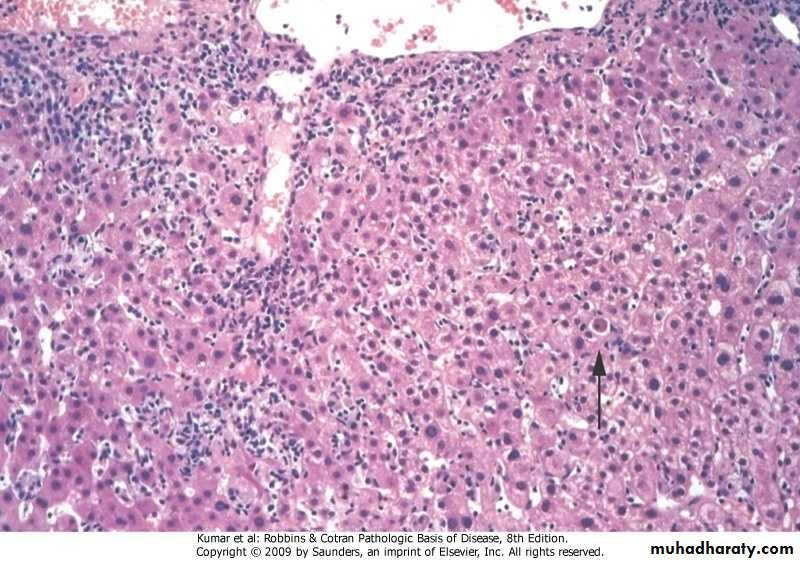
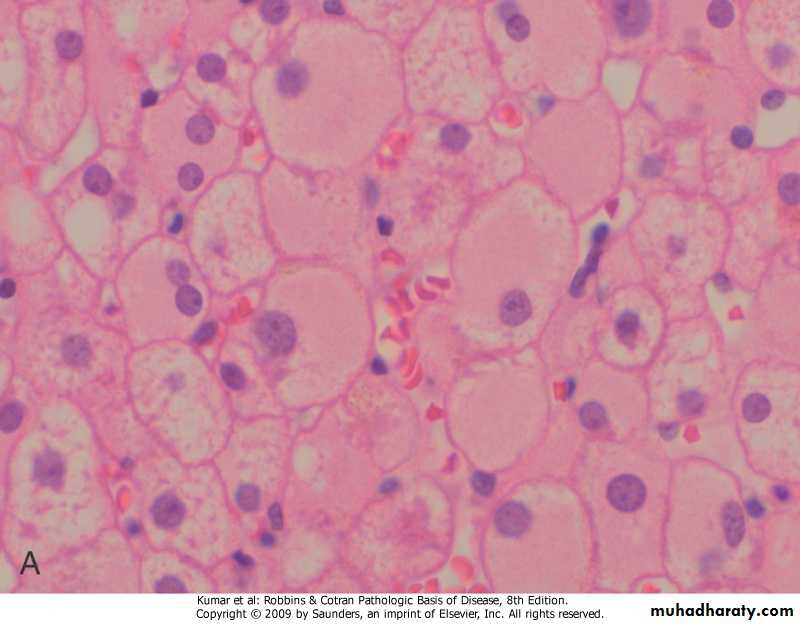
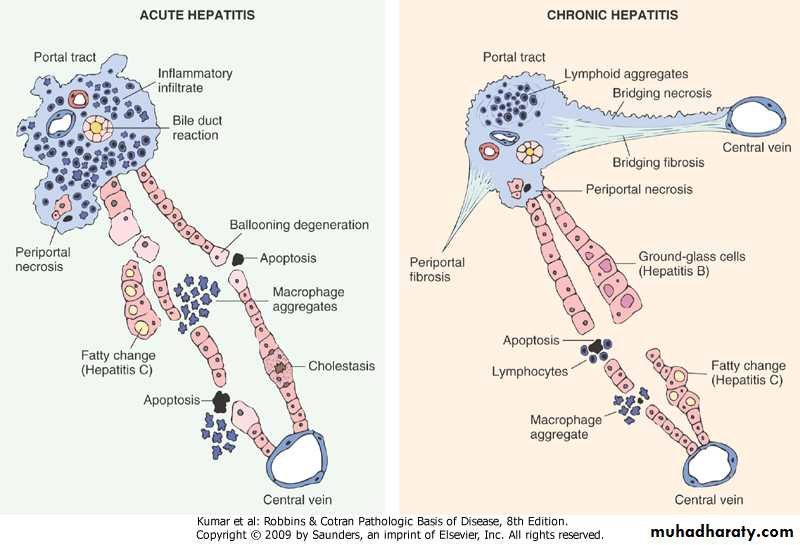
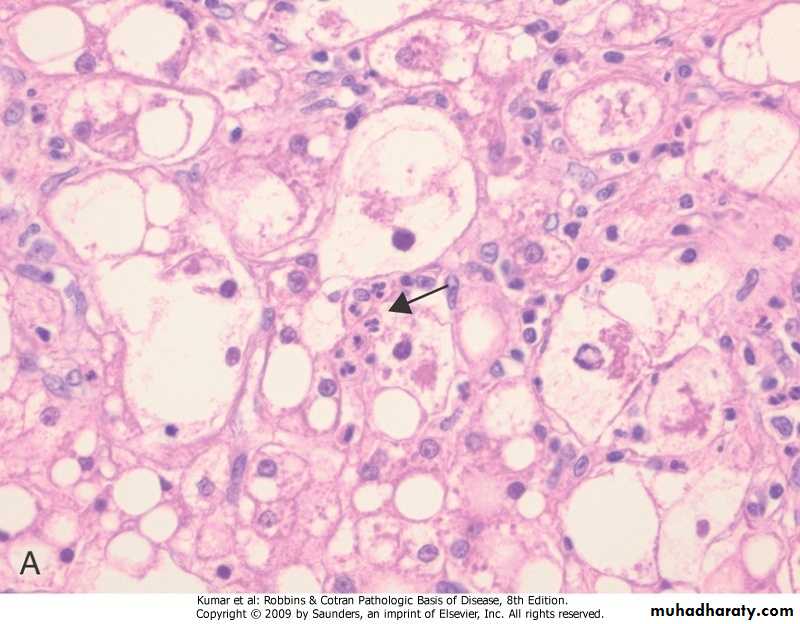
Acute viral hepatitis
Ballooning degeneration
Hepatitis B Virus.DNA virus, incubation period 4-26 wks.diseases -acute hepatitis with recovery -nonprogressive chronic hepatitis -progressive chronic disease>cirrhosis -fulminant hepatitis -asymptomatic carrier state (presence of HBsAg in serum for 6 months or longer) -hepatocellular carcinoma
