المرحلة الخامسة / مجموعة A
DERMATOLOGY د.مازن خالدP s o r i a s i s
is an autoimmune disease that appears on the skin. It occurs when the immune system mistakes the skin cells as a pathogen, and sends out faulty signals that speed up the growth cycle of skin cells. Psoriasis is not contagious. There are five types of psoriasis: plaque, guttate, inverse, pustular and erythrodermic. The most common form, plaque psoriasis, is commonly seen as red and white hues of scaly patches appearing on the top first layer of the epidermis (skin). Some patients, though, have no dermatological symptoms.
In plaque psoriasis, skin rapidly accumulates at these sites, which gives it a silvery-white appearance. Plaques frequently occur on the skin of the elbows and knees, but can affect any area, including the scalp, palms of hands and soles of feet, and genitals. In contrast to eczema, psoriasis is more likely to be found on the outer side of the joint.
The disorder is a chronic recurring condition that varies in severity from minor localized patches to complete body coverage. Fingernails and toenails are frequently affected (psoriatic nail dystrophy) and can be seen as an isolated symptom. Psoriasis can also cause inflammation of the joints, which is known as psoriatic arthritis. Between 10-30% of all people with psoriasis also have psoriatic arthritis.
The cause of psoriasis is not fully understood, but it is believed to have a genetic component and local psoriatic changes can be triggered by an injury to the skin known as the Koebner phenomenon . Various environmental factors have been suggested as aggravating to psoriasis, including stress, withdrawal of systemic corticosteroid, as well as other environmental factors, There are many treatments available, but because of its chronic recurrent nature, psoriasis is a challenge to treat. Withdrawal of corticosteroids (topical steroid cream) can aggravate the condition due to the 'rebound effect' of corticosteroids but this may be followed by cure.
Classification
Psoriasis is a chronic relapsing disease of the skin that may be classified into nonpustular and pustular types as follows :
Nonpustular
Psoriasis vulgaris ( plaque-like psoriasis) is the most common form of psoriasis. It affects 80 to 90% of people with psoriasis. Plaque psoriasis typically appears as raised areas of inflamed skin covered with silvery white scaly skin. These areas are called plaques.
Psoriatic erythroderma (erythrodermic psoriasis involves the widespread inflammation and exfoliation of the skin over most of the body surface. It may be accompanied by severe itching, swelling and pain. It is often the result of an exacerbation of unstable plaque psoriasis, particularly following the abrupt withdrawal of systemic treatment. This form of psoriasis can be fatal, as the extreme inflammation and exfoliation disrupt the body's ability to regulate temperature and for the skin to perform barrier functions.
Pustular
Pustular psoriasis appears as raised bumps that are filled with noninfectious pus (pustules). The skin under and surrounding the pustules is red and tender. Pustular psoriasis can be localised, commonly to the hands and feet (palmoplantar pustulosis), or generalised with widespread patches occurring randomly on any part of the body. Types include:Generalized pustular psoriasis (pustular psoriasis of von Zumbusch)
Pustulosis palmaris et plantaris (persistent palmoplantar pustulosis, pustular psoriasis of the Barber type, pustular psoriasis of the extremities)
Annular pustular psoriasis
Acrodermatitis continua
Impetigo herpetiformis
Other
Additional types of psoriasis include
Drug-induced psoriasis
Inverse psoriasis (flexural psoriasis, inverse psoriasis)( appears as smooth inflamed patches of skin. It occurs in skin folds, particularly around the genitals (between the thigh and groin), the armpits, under an overweight abdomen ( HYPERLINK "http://en.wikipedia.org/wiki/Panniculus" \o "Panniculus" panniculus), and under the breasts ( HYPERLINK "http://en.wikipedia.org/wiki/Inframammary_fold" \o "Inframammary fold" inframammary fold). It is aggravated by friction and sweat, and is vulnerable to fungal infections.
