د. شامل ادوية 5\4\2018
عدد الاوراق ( 9 ) م\3\موصل lec:16ANTIBIOTICS
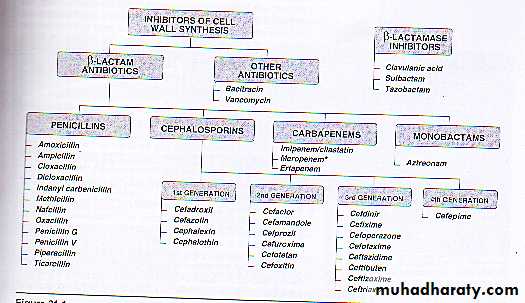
Penicillins
and Cephalosporins
Beta-lactam antibiotics
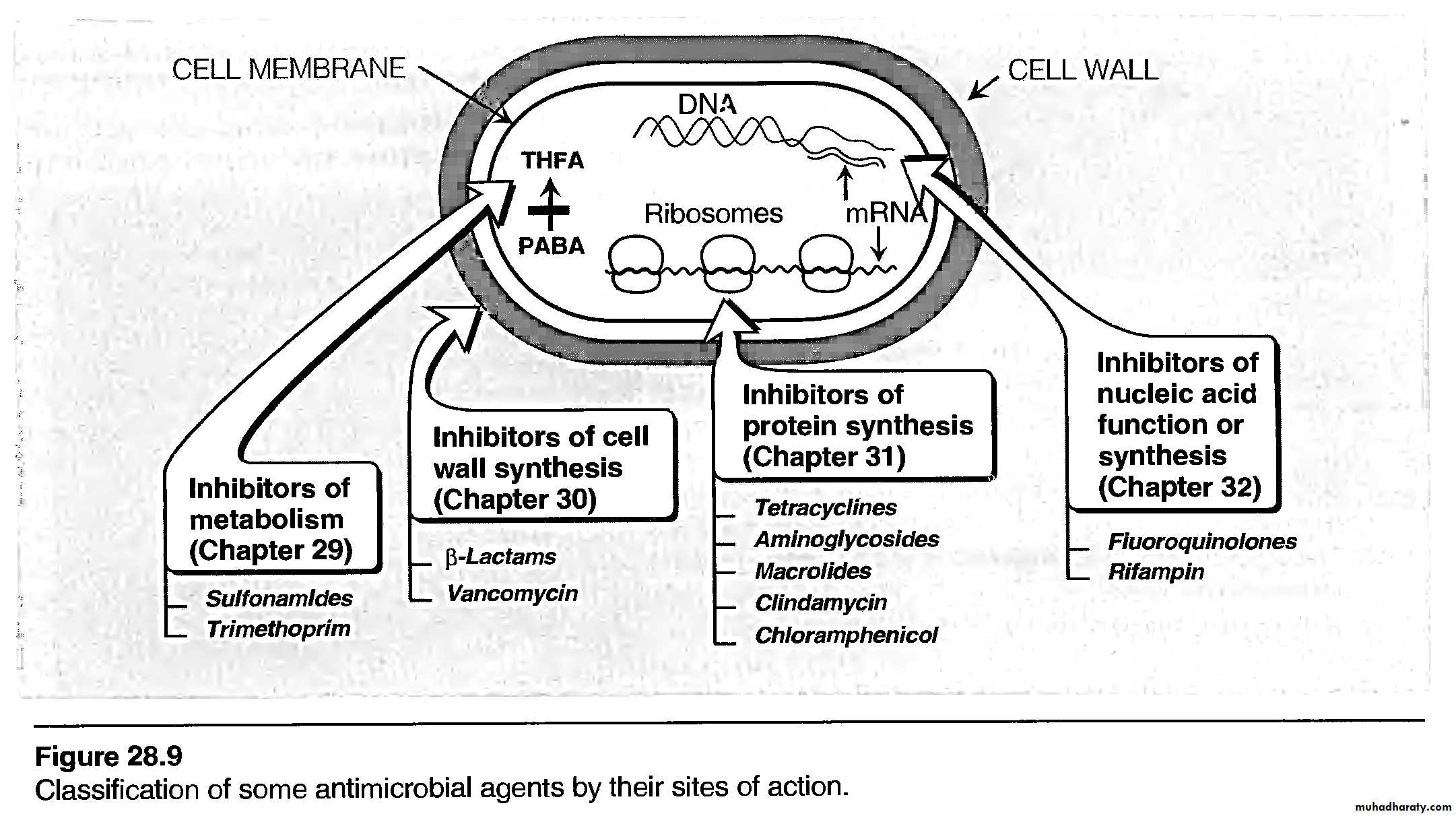
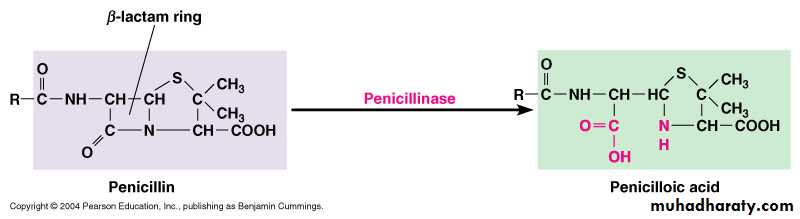
Drugs with structure containing a bata-lactam ring; include the penicillins and cephalosporins. This ring must be intact for antimicrobial action.Beta-lactamases:
Bacterial enzymes (penicillinases, cephalosporinases) that hydrolyze the lactam ring of certain penicillins and cephalosporins.
Penicillin- binding proteins (PBP):
Bacterial cytoplasmic membrane proteins that acts as the initial receptors for penicillins and other beta-lactam antibiotics
Peptidoglycan , Murein (NAM, NAG):
Chain of polysaccharides and polypeptides that are Cross-linked to form the bacterial cell wall.
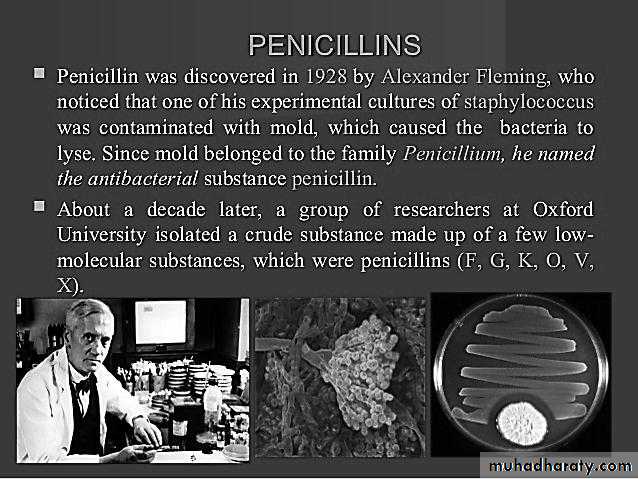
Penicillins
A- Classification:- All penicillins are derivative of 6-aminopenicillanic acid and contain a beta-lactam ring structure that is essential for antibacterial activity.
- Penicillin subclasses have additional chemical structure that confer differences in antimicrobial activity, susceptibility to acid and enzymatic hydrolysis, and biodisposition.
C- Mechanism of Action and Resistance:
# Beta-lactam antibiotics are bactericidal drugs.# They act to inhibit cell wall synthesis by the following steps:
(1)binding of the drug to specific receptors (PBP).
(2)inhibition of transpeptidase enzymes.
(3)activation of autolytic enzymes that cause
lesions in the bacterial cell wall.
B- Pharmacokinetics:
# Penicillins vary in their resistance to gastric acid and therefore vary in their oral bioavailability.
# They are usually excreted unchanged in the urine via glomerular filtration and tubular secretion, the later process being inhibited by probenecid.
# Ampicillin and nafcillin are excreted partly
in the bile.
# t ½ vary from 30 min. to 1 hr.
# procaine and benzathine forms of penicillin G are administrated i.m and have long t ½ .# most penicillins cross the blood-brain barrier only when the meninges are inflamed.
# Enzymatic hydrolysis of the beta-lactam ring results in loss of antibacterial activity.
# The formation of beta-lactamases (penicillinases) by most staph. And many gram-negative organisms is thus a major mechanism of bacterial resistance.# Structural changes in target PBPs is another mechanism of resistance and is responsible for methicillin resistance in staphylococci and for resistance to penicillin G in pneumococci.