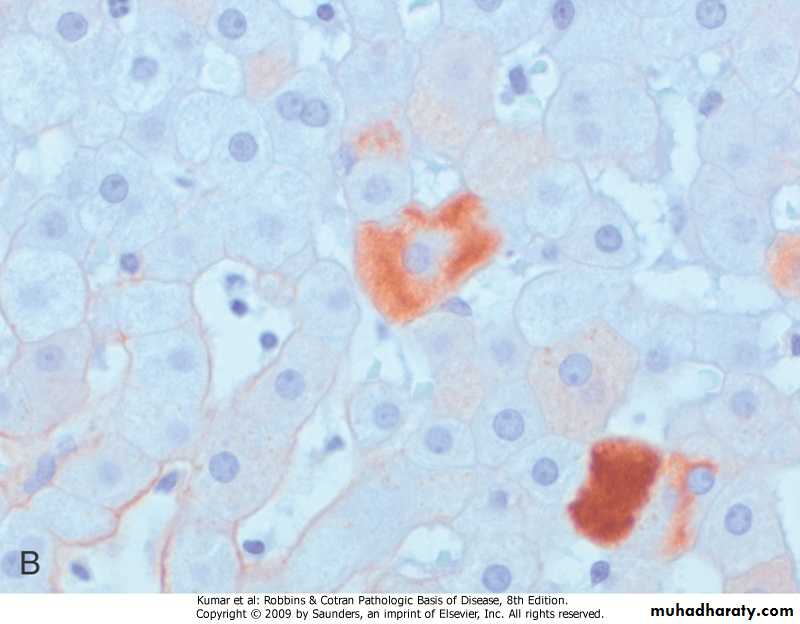
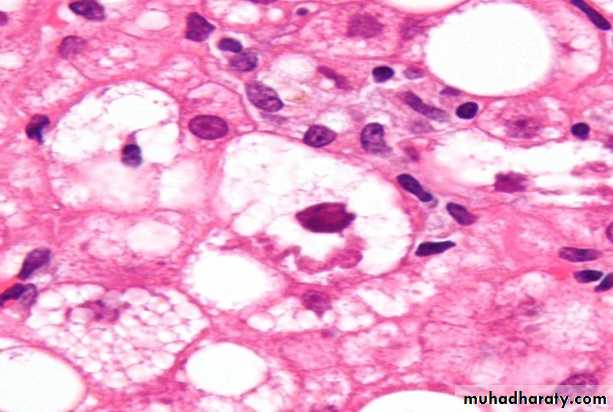
Chronic HBV hepatitis, ground-glass hepatocytes
Chronic HBV hepatitis, immuno-peroxidase stain for HBsAg
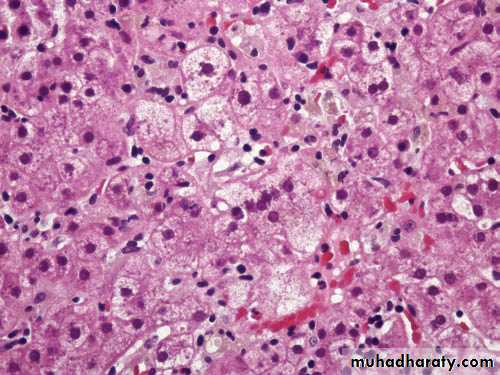
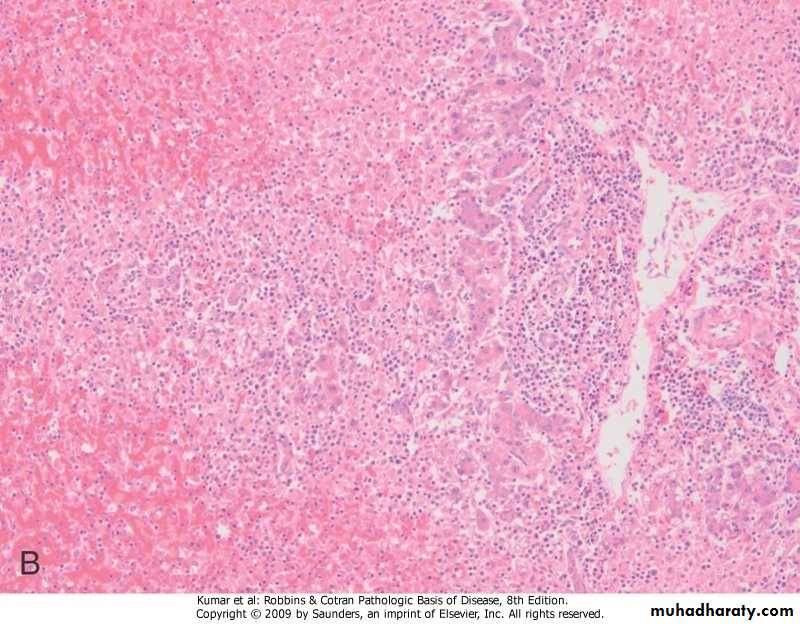
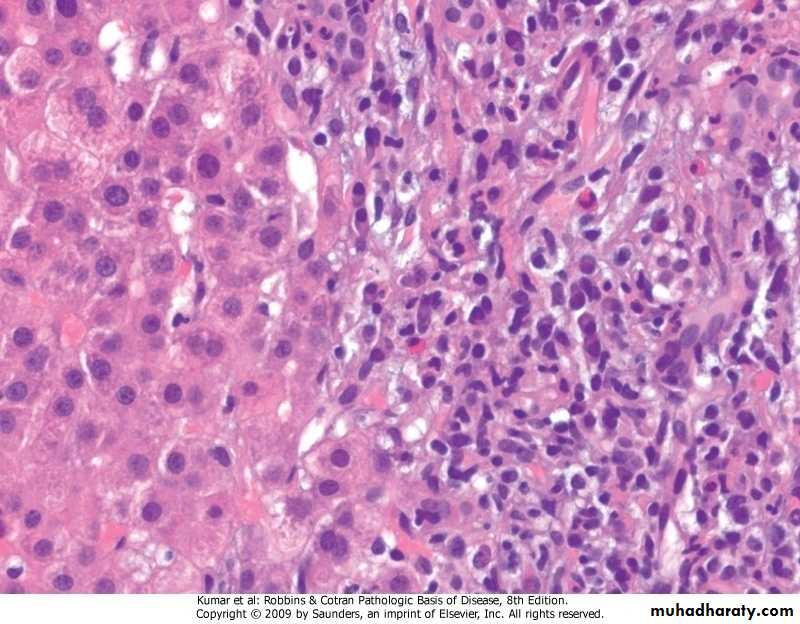
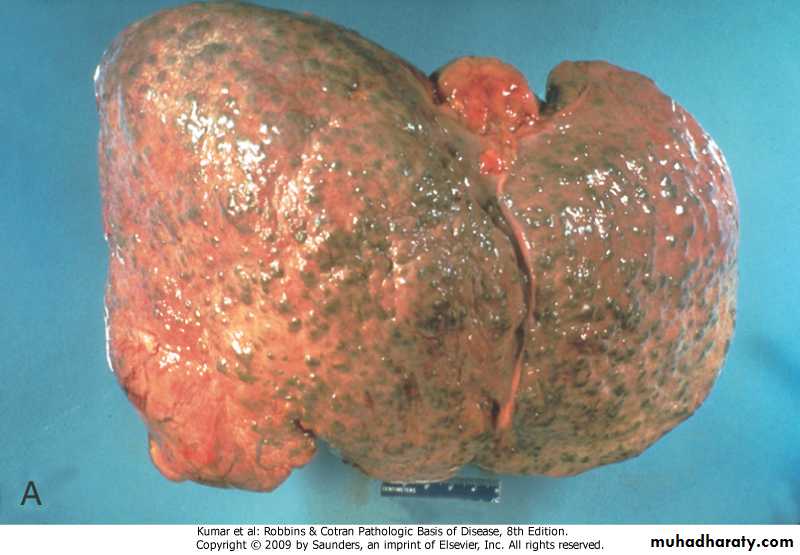
Fulminant viral hepatitis
Fulminant viral hepatitis.modes of transmission -vertical .perinatal during childbirth (high prevalence regions) -horizontalvia