Napkin psoriasis
Seborrheic-like psoriasis
Guttate psoriasis ( is characterized by numerous small, scaly, red or pink, teardrop-shaped lesions. These numerous spots of psoriasis appear over large areas of the body, primarily the trunk, but also the limbs and scalp. Guttate psoriasis is often preceded by a streptococcal infection, typically streptococcal pharyngitis. The reverse is not true.
Nail psoriasis produces a variety of changes in the appearance of finger and toe nails. These changes include discolouring under the nail plate, pitting of the nails, lines going across the nails, thickening of the skin under the nail, and the loosening ( HYPERLINK "http://en.wikipedia.org/wiki/Onycholysis" \o "Onycholysis" onycholysis) and crumbling of the nail.
Psoriatic arthritis involves joint and connective tissue inflammation. Psoriatic arthritis can affect any joint, but is most common in the joints of the fingers and toes. This can result in a sausage-shaped swelling of the fingers and toes known as dactylitis. Psoriatic arthritis can also affect the hips, knees and spine (spondylitis). About 10–30% of people who have psoriasis also have psoriatic arthritis.
The migratory stomatitis in the oral cavity mucosa and the geographic tongue that confined to the dorsal and lateral aspects of the tongue mucosa, are believed to be oral manifestations of psoriasis, as being histologically identical to cutaneous psoriasis lesions and more prevalent among psoriasis patients , although these conditions are quite common in the non-psoriatic population, affecting 1% to 2.5% of the general population.
Signs and symptoms
Plaque of psoriasis
Plaque of psoriasis
An arm covered with plaque psoriasis
Psoriasis of a fingernail
Quality of lifeDepending on the severity and location of outbreaks, individuals may experience significant physical discomfort and some disability. Itching and pain can interfere with basic functions, such as self-care, walking, and sleep. Plaques on hands and feet can prevent individuals from working at certain occupations, playing some sports, and caring for family members or a home. Plaques on the scalp can be particularly embarrassing, as flaky plaque in the hair can be mistaken for dandruff. Medical care can be costly and time-consuming, and can interfere with an employment or school schedule.
Psychological distress can lead to significant depression and social isolation.
Severity
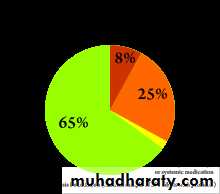
Distribution of severity among people with psoriasis
Psoriasis is usually graded as mild (affecting less than 3% of the body), moderate (affecting 3–10% of the body) or severe. The degree of severity is generally based on the following factors: the proportion of body surface area affected; disease activity (degree of plaque redness, thickness and scaling); response to previous therapies; and the impact of the disease on the person.The Psoriasis Area Severity Index (PASI) is the most widely used measurement tool for psoriasis. PASI combines the assessment of the severity of lesions and the area affected into a single score in the range 0 (no disease) to 72 (maximal disease).
Cause
The cause of psoriasis is not fully understood. There are two main hypotheses about the process that occurs in the development of the disease. The first considers psoriasis as primarily a disorder of excessive growth and reproduction of skin cells. The problem is simply seen as a fault of the epidermis and its keratinocytes. The second hypothesis sees the disease as being an immune-mediated disorder in which the excessive reproduction of skin cells is secondary to factors produced by the immune system. T cells (which normally help protect the body against infection) become active, migrate to the dermis and trigger the release of cytokines (tumor necrosis factor-alpha TNFα, in particular) which cause inflammation and the rapid production of skin cells. It is not known what initiates the activation of the T cells.
The immune-mediated model of psoriasis has been supported by the observation that immunosuppressant medications can clear psoriasis plaques.
Psoriasis is a fairly idiosyncratic disease. The majority of people's experience of psoriasis is one in which it may worsen or improve for no apparent reason. Conflicting findings are often reported. Nevertheless, the first outbreak is sometimes reported following stress (physical and mental), skin injury, and streptococcal infection. Conditions that have been reported as accompanying a worsening of the disease include infections, stress, and changes in season and climate. Certain medicines, including lithium salt, beta blockers and the HYPERLINK "http://en.wikipedia.org/wiki/Antimalarial_drug" \o "Antimalarial drug" antimalarial drug chloroquine have been reported to trigger or aggravate the disease. Excessive alcohol consumption, smoking and obesity may exacerbate psoriasis or make the management of the condition difficult or perhaps these comorbidities are effects rather than causes.
Individuals suffering from the advanced effects of the human immunodeficiency virus, or HIV, often exhibit psoriasis. This presents a paradox to researchers, as traditional therapies that reduce T-cell counts generally cause psoriasis to improve. Yet, as CD4-T-cell counts decrease with the progression of HIV, psoriasis worsens. In addition, HIV is typically characterized by a strong Th2 cytokine profile, whereas psoriasis vulgaris is characterized by a strong Th1 secretion pattern. It is hypothesized that the diminished CD4-T-Cell presence causes an overactivation of CD8-T-cells, which are responsible for the exacerbation of psoriasis in HIV positive patients.
Genetics
Psoriasis has a large hereditary component, and many genes are associated with it, but it is not clear how those genes work together. Most of them involve the immune system, particularly the major histocompatibility complex (MHC) and T cells. The main value of genetic studies is they identify molecular mechanisms and pathways for further study and potential drug targets.
Classic genomewide linkage analysis has identified nine locations (loci) on different chromosomes associated with psoriasis. They are called psoriasis susceptibility 1 through 9 (PSORS1 through PSORS9). Within those loci are genes. Many of those genes are on pathways that lead to inflammation. Certain variations (mutations) of those genes are commonly found in psoriasis.
The major determinant is PSORS1, which probably accounts for 35–50% of its heritability.
Immunology: In psoriasis, immune cells move from the dermis to the epidermis, where they stimulate skin cells (keratinocytes) to proliferate. Psoriasis does not seem to be a true autoimmune disease. In an autoimmune disease, the immune system confuses an outside antigen with a normal body component, and attacks them both. But in psoriasis, the inflammation does not seem to be caused by outside antigens (although DNA does have an immunostimulatory effect). Researchers have identified many of the immune cells involved in psoriasis, and the chemical signals they send to each other to coordinate inflammation. At the end of this process, immune cells, such as dendritic cells and T cells, move from the dermis to the epidermis, secreting chemical signals, such as tumor necrosis factor-α, interleukin-1β, and interleukin-6, which cause inflammation, and interleukin-22, which causes keratinocytes to proliferate.
DiagnosisA diagnosis of psoriasis is usually based on the appearance of the skin; there are no special blood tests or diagnostic procedures. Sometimes, a skin biopsy, or scraping, may be needed to rule out other disorders and to confirm the diagnosis. Skin from a biopsy will show clubbed rete pegs if positive for psoriasis. Another sign of psoriasis is that when the plaques are scraped, one can see pinpoint bleeding from the skin below ( HYPERLINK "http://en.wikipedia.org/wiki/Auspitz%27s_sign" \o "Auspitz's sign" Auspitz's sign).
Management
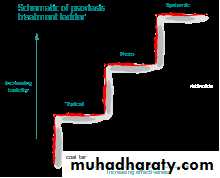
Schematic of psoriasis treatment ladder
There are a number of different treatment options for psoriasis. Typically topical agents are used for mild disease, phototherapy for moderate disease, and systemic agents for severe disease.Topical agents
Bath solutions and moisturizers, mineral oil, and petroleum jelly may help soothe affected skin and reduce the dryness which accompanies the build-up of skin on psoriatic plaques. Medicated creams and ointments applied directly to psoriatic plaques can help reduce inflammation, remove built-up scale, reduce skin turn over, and clear affected skin of plaques. Ointment and creams containing coal tar, dithranol (anthralin), corticosteroids like desoximetasone (Topicort), fluocinonide, vitamin D3 analogues (for example, calcipotriol), and retinoids are routinely used. The use of the Finger tip unit may be helpful in guiding how much topