Emberyology
Dr.Muna ZuhairLec. 3
Urogenital System
Urinary System(1). Kidneys.
(4). Urethra.(3). Urinary Bladder.
(2). Ureters.
(5). Prostate.
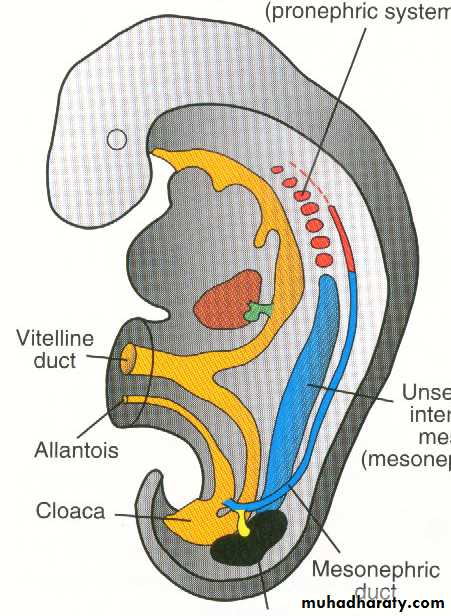
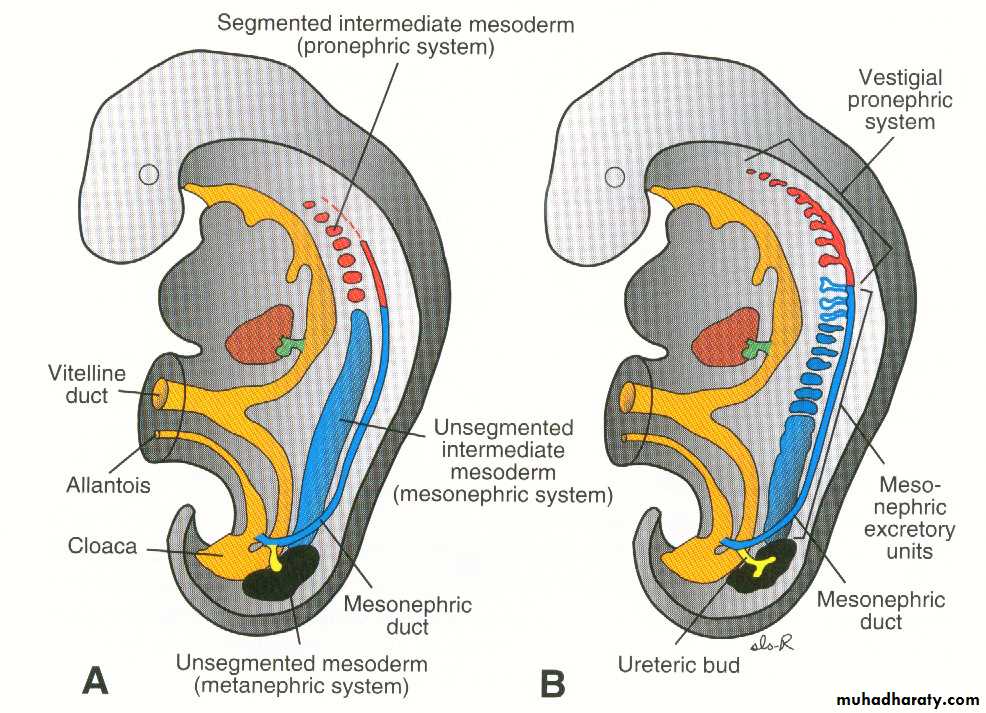
The kidneys of the fetus passes through 3 stages of development :
• Pronephros.• Mesonephros.
• Metanephros.
All developed from the intermediate cell mass of mesoderm (nephrogenic cord).
These 3 stages appear one after the other in time and one caudal to the other in position.The earlier stage degenerates or become transformed into some form of ducts before the appearance of the succeeding stage.
Develops in the cervical region from the cranial part of the nephrogenic cord which is broken up into several segments one caudal to the other called nephrotomes (7-10 in number).
Each segment is converted into hollow elongated tubule called pronephric tubule which lies transversely having a medial and lateral ends.
Medial end is expanded and opens into the coelomic (peritoneal) cavity while the lateral end is tubula and curves caudally to open into the corresponding part of the succeeding tubule.By this arrangement a longitudinal duct (pronephric duct) is formed along the lateral side of the pronephros
Fate of Pronephros:
• The pronephric tubules degenerates compleletely.
• The pronephric duct persists to be used by the succeeding stage of mesonephros where it is transformed into the mesonephric duct.
It arise from the part of the nephrogenic cord caudal to the part which has developed into pronephros ( upper thoracic to upper lumber segment).
• Mesonephros.