transfusion, blood products, dialysis, needlestick accidents among health care workers, sharing of needles in intravenous drug use and through minor cuts in skin or mucous membranes (intermediate prevalence regions) .sexual & intravenous (low prevalence regions).prevention -vaccination -screening of donor blood & tissuesanti-HBs may persist for life, conferring protection; a basis for vaccination using noninfectious HBsAg Hepatitis C Virus
.single stranded RNA, incubation period 2-26 weeks
.most common chronic blood-borne infection
.routes of transmission
- intravenous
-blood transfusions
-sexual intercourse
-perinatal
.diseases -acute hepatitis (rarely fulminant) -chronic hepatitis .characteristic clinical feature is episodic elevations in serum aminotransferases -cirrhosis .in 20%-30% of patients with chronic infection .after 5-20y of acute infection
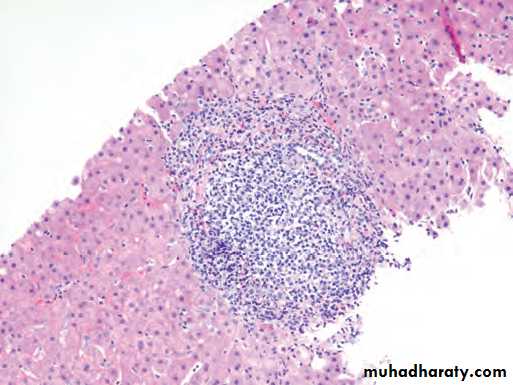
Chronic viral hepatitis due to HCV showing characteristic portaltract expansion by a lymphoid follicle.
