د.علياء طب 13\3\2018
عدد الاوراق( 7 ) م\3\موصل lec:3ALLERGY
Allergic disease can be defined as the clinical manifestation of this inappropriate IgE immune response. affecting between 15% and 20% of the population at some time. They comprise a range of disorders from mild to life-threatening, and affect many organs.
Pathology of allergy
This type I hypersensitivity reaction, An allergic reaction,initial exposure to harmless exogenous substance (known as an allergen) triggers the production of specific IgE antibodies by activated B cells,
Specific IgE antibodies bind to circulating mast cells via high-affinity IgE cell surface receptors.
On re-encounter with allergen, the allergen binds to the IgE antibody-coated mast cells. This triggers mast cell activation with release of vasoactive mediators
Pathology of allergy
Products of mast cell degranulationSusceptibility to allergic diseases
The incidence of allergic diseases is increasing.hygiene hypothesis: It is suggested that the high prevalence of allergic disease is the penalty for the decreased exposure to infection that has resulted from improvements in sanitation and health care.
Familial: A wide array of genetic determinants of disease susceptibility have been identified, including genes controlling innate immune responses, cytokine production, IgE levels and the ability of the epithelial barrier to protect against environmental agents.
Environmental : include bacterial and viral infection, pollutants and cigarette smoke.
Presenting problems in allergy
Common allergic diseases:
• Urticaria
• Angioedema
• Atopic dermatitis
• Allergic conjunctivitis
• Allergic rhinitis (hay fever)
• Allergic asthma
• Food allergy
• Drug allergy
• Allergy to insect venom
• Anaphylaxis
A general approach to the allergic patient
An allergic reaction usually occurs within minutes of exposure and provokes predictable symptoms (angioedema, urticaria, wheezing and so on)
The nature of symptoms should be established and specific triggers identified, along with the predictability of a reaction, and the time lag between exposure to a potential allergen and onset of symptoms.
Potential allergens in the home and workplace should be identified, and a detailed drug history should always be taken,
Investigations
Skin prick tests: A droplet of diluted standardised allergen solution is placed on the forearm and the skin is superficially punctured through the droplet with a sterile lancet. After 15 minutes, a positive response is indicated by a local weal and flare response at least 2 mm larger than the negative control. Antihistamines inhibit the magnitude of the response and should be discontinued before testing; corticosteroids do not influence test results.
Specific IgE tests: quantitation of IgE directed against the putative allergen.
Supervised exposure to allergen (challenge test):These may be particularly useful in the investigation of occupational asthma or food allergy, usually performed in specialist centres.
Mast cell tryptase: Measurement of serum mast cell tryptase is extremely useful in investigating a possible anaphylactic event., serum levels peak at 1–2 hours.
Non-specific markers of atopic disease: total serum IgE and eosinophilia
Skin prick tests
Investigations
Peripheral blood eosinophilia is common in atopic individuals. However, eosinophilia of more than 20% or an absolute eosinophil count over 1.5 × 109/L should initiate a search for a non-atopic cause.Atopy is the most common cause of elevated total IgE in developed countries. However, there are many other causes, including parasite infections, lymphoma , drug reactions.
Significant allergic disease can occur despite a normal total IgE level. Thus total IgE quantitation is not indicated in the routine investigation of allergic disease.
Management
Avoidance of the allergen should be rigorously attempted, and the advice of specialist dietitians and occupational physicians may be required.Antihistamines block histamine H1 receptors, thereby inhibiting the effects of histamine release. Longacting, non-sedating preparations are particularly useful for prophylaxis against frequent attacks.
Corticosteroids down-regulate pro-inflammatory cytokine production. They are highly effective in allergic disease and, if used topically, their adverse effects may be minimised.
Sodium cromoglicate stabilises the mast cell membrane, inhibiting release of vasoactive mediators. It is effective as a prophylactic agent in asthma and allergic rhinitis, but has no role in acute attacks. It is poorly absorbed and therefore ineffective in the management of food allergies.
Management
Antigen-specific immunotherapy involves the sequential administration of escalating amounts of dilute allergen over a prolonged period of time. Its mechanism of action is unknown, but it is highly effective in the prevention of insect venom anaphylaxis, and allergic rhinitis secondary to grass pollen .Omalizumab, a monoclonal antibody against IgE, inhibits the binding of IgE to mast cells and basophils. It is effective in moderate and severe allergic asthma and rhinitis.
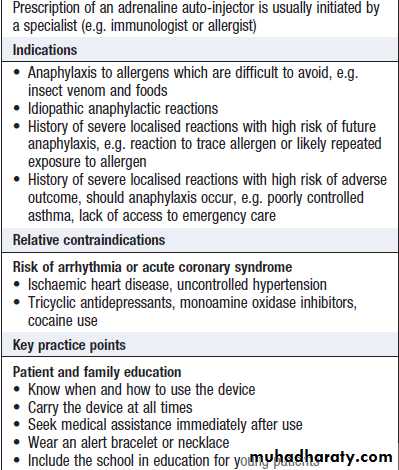
Preloaded self-injectable adrenaline (epinephrine) may be life-saving in acute anaphylaxis.
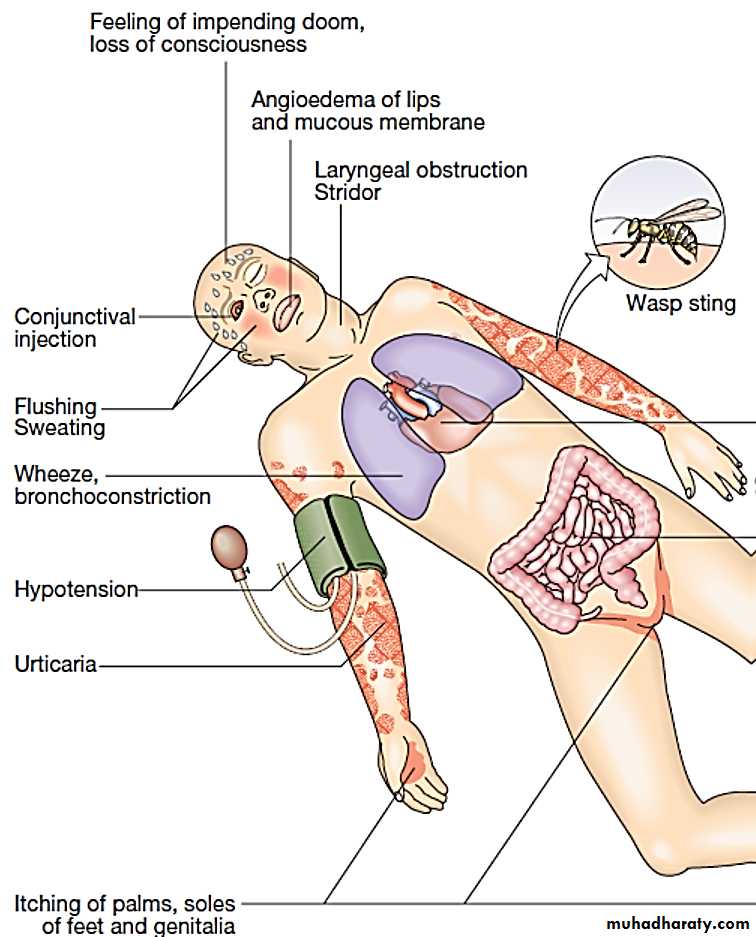
Anaphylaxis
Anaphylaxis is a potentially life-threatening, systemic allergic reaction caused by the release of histamine and other vasoactive mediators from mast cells. The risk of death is increased in patients with pre-existing asthma, particularly if this is poorly controlled, and when treatment with adrenaline (epinephrine) is delayed.
Clinical assessment
Cardiac arrhythmia
DiarrhoeaClinical assessment
The severity of a reaction should be assessed; the time between allergen exposure and onset of symptoms provides a Guide detailed history of the previous 24 hours may be helpful.A history of previous allergic responses to the offending agent is common.
The route of allergen exposure may influence the principal clinical features of a reaction; for example, if an allergen is inhaled, themajor symptom is frequently wheezing.
Features of anaphylaxis may overlap with the direct toxic effects of drugs and venoms
Potentiating factors, such as exercise or alcohol, can lower the threshold for an anaphylactic event.
Differential diagnosis (examples)
Causes of loss of consciousness• Vasovagal syncope
• Cardiac arrhythmias
• Myocardial infarction
Causes of respiratory distress
• Status asthmaticus
Causes of laryngeal obstruction
• C1 inhibitor deficiency
• Idiopathic angioedema
Causes of generalised flushing
• Systemic mastocytosis
• Carcinoid syndrome
Other causes
• Phaeochromocytoma
Common causes of systemic allergic reactions
Investigations and management:
Measurement of serum mast cell tryptase concentrations is useful to confirm the diagnosis.Specific IgE tests may be preferable to skin prick tests when investigating patients with a history of anaphylaxis.
Anaphylaxis is an acute medical emergency.
Individuals who have recovered from an anaphylactic event should be referred for specialist assessment.
Management
Self injectable adrenalineAngioedema
Angioedema is the episodic, localised, non-pitting swelling of submucous or subcutaneous tissues. This most frequently affects the face, extremities and genitalia.Involvement of the larynx or tongue may cause life-threatening respiratory tract obstruction, and oedema of the intestinal mucosa may cause abdominal pain and distension.
In most cases, the underlying mechanism is degranulation of mast cells. However, angioedema may occasionally be mediated by increased local bradykinin concentration
Types of angioedema
1- Allergic reaction to specific trigger.2- Idiopathic angioedema.
3- Hereditary angioedema.
4-ACE-inhibitor associated angioedema
Hereditary angioedema
Hereditary angioedema (HAE), also known as inherited C1 inhibitor deficiency, is an autosomal dominant disorder caused by decreased production or activity of C1 inhibitor protein. This complement regulatory protein inhibits spontaneous activation of the classical complement Pathway.
Patients with HAE generally present in adolescence, but may go undiagnosed for many years. A family history can be identified in 80% of cases.
Hereditary angioedema
angioedema may be spontaneous or triggered by local trauma or infection. Multiple parts of the body may be involved, especially the face, extremities upper airway and gastrointestinal tract.
The most important complication is laryngeal obstruction, often associated with minor dental procedures, which can be fatal. Episodes of angioedema are self-limiting and usually resolve within 48 hours.
Severe acute attacks should be treated with purified Cl inhibitor or a bradykinin receptor antagonist
Specific allergies
Insect venom allergy: Local non-IgE-mediated reactions to insect stings are common and may cause extensive swelling around the site lasting as long as 7 days. These usually do not require specific treatment.
Peanut allergy: Peanut allergy is the most common food-related allergy. More than 50% of patients present before the age of 3 years and some individuals react to their first known exposure to peanuts.
Birch oral allergy syndrome: This syndrome is characterised by a combination of birch pollen hay fever and local angioedema after contact with fresh fruit (especially apples), vegetables and nuts. Cooked fruits and vegetables are tolerated.
TRANSPLANTATION IMMUNOLOGY
Transplantation provides the opportunity for definitive treatment of end-stage organ disease.The major complications are graft rejection, drug toxicity and infection consequent on immunosuppression.
Transplant rejection
Solid organ transplantation inevitably stimulates an aggressive immune response by the recipient, unless the transplant is between monozygotic twins.
The type and severity of the rejection response are determined by the genetic disparity between the donor and recipient, the immune status of the host and the nature of the tissue transplanted
The most important genetic determinant is the difference between donor and recipient HLA proteins
Classification of transplant rejection
Acute cellular rejection is the most common form of graft rejection. It is mediated by activated T cells and results in deterioration in graft function. It may cause fever, pain and tenderness over the graft. It is usually amenable to increased immunosuppressive therapy.
Hyperacute rejection results in rapid and irreversible destruction of the graft. It is mediated by preexisting recipient antibodies against donor HLA antigens, which arise as a result of previous exposure through transplantation, blood transfusion.
Classification of transplant rejection
Acute vascular rejection is mediated by antibody formed de novo after transplantation. It is more curtailed than the hyperacute response because of the use of intercurrent immunosuppression, but it is also associated with reduced graft survival. Aggressive immunosuppressive therapy is indicated, and physical removal of antibody through plasmapheresis may be effective.
Chronic allograft failure, also known as chronic rejection, is a major cause of graft loss. It is associated with proliferation of transplant vascular smooth muscle, interstitial fibrosis and scarring. The pathogenesis is poorly understood but contributing factors include immunological damage caused by h hypertension, hyperlipidaemia and chronic drug toxicity.
Investigations
Pre-transplantation testing: HLA typing determines an individual’s HLA polymorphisms and facilitates donor–recipient matching.
Donor–recipient cross-matching is a functional assay that directly tests whether serum from a recipient (which potentially contains anti-donor antibodies) is able to bind and/or kill donor lymphocytes. It is specific to a prospective donor–recipient pair and is done immediately prior to transplantation.
prevention of transplant rejection
Prevention requires indefinite treatment with immunosuppressive agents. In general, two or more immunosuppressive drugs are used in synergistic combinations in order to minimize drug side effects
prevention of transplant rejection
The major complications of long-term immunosuppression areInfection: The risk of some opportunistic infections may be minimized through the use of prophylactic medication (e.g. ganciclovir for CMV prophylaxis and trimethoprim– sulfamethoxazole for Pneumocystis prophylaxis). Immunisationwith killed vaccines is appropriate,
malignancy. The increased risk of malignancy arises because T-cell suppression results in failure to control viral infections. Virus-associated tumours include lymphoma (associated with EBV), Kaposi’s sarcoma (associated with human herpesvirus 8) and skin tumours (associated with human papillomavirus).