# In some gram-negative rods (e.g. Pseudomonas aeruginosa ) changes in the porin structure in the outer membrane may contribute to resistance by impeding access of penicillins to PBPs.
#Inhibitors of these bacterial enzymes (eg. Clavulanic acid, sulbactam, tazobactam) are sometimes used in combination with penicillins to prevent Their inactivation.
D. Clinical uses:
1. Narrow spectrum, penicillinase- susceptible agents:(prototype is penicillin G)
# Clinical use include therapy of infections caused by :
- Streptococci.
- Meningococci.
- Gram positive bacilli.
- Spirochetes.
# Resistant m.o. :
- Several strains of pneumococci.
- Most strains of Staph. Aureus.
- Strains of N. gonorrhoeae
# It is the drug of choice for syphilis.
# Activity against enterococci is enhanced by aminoglycisides.
# Penicillin V is an oral drug used mainly in oropharyngeal infections.
2- Very narrow spectrum, penicillinase-
resistant drugs:
- includes methicillin (prototype), nafcillin
and oxacillin.
- used in the treatment of staphylococcal
infections.
- MRSA are resistant to members of this
subgroup and may be resistant to multiple
antimicrobial drugs.
3- Wider spectrum, penicillinase-susceptable
drugs:
a. Ampicillin and amoxicillin:
- Their indications similar to penicillin G
as well as infections due to enterococci,
Listeria monocytogenes, E. coli, Proteus
merabilis, Haemophilus influenzae , and
Moraxella catarrhalis , though resistant
strains occur.
- When used in combination with inhibitors of penicillinases ( clavulanic acid, etc.) their antibacterial activity is enhanced.
- In enterococcal and listerial infections ampicillin is synergistic with aminoglyciside.
b- Piperacillin and ticarcillin:
- Have activity against several G- rods
including pseudomonas, enterobacter and in some cases Klebsiella spp.
- most members have synergism with
aminoglycosides.
- they are susceptible to penicillinases and
often used in combination with penicillinase inhibitors.
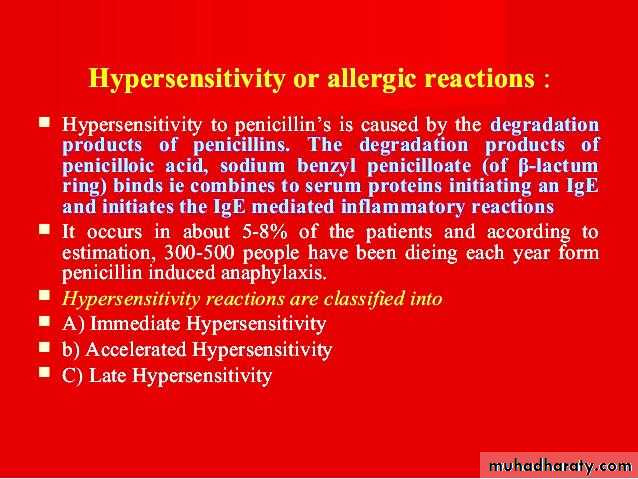
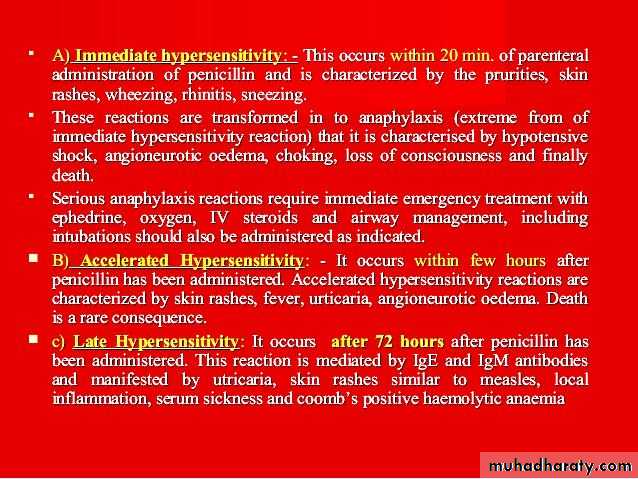
E. Toxicity:
1. Allergy: include urticaria, severe pruritus,
fever, joint swelling, haemolytic anemia, nephritis, and anaphylaxis.