Hepatitis D Virus
.RNA virus dependent for its life cycle on HBV .hepatitis arises in the following settings -acute coinfection after exposure to serum containing both HDV & HBV .acute hepatitis (self-limited or fulminant) .chronic hepatitis (persistent or progressive)-super-infection of a chronic carrier of HBV .severe acute hepatitis .exacerbation of preexisting chronic hepatitis B, may progress to cirrhosis & hepatocellular carcinoma
Hepatitis E Virus
.single stranded RNA, incubation period 6 weeks
.water-borne infection affecting young to middle-aged adults (oral route)
.zoonotic with animal reservoirs (mokeys, cats, pigs, and dogs)
.causes acute self-limiting hepatitis
.among pregnant women has a high mortality rate (20%)
HIV and Chronic Viral Hepatitis .because of similar transmission mode & similar high-risk patient population, co- infection of HIV & HVs is now a common clinical problem .HIV infection exacerbates the severity of liver disease caused by HBV or HCV.less clear is the impact of HBV or HCV on the course of HIV infection.in addition, anti-HIV agents may cause hepatotoxicity in some patients with HBV or HCV co-infection
Autoimmune Hepatitis.chronic & progressive hepatitis of unknown etiology
.pathogenesis
-T cell-mediated autoimmunity (defect in regulatory T-cells), which may be genetically determined
-injurious immune reaction may be triggered by
.viral infections
.drugs (methyldopa, interferons, nitrofurantoin)
.herbal products
. Features -clinical .female predominance .indolent or severe (fulminant hepatitis) .cirrhosis in 40% of survivals . The presence of other forms of autoimmune diseases, including rheumatoid arthritis, thyroiditis, Sjögren syndrome, and ulcerativecolitis -serological .absence of markers of viral infection .elevated serum IgG & γ-globulin levels .high serum titers of auto-antibodies -histological .lymphocytes & plasma cells in the interface of portal tracts & hepatic lobules
Autoimmune hepatitis
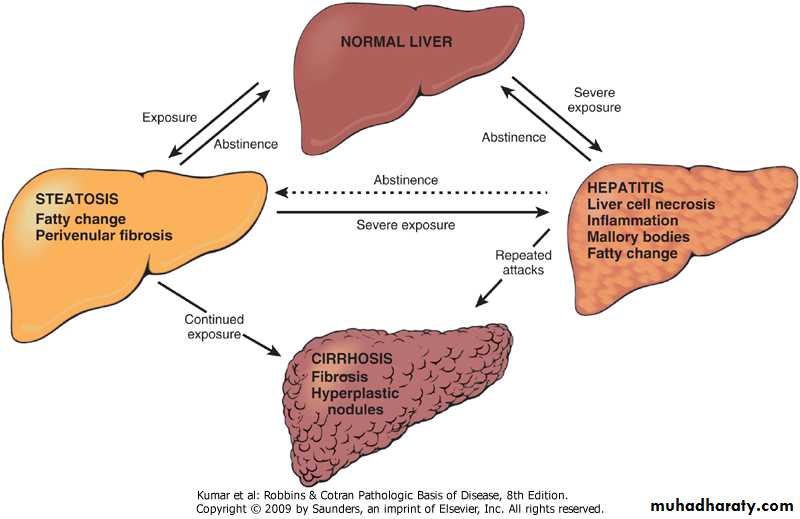
ALCOHOLIC LIVER DISEASE.factors influencing development & severity of liver disease -quantity of alcohol -duration of consumption -gender, women are more susceptible to hepatic injury than men -genetic -iron overload & infections (HCV, HBV).diseases, 3 overlapping forms -steatosis (fatty liver disease) .asymptomatic .hepatomegaly & mild elevation of serum bilirubin & alkaline phosphatase -hepatitis (minimal to fulminant) -cirrhosis
.pathogenesis -hepatocellular steatosis .increased lipid biosynthesis .defect in assembly & secretion of lipo- proteins .increased peripheral catabolism of fat -hepatitis .acetaldehyde induces disruption of cytoskeletal & membrane function .reactive oxygen species react with cellular proteins, & damage membranes .low hepatic glutathione>oxidative injury
.morphology -steatosis -hepatitis .hepatocyte swelling & necrosis .Mallory bodies .neutrophil infiltration .fibrosis -cirrhosis
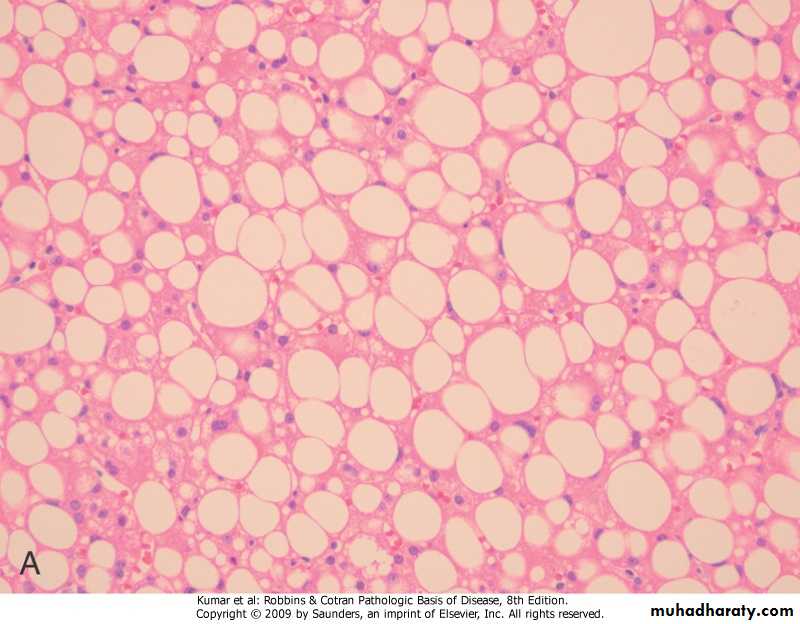
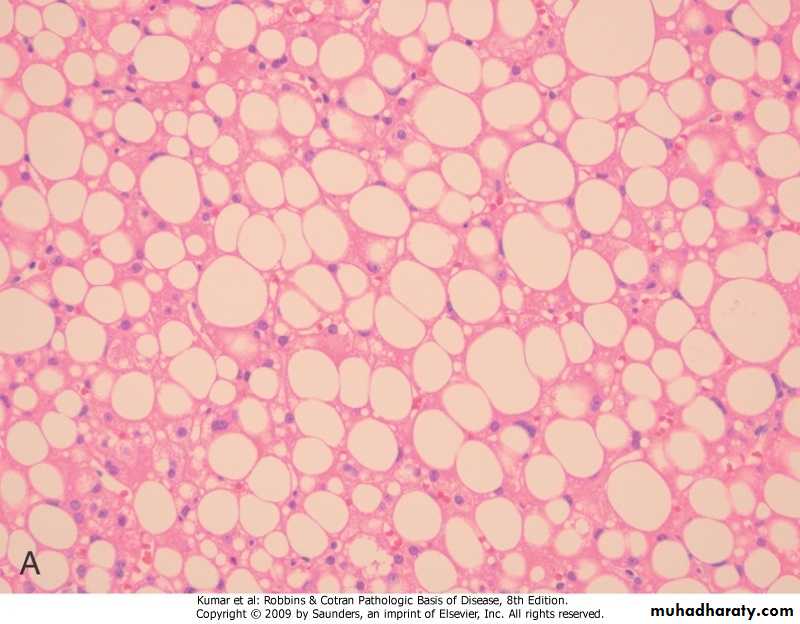
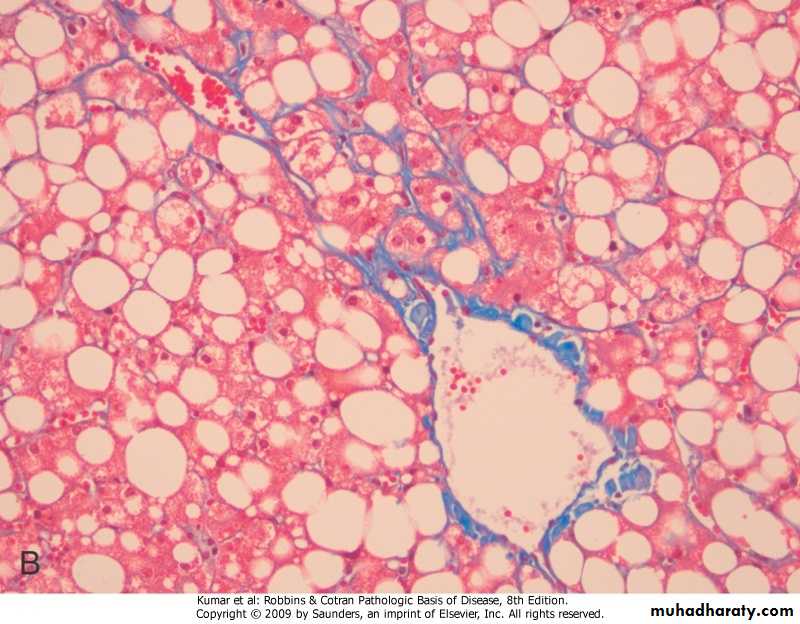
Liver, steatosis
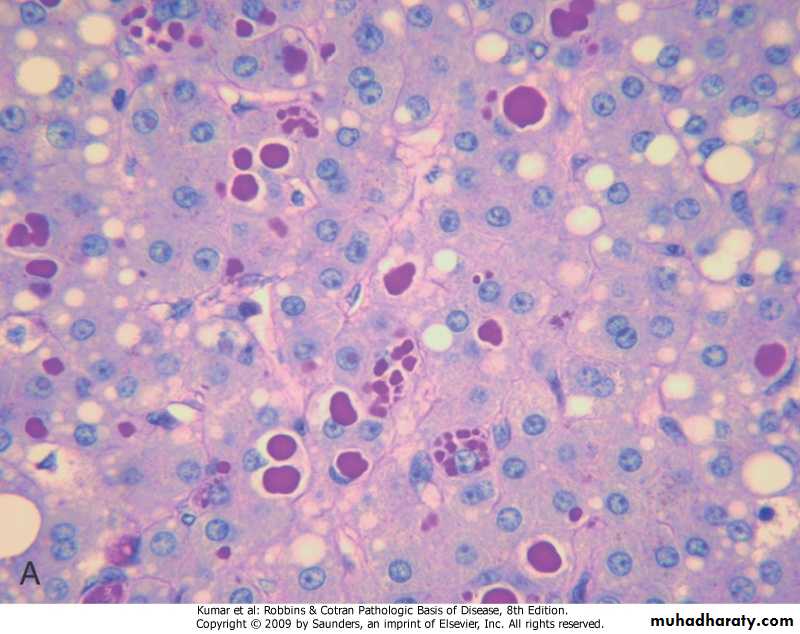
Alcoholic hepatitis
Alcoholic hepatitis, Mallory bodies
Alcoholic cirrhosis
Alcoholic cirrhosis, Masson trichrome
Metabolic Liver Diseaseseither acquired or inherited.
The most common acquired metabolic disorder is non-alcoholic fatty liver disease(NAFLD).
Among inherited metabolic diseases, hemochromatosis, Wilson disease, and α1-antitrypsin deficiency are most prominent.
Also included among liver metabolic diseases is neonatal hepatitis.