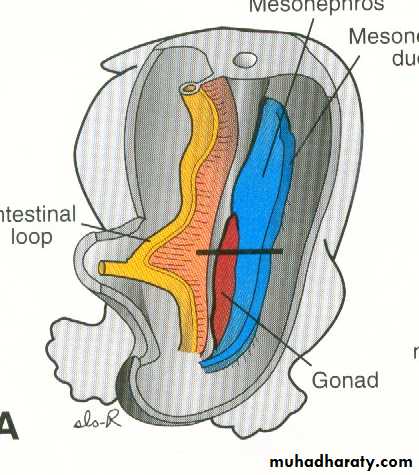
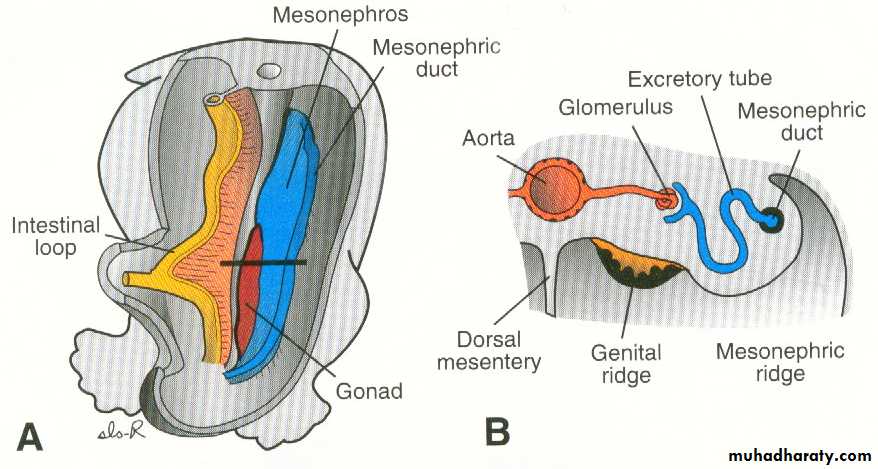
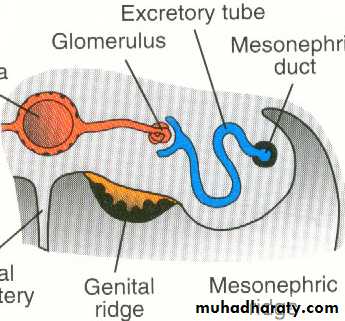
• Similarly , the mesoderm of the cord is segmented and each segment is transformed into a hollow tubule called mesonephric tubule which lie transversely one caudal to the other (as the pronephric tubules).
• Each mesonephric tubule become S-shaped with an expanded medial end and a narrow tubular lateral end.
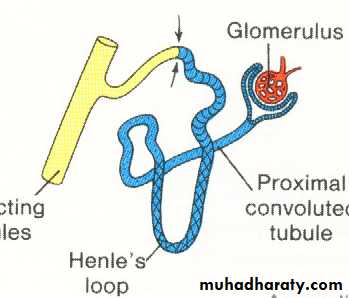
• The medial end become invaginated (indented) by capillaries from the dorsal aorta to form the internal glomerulus then the tubule form Bowman's capsule so the capsule +glomerulus form the renal corpuscle.
• The lateral end joins the pronephric duct and become termed mesonephric duct (Wolffian duct) which runs along the lateral side of mesonephros.
The mesonephros forms a mass which bulge into the coelomic cavity as an ovoid mass on each side of midline +developing gonads forming a ridge called urogenital ridge.
Fate of mesonephros:
• Fate of mesonephric tubules:
Most of the cranial tubules degenerate while at the same time the caudal tubules are differentiating.
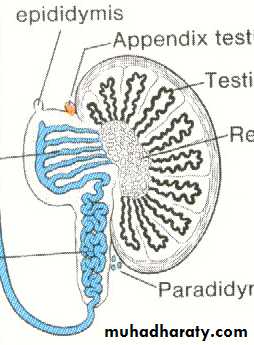
• In male it gives:
• Efferent ductules of testis.• Paradidymis(rudimentary tubule on the side of testis).
• Aberrant ductules.
• In female it gives:
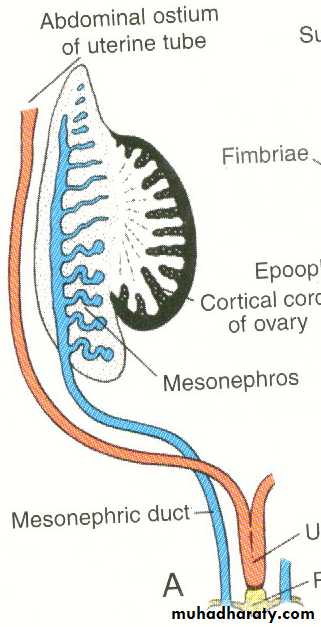
• Tubules of epoophoron
• Paroophoron.
Fate of mesonephric duct (Wolffian duct):
• In male it gives:
• Duct of epididymis.
• Ductus deferens (vas deferens).
• Ejaculatory duct.
• Seminal vesicle.
• Its blind cranial (upper) end form the appendix of epididymis.
• In female:
Most of the duct disappear and only a small segment in its cranial part persist as duct of epoophoron.
• In both sexes:
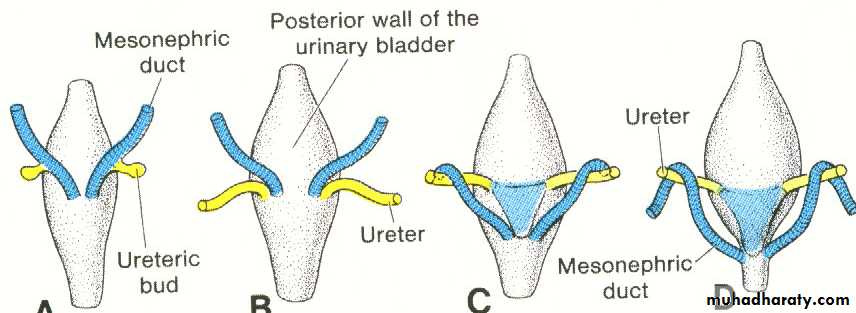
• The lower end of the duct gives the ureteric bud.• The part caudal to the uretric bud is absorbed into the urogenital sinus to form posterior part of the bladder wall (trigon) and upper post. wall of prostatic urethra.
Metanephros
(1). Collecting System (ureteric bud).(2). Excretory System (metanephric cap).
permanent kidney
Metanephros (Permanent kidney):
It develops from 2 sources:
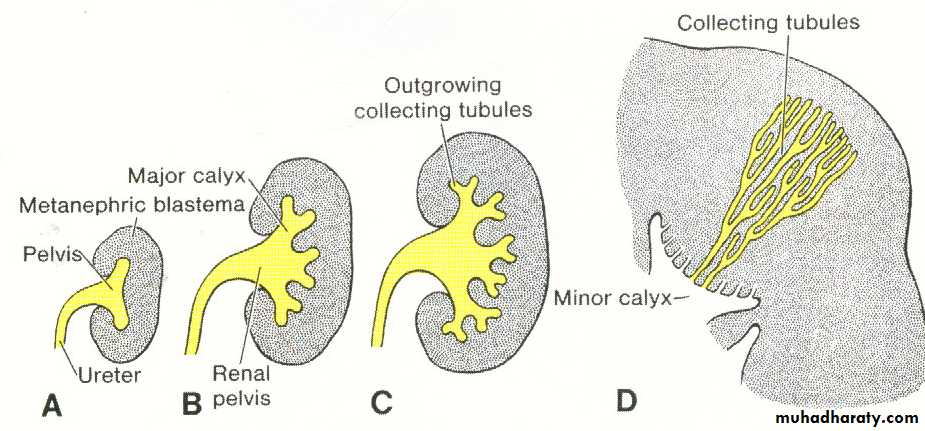
Uretric bud: forms the collecting tubule of the kidney (in addition to the ureter and its calyces.
Metanephric cap (blstema): forms the whole nephrons.
Development:
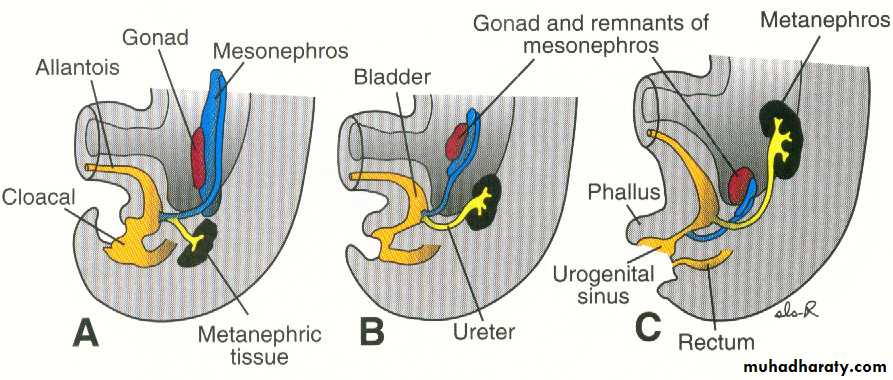
• The uretric bud arise as a diverticulum from the lower end of the mesonephric duct close to cloaca. Its free end expand and come to lie in contact with the metanephric cap which lies in the pelvic region at this time (the cap is the caudal part of the mesoderm of the nephrogenic cord).
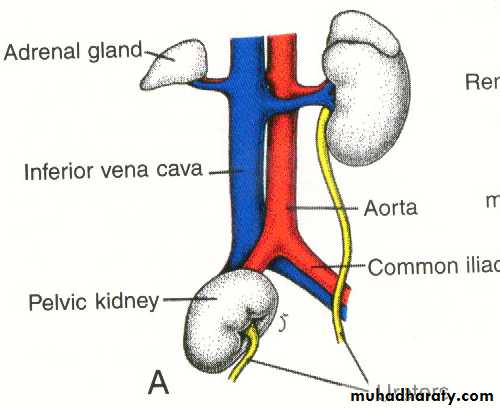
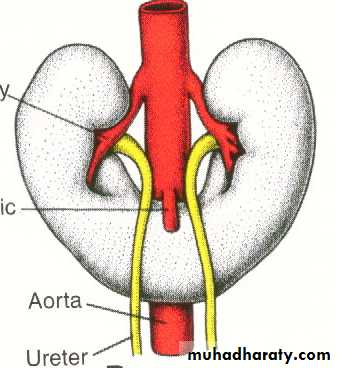
• Elongation of the uretric bud will push the metanenephric cap cranially(ascent of the kidney) to reach the level of the upper lumber segments(adult position of the kidney).
• The cranial end of the uretric bud divides repeatedly to form the major and minor calyces as well as the collecting tubules of the kidney(1-3 milion). The successive generations of the tubules elongated and converge on the minor calyx forming (renal pyramid).
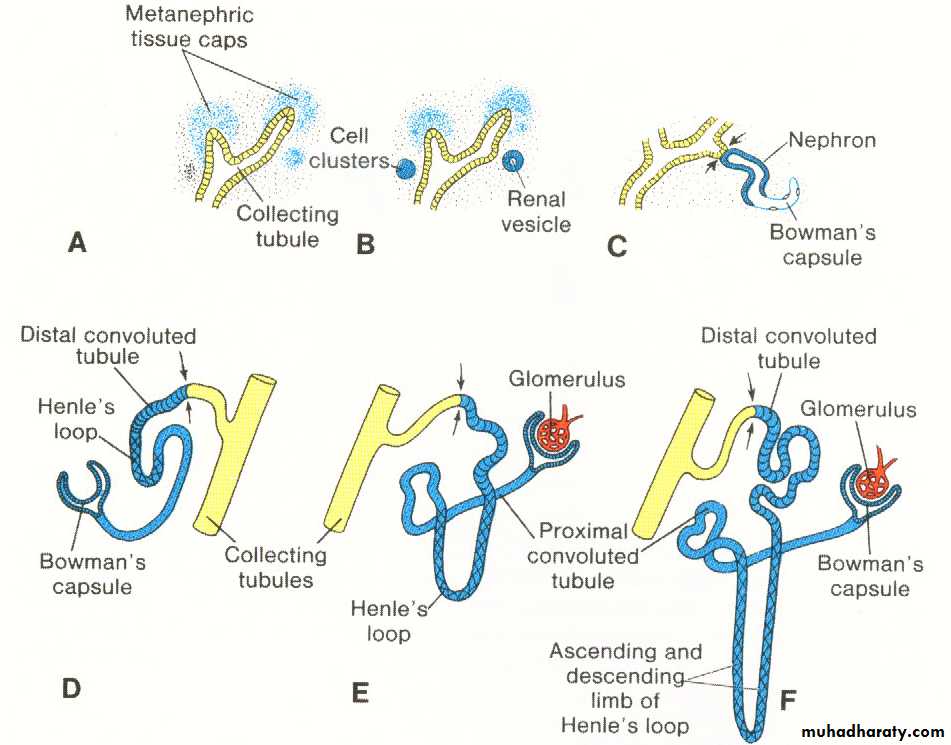
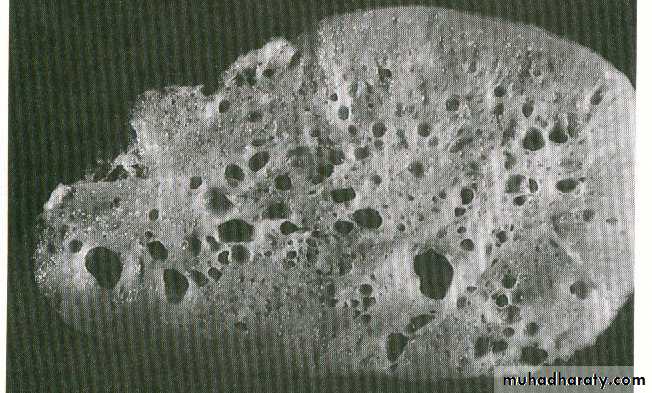
Each collecting tubule become covered by a separate small mass of mesoderm of the metanephric cap, this solid small mass is canalized and become S-shaped tubule called metanephric tubule which elongates and become much convoluted with 2 ends one open into the collecting tubule while the other end expanded and invaginated by a tuft of capillaries to form the renal corpuscle thus forming the nephrons of the kidney.The kidney is lobulated at first later on, the lobulation will disappear during 1st year after birth.
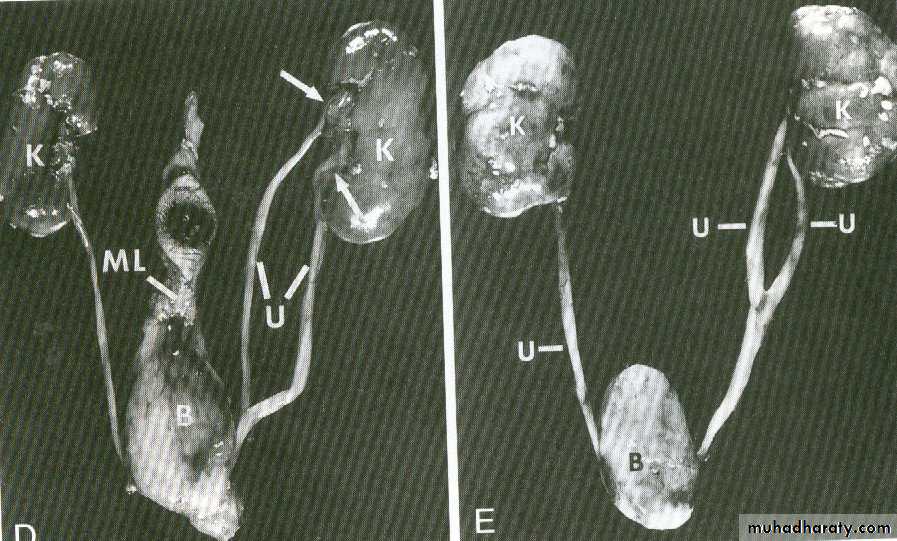
Congenital anomalies of the metanephros:
• Renal agenesis: complete absence of one or 2 kidney associated with oligohydramnios.
• Horse-shoe kidney: due to fusion of the 2 metanephric cap together at their lower pole in the median plane.
• Pelvic kidney: due to failure of the kidney to ascend, it remains in the pelvis close to the common iliac artery.
• Congenital cystic kidney: due to failure of communication between the metanephric tubules with the collecting tubule could be solitary or multiple cysts.
Position of the kidney
The Ureter:
It is formed from the uretric bud which arise at the lower end of the mesonephric duct close to the cloaca. It then grows dorsally and cranially to come in contact with the metanephric cap and ascend up together to reach the level of the 2nd lumber vertebra.The upper end of the bud divide repeatedly to form:Pelvis of the ureter.
Major and minor calyces.
Collecting tubule of the kidney.
It shows 2 fusiform dilatations along its length, one affects its abdominal part and the other affects its pelvic part.As a consequence, the lumen of the ureter shows number of relative constrictions at the ends of the dilatation as follows:
At the pelvi-uretic junction.
At the point where it cross the pelvic brim.
As it enters the bladder(intramural part).
By absorption of the caudal part of the mesonephric duct into the wall of the urogenital sinus , the ureter is freed from the duct and comes to open directly into the bladder.
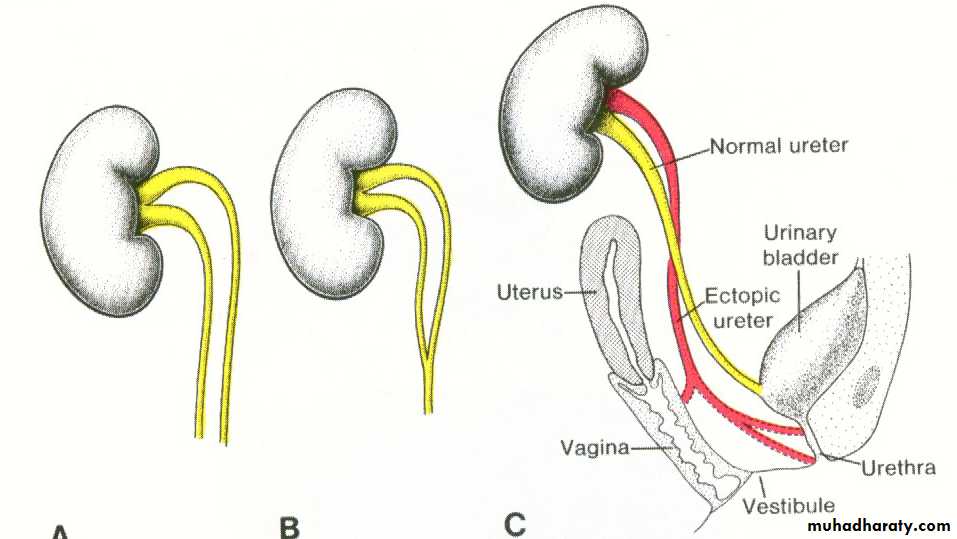
Anomalies of the ureter:
Double ureter: complete or partial duplication, 2 uretric buds develop from the mesonephric duct.Bifid ureter or cleft pelvis of the ureter.
Ectopic uretral opening in the vagina, vestibule or urethra.
The cloaca:
It is the dilated lower part of the hindgut just caudal to the point of connection of the allantois.Development:
The mesoderm at the angle between the allantois and the cloaca proliferates to form the urorectal septum which descends towards the cloacal membrane, thus dividing the cloaca into 2 parts:
Rectum and upper part of anal canal dorsally.
Urogenital sinus (with the allantois attached to it ventrally , it is termed primitive urogenital sinus.
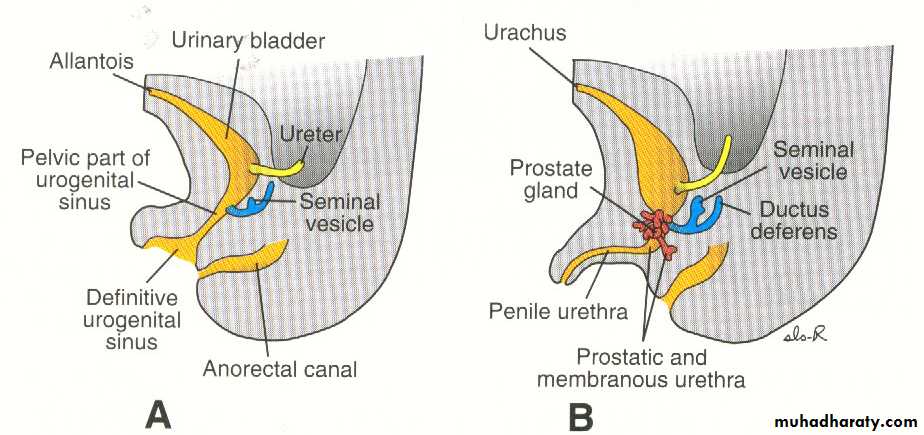
The primitive urogenital sinus is subdivided by the point of entrance of the mesonephric ducts into 2 parts:
• Vesicourethral canal: is the cranial part which has the allantois attached to its apex. It forms the following:
• Urinary bladder except the trigon.
• Upper part of the prostatic urethra in male.
• The whole urethra in female.
2. Definitive urogenital sinus: Its upper (cranial) segment is phallic part. It forms the following:
Most of the male urethra (lower 1/2 of prostatic part, whole of the membranous part and most of the spongy part).
Vestibule of the vagina in female.
Urinary bladder:
It develops from 2 sources :
Vesico urethral canal : endodermal
Lower parts of the mesonephric ducts : mesodermal.
Development:
The lower parts of the 2 mesonephric ducts are incorporated (absorbed) into the back of the bladder to form the trigone. The results of this incorporation:
• Ureter enters the bladder separately and freed from the duct.
• Formation of the trigone.
• Ascend of the kidney: uretric openings move cranially at the upper angles of trigone.
• Openings of the mesonephric duct enter the prostatic urethra and become ejaculatory duct.
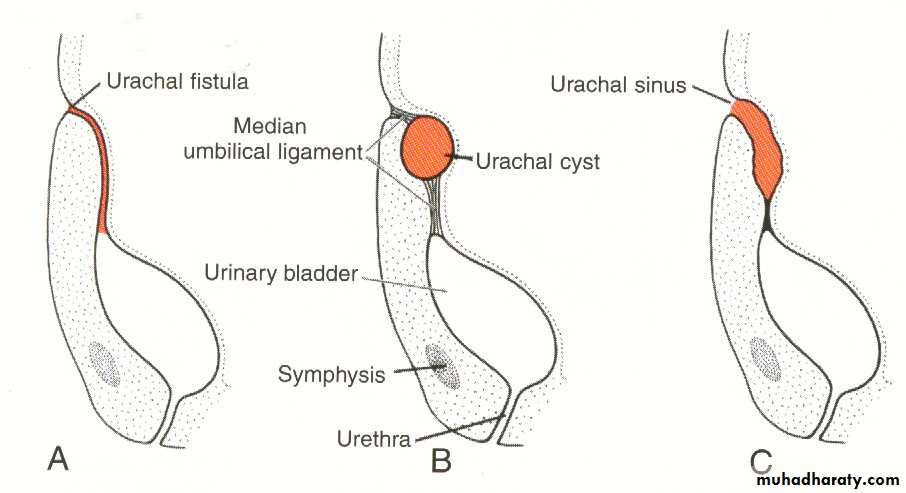
The allantois which is continuous with the apex of the bladder become a narrow canal called urachus which extends up to the umbilicus.In the adult it becomes fibrosed to form the median umbilical ligament.
Congenital anomalies of the urinary bladder:
Ectopic Vesicae: opening of the bladder cavity onto the surface just above the symphysys pubis due to failure of formation of the anterior wall of the bladder.Persistence of a patent urachus: lumen of the allantois persist.
• Urachal fistula connecting the urinary bladder to the umbilicus due to patent whole urachus.
• Urachal cyst: due to patent segment of urachus.
• Urachal sinus: lumen of upper part of allantois only persist.
Urethra:
Development:Upper half of the postatic urethra (above the openings of the ejaculatory ducts) is developed from:
Lower part of the vesico-urethral canal.
Absorbed part of the mesonephric duct form the posterior wall of this part.
Lower part of prostatic urethra (Below the opening of the ejaculatory duct) is derived from the pelvic part of the definitive urogenital sinus.
Membranous urethra: is derived from the pelvic part of the definitive urogenital sinus.
Spongy urethra : is developed from the phallic part of the definitive urogenital sinus.
Congenital anomalies:
• Hypospedias: when the urethra opens on the under surface of the penis.
• Epispedias: where the urethra opens on the dorsum of penis.
• Urethral stenosis (stricture): due to incomplete canalization.
Thank you
EmberyologyDr.Muna Zuhair
Lec. 2
Respiratory System
Emberyology
Dr.Muna Zuhair
Lec. 4
Genital System
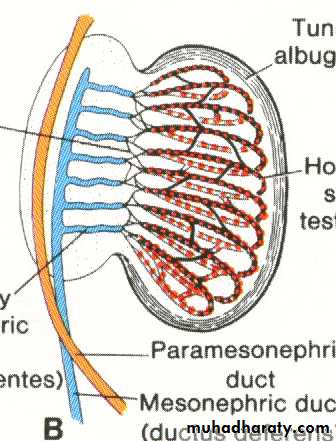
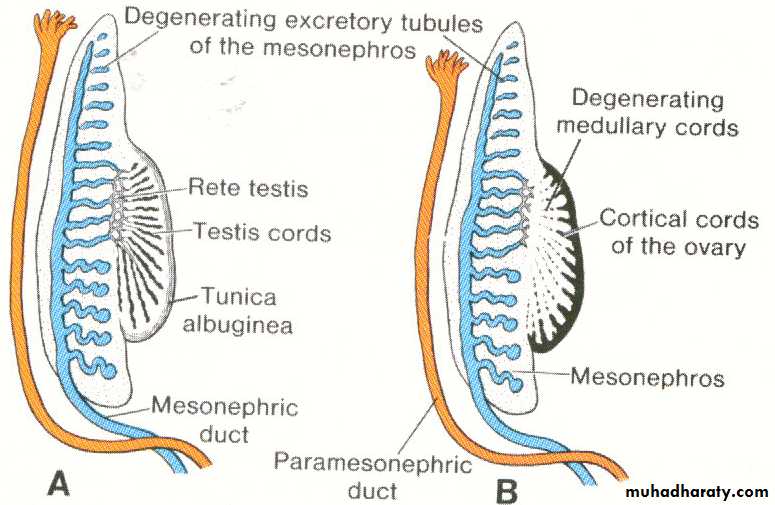
Development of testis:
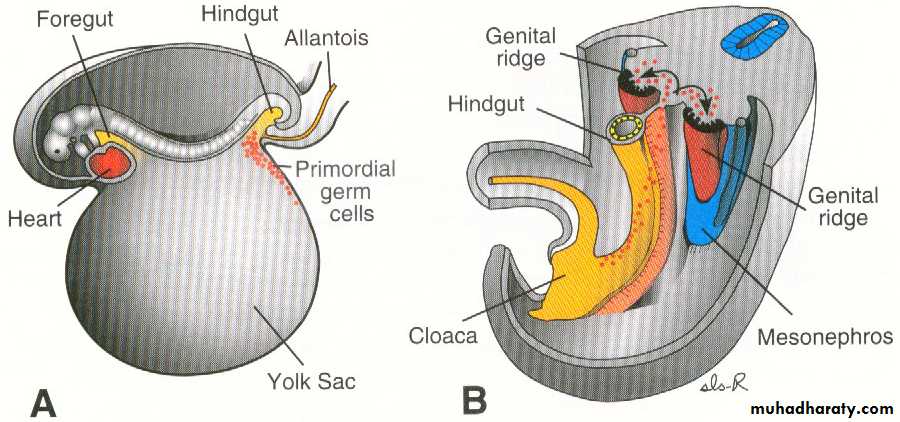
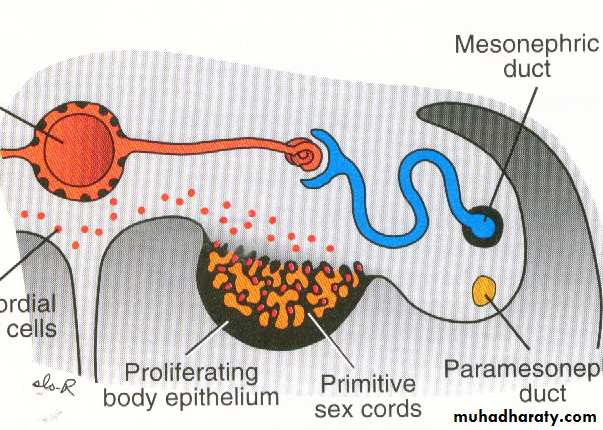
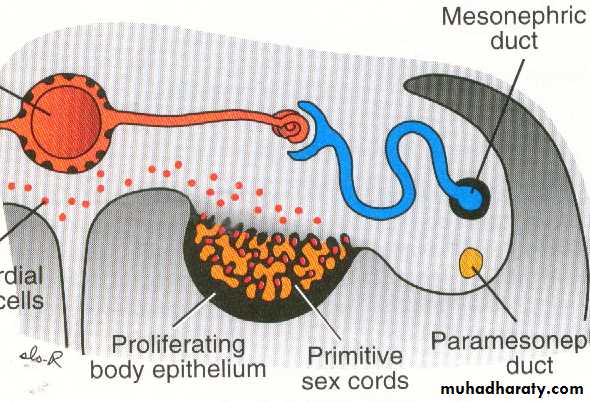
• The gonads appear as a pair of longitudinal ridge called genital ridge.• The primordial germ cells appear in the wall of yolk sac and migrate to reach the gonads at 5th week and invade the epithelium of the genital ridge which proliferate to form primitive sex cords.
The testis develops from 3 sources:
Coelomic epithelium: give rise to Sertoli cells.Primordial germ cells : give rise to spermatogonia.
Intermediate cell mass of mesoderm: forms the connective tissue of testis and its covering tunica albuginea.
The primitive sex cords continue to proliferate and enter the medulla forming medullary cords (testis cords) formed from germ cells and Sertoli cells then become separated from the surface by tunica albuginea forming horse-shoe shaped testis cords, then undergo canalization to form the seminiferous tubules.
Descent of testis:
• The testis descends from its higher position on the posterior abdominal wall to enter the scrotom.Its descend is guided and facilitated by a fibrous cord called gubernaculum which extends from the lower pole of testis to the floor of the scrotal pouch.• The gubernaculum traverses the muscles of the anterior abdominal wall (in the inguinal canal) to reach the scrotom where it is accompanied by an evagination of peritoneal sac called Processus vaginalis which follow the course of gubernaculum to the scrotal swelling.
• Shortening of the gubernaculum together with lengthening of the embryo will help in the descent of testis.It descend retroperitoneally to enter:The inguinal canal : at 7th month.Inside the scrotom: at birth (or in the 9th month).
• The canal connecting processus vaginalis with the peritoneal cavity obliterated .
Congenital anomalies:
• Indirect inguinal hernia: due to patent processus vaginalis or it become filled with peritoneal fluid forming (congenital hydrocele).• Undescended testis : due to failure of descent of testis which may retained in the abdomen or may stop at : superficial inguinal ring, Root of penis, perineum.
• Ectopic testis: the testis may take a position away from the normal pathway of descent as to be found in the lower part of anterior abdominal wall or upper part of thigh.
• Gonadal dysgenesis: failure of formation of genital duct and external genital organ.
• Hermaphroditism (intersex):
• True hermaphroditism- gonads +external genetalia of both sexes
• Pseudo hermaphroditism-gonads of one sex+external genetalia of the opposite sex.
Anomalies of the processus vaginalis:
It may remain patent in the whole or in part leading to the following:• Congenital hydrocele.
• Congenital inguinal hernia.
• Cyst in the spermatic cord.
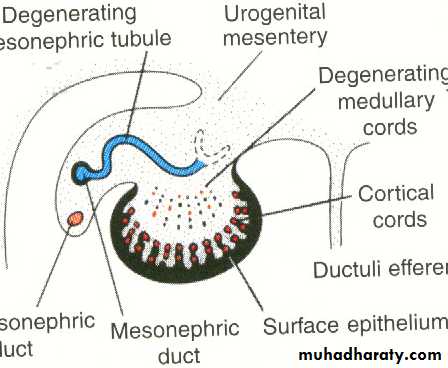
Development of the ovary:
• The primitive sex cords dissociate forming degenerating medullary cords which disappear and replaced by vascular stroma (ovarian medulla).
• The germinal epithelium proliferate together with the primordial germ cells form cortical cords which become divided into isolated cell clusters called (primordial follicles). Each follicle is formed from oogonia surrounded by a single layer of follicular cells.
Thus the ovary develops from 3 sources:
Coelomic epithelium (germinal epithlium): forms the follicular cells.Primordial germ cells : give rise to oogonia.
Intermediate cell mass of mesoderm: forms the stroma of the ovary and its covering tunica albuginea.
Descent of ovary:
The ovary is attached by gubenaculum which traverse the anterior abdominal wall in the inguinal canal to reach the labium majus and it get attachment to the side of the uterus close to the entrance of uterine tube and as a result it become divided into 2 parts:Cranial part: forms the ligament of the ovary (between the uterus and ovary).
Caudal part : forms the round ligament of uterus (between the uterus and labium majus).
Paramesonephric duct:
Development:
Two longitudinal ducts one on each side and descend very close to Mesonephric (Wollfian duct).Each duct has 2 ends:
• Cranial end: open into the coelomic (peritoneal) cavity.
• Caudal end: blind and comes in contact with the posterior wall of the definitive urogenital sinus.
Its course divided into 3 patrs:
Cranial part: descend vertically lateral to the mesonephros.Intermediate part : crosses transversely (horizontally) ventral to the mesonephric duct.
Caudal part: descends vertically medial to the mesonephric duct.
The caudal vertical parts of both ducts descend in contact with each other inside a mesodermal partition called genital cord. This cord extends between the rectum posteriorly and urinary bladder anteriorly and its mesoderm differentiates into the fibromuscular wall of the uterus and vagina (not its epithelial lining).
Fate of Paramesonephric duct:
In the female :• The cranial vertical part : form uterine tube with its cranial end opening into the coelomic cavity
• The intermediate transverse part: form the fundus and upper part of the body of the uterus.
• The caudal fused vertical parts of both sides: forms the lower part of the body of uterus and cervix.
In the male:
The duct disappears almost completely except for 2small parts at its ends:
Cranial end : form the appendix of testis.
Caudal end: form the prostatic utricle.
In contrast to the paramesonephric duct, the mesonephric duct disappears completely in female but persist in the male.
Female genital organs:
Uterine tube:
Each tube is developed from the cranial vertical part of the paramesonephric duc. The cranial end of the duct will become the limbricated end of the uterine tube which persist communicating with the peritoneal cavity.
Uterus:
The fundus and upper part of the body of uterus: develop from the intermediate transverse parts of the paramesonephric ducts.
The cervix and lower part of the body of uterus: develop from the fused caudal vertical parts of the 2 paramesonephric ducts which extend inside the genital cord.
Anomalies of uterus:
• Uterus didelphys (double uterus): the 2 paramesonephric ducts fail to fuse completely in the genital cord where each duct forms a separate uterus and each one has a separate vagina.• Uterus bicornis bicollis: double uterus with double cervix but with a single vagina.
• Bipartite uterus: The caudal part s of the 2paramesonephric duct fuse together but the septum in between persist and thus there is a single uterus with its cavity divided into 2 parts by a septum .
• Bicornuate uterus: The uterus is single but has 2 separate horns due to improper development of the fundus.
Development of the vagina:
The caudal vertical part of the 2 paramesonephric ducts come in contact with the dorsal wall of the definitive urogenital sinus to produce a bulge into the cavity of the sinus called Mullerian tubercle.At the point where the Mullerian tubercle lies, the endodermal cells lining the urogenital sinus proliferate to form 2 masses called sino-vaginal bulbs which fuse together to form the vaginal plate.
The vaginal plate grows cranially then become canalized to form the lumen of the vagina. Expansion of the lumen forms:
• Vaginal fornices around the cervix at the cranial end of the vagina.
• The hymen at the caudal end of the vagina.
Anomalies:
• Absent vagina: due to failure of canalization of the vaginal plate.
• Imperforated hymen: when the continuity between the vaginal lumen and the cavity of urogenital sinus is not established.
Prostate gland:
It develops as multiple (15-20) outgrowths (buds) from the lining of the prostatic urethra (caudal part of the vesicourethral canal and pelvic part of the urogenital sinus). They arise mainly from the lateral aspect of the urethra, although few buds also arise from its dorsal and ventral aspect.The lining of the prostatic urethra is mainly endodermal except in its posterior wall which is mesodermal and therefore, the prostatic buds are mostly endodermal (except posteriorly). The cellular buds become canalized to form the alveoli and tubules of the prostate.
The fibromuscular capsule and the connective tissue of the gland are derived from the surrounding mesoderm in the genital cord.