- About 5-10 % of persons with a past
history of penicillin reaction have an allergic response when given it again.- Methicillin causes nephritis more than others.
- nafcillin is associated with neutropnia.- Complete cross-allerginicity between different penicillins should be assumed.
- Ampicillin frequently causes maculopapular skin rashes that may not be an allergic reaction.
2. Gastrointestinal disturbances:
- Nausea and diarrhea may occur with oral penicillins, especially with ampicillinwhich has been implicated in pseudo-
membranous colitis.
- Gastrointestinal upsets may be caused by
direct irritation or by overgrowth of gram- positive organisms or yeasts.
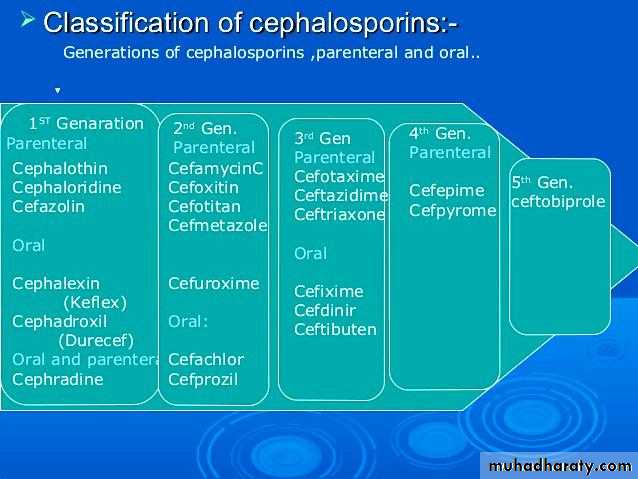
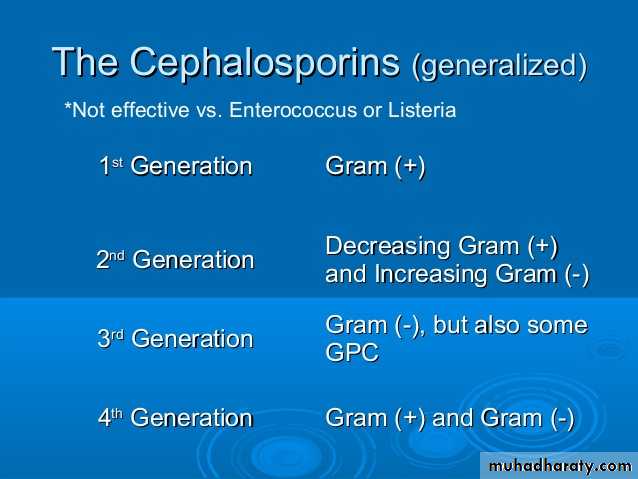
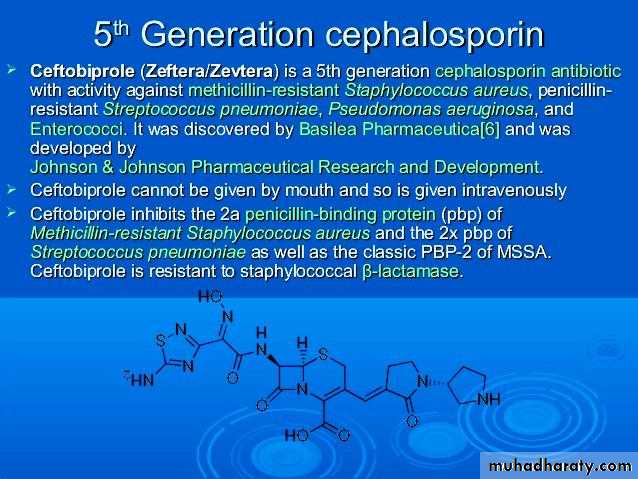
CEPHALOSPORINS:
A. Classification:- Derivatives of 7-aminocephalosporanic
acid and contain the beta-lactam ring
structure.
- They are designated first-, second-, third-, forth and fifth- generation drugs according to the order of their introduction Into clinical use.
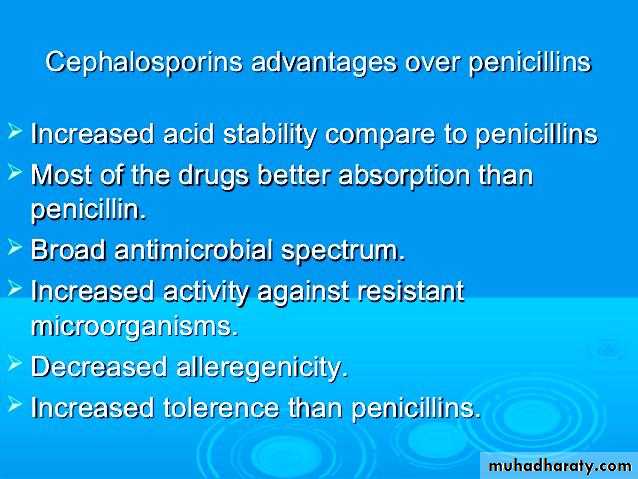
B. Pharmacokinetics:
- several are available for oral use butmost administered parentrally.
- The major elimination is by renal excretion via active tubular secretion, some may undergo hepatic metabolism.
- Cefoperazone and ceftriaxone are excreted mainly in the bile.
- Most 1st and 2nd generation do not enter the CSF fluid even when the meninges are inflammed.
C. Mechanism of Action and Resistance:
- They bind to PBPs on bacterial cell membrane to inhibit cell wall synthesis by mechanism similar to those of the penicillins.- Cephalosporins are batericidal against susceptible organisms.
- less susceptible to staph. Penicillinases.
- some bacteria are resistant through the production of other beta-lactamases.
- Resistance may resulted from decrease in membrane permeability and from changes in PBPs.
- Methicillin resistant staph. are also resistant to most cephalosporins.
D. Clinical Uses:
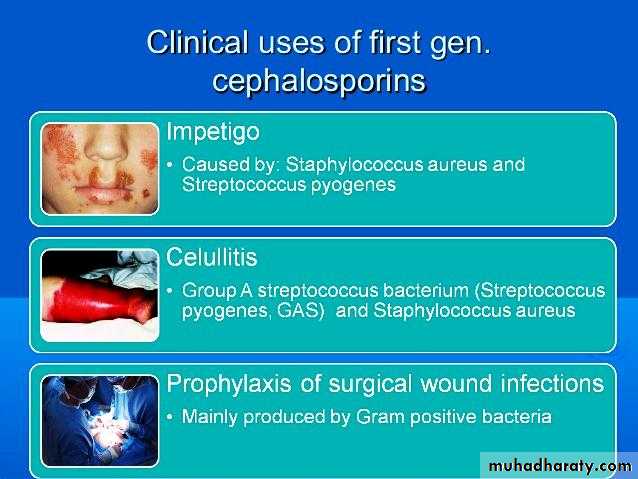
1. First generation drugs:
- Cefazolin (parentral) and Cephalexin
(oral) are examples of this subgroups.
- They are active against G+ cocci, including Staph. and Strept., E. coli and K. pneumoniae.
- Clinical uses include treatment of infections
Caused by these organisms and surgical prophylaxis in selected conditions.
- Have minimal activity against gram-negative cocci, enterococci, methicillin-resistant Staph, and most G-rods.
2. Second-generation drugs:
- Less active against G+ organisms than the 1st generation drugs but have an extended G- coverage.- Clinical uses include infections caused by Bacteroids fragilis (Cefotetan, cefoxitin) and by H. influenzae or Morexella catarrhalis (cefuroxime, cefaclor).
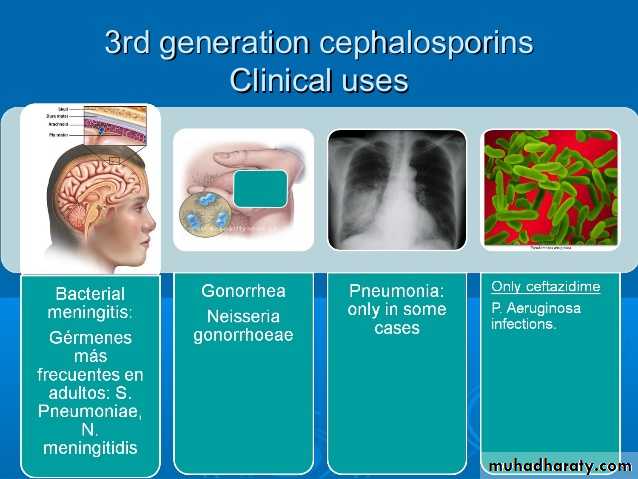
3. Third Generation Drugs: (Cefoperazone, Cefotaxime)
- increased activity against G- organisms
resistant to other beta-lactam drugs and ability to penetrate the blood –brain barrier (excpet cefoperazone and cefixime).
- Most are active against enterobacter,
providencia, Serratia marcescens and beta- lactamase producing strains of H. influenzae and Neisseria.
- Individual drugs also have activity against pseudomonas (cefazidime) and B. fragilis (ceftizixime).
- Drugs in this subclass should usually be reserved for treatment of serious infections (e.g. bacterial meningitis).
- Ceftriaxone (parenteral) and cefixime (oral),currently drugs of choice in gonorrhea
- Likewise, in acute otitis media,a single injection of ceftriaxone is an effective as 10-days course of treatment with amoxicillin or cefaclor.
4. Fourth-generation drugs:
- Cefipime is more resistant to beta- lactamases produced by G- organisms,
including enterbacter, haemophilus, and
neisseria.
- Cefipime combines the G+ activity of the
1st generation agents with the wider gram-negative spectrum of the 3rd generation cephalosporins.
E. Toxicity:
1. Allergy:- Cephalosporin cause a range of allergic reactions from skin rashes to anaphylactic shock. They occur less frequently with cephalosporin than with penicillins.
- Complete cross hypersensitivity between different cephalosporins should be assumed.
- Cross- reactivity between penicillins and cephalosporins is incomplete (5-10 %).
- Patients with a history of anaphylaxis to penicillins should not be treated with cephalosporins.
2. Other adverse effects:
- They may cause pain at intramuscular injection sites and phlebitis after iv administration.
- Increase the nephrotoxicity when combined with aminoglycosides.
- Drugs containing a methylthiotetrazole
group (cefoperazone, cefotetan, moxalactam) cause hypoprothrombineamia and may cause disulfiram-like reactions with ethanol.
- Moxalactam also decreases platelet function and may cause severe bleeding.
Other Beta-lactam Drugs
A. Aztreonam:
- is a monobactam that is resistant to beta-lactamases produced by certain G- rods, including klebsiella, pseudomonas and serratia.
- has no activity against G+ bacteria or anaerobes.
- It is an inhibitor of cell wall synthesis and synergistic with aminoglycosides.
- Administered iv and is eliminated via renal tubular secretion so its t ½ is prolonged in renal failure.
- Adverse effect include gasterointestinal upset with possible superinfection, vertigo and headache, and rare hepatotoxicity.
- Though skin rash may occur, there is no cross allergenicity with penicillins.
B. Imipenem and meropenem:
- They are carbapenems ( chemically different from penicillins but retaining the beta-lactam ring structure) with low susceptibility for beta-lactamases.- The drug have wide activity against
G+ cocci ( including some penicillin resistant pneumococci), G- rods, and
anaerobes.
- It is administered parenterally and is especially useful for infections caused by organisms resistant to other antibiotics.
It is currently the drug of choice for infection due to enterobacter.
- Imipenem is rapidly inactivated by
renal dehydropeptidase I and is administered in fixed combination with cilastatin, an inhibitor of this enzyme.
- Cilastatin increases the plasma t ½ of imipenem and inhibits the formation of a potentially nephrotoxic metabolite.
- Adverse effect of Imipenem-cilastatin include gastrointestinal distress, skin rash, and, at very high plasma levels, CNS toxicity( confusion, encephalopathy, seizures).
- There is partial cross- allerginicity with the penicillins.
-Meropenem is similar to imipenem except that it is not metabolized by renal dehydropeptidase and is less likely to cause seizures.
C. Beta-lactamase Inhibitors:
- Clavulanic acid, sulbactam, and tozabactam are used in fixed combinations with certain hydrolyzable penicillins.
- They are most active against plasmid encoded beta-lactamases such as those produced by gonococci, streptococci , E coli, and H influenzae.
- The are not good inhibitors of inducible chromosomal beta lactamases formed by enterobacter and pseudomonas.