NON-ALCOHOLIC FATTY LIVER DISEASE (NAFLD).simple hepatic steatosis.steatosis with minor inflammation -both are asymptomatic.non-alcoholic steatohepatitis (NASH) -hepatocyte injury>cirrhosis in 10%-20% -pathogenesis, genetics & environment “two-hit” model .hepatic fat accumulation .hepatic oxidative stress
Steatosis
NASH
HEMOCHROMATOSIS.excessive accumulation of body iron, mostly in liver & pancreas .types -primary -secondary (hemosiderosis) .repeated blood transfusions .increased intestinal absorption of ironprimary (hereditary) hemochromatosis
.autosomal recessive, due to excessive intestinal absorption of iron.diagnosed at 5th decade of life
.males predominate by 5:1 to 7:1
.fully developed cases exhibit
-micronodular cirrhosis>hepatocellular carcinoma
-diabetes mellitus
-skin pigmentation
.pathogenesis -excessive iron is toxic to tissues through .lipid peroxidation via free radicals .stimulation of collagen via activation of stellate cells .interaction of reactive oxygen species & iron with DNA>lethal cell injury or hepatocellular carcinoma
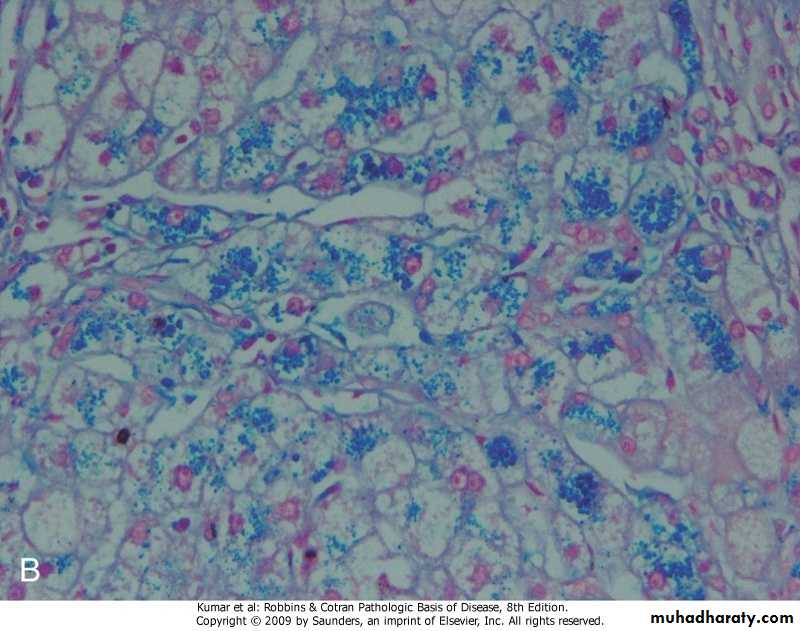
Hemochromatosis
Hemochromatosis, Prussian blue stain
WILSON DISEASE.autosomal-recessive characterized by deficiency in ATP7B enzyme leading to -decrease in copper transport into bile -impairment of copper incorporation into ceruloplasmin -inhibition of ceruloplasmin secretion into the blood -accumulation of toxic levels of copper in .liver, (steatohepatitis, necrosis, cirrhosis) .brain, (damage to basal ganglia) .eye, (Kayser-Fleischer ring)
.clinical features -rare before the age of 6 years -acute or chronic liver disease -neuropsychiatric manifestations.diagnosis -biochemical changes .decrease in serum ceruloplasmin .increase in hepatic copper content (sensitive & specific test) .increase urinary excretion of copper (most specific screening test) -clinical (Kayser-Fleischer ring)
ALPHA-1 ANTITRYPIN DEFICIENCY
autosomal-recessive disorder
The AAT gene, located on human chromosome 14, is very polymorphic, and at least 75 forms have been identified.
The most common genotype is PiMM, occurring in 90% of individuals.
The most common clinically significant mutation is PiZ; homozygotes for the Z allele (PiZZ genotype) have circulating AAT levels that are only 10% of normal levels.
all persons with the PiZZ genotype accumulate AAT in the liver, but only 8% to 20% develop significant liver damage.
AAT alleles are autosomal codominant, and consequently PiMZ heterozygotes have intermediate plasma levels of AAT
ALPHA-1 ANTITRYPIN DEFICIENCY.pathogenesis -accumulation of α1AT in endoplasmic reticulum leads to .autophagy .mitochondrial dysfunction .inflammation & hepatocyte damage .morphology -hepatocytes show (fatty change, hyaline cytoplasmic inclusions, Mallory bodies)
.clinical features -only 10%-15% of affected individuals have overt clinical features due to presence of .other genetic factors .environmental factors -in neonates .hepatitis & jaundice -in adolescence .hepatitis>recovery, or>cirrhosis -in adults .cirrhosis .liver cell carcinoma in 2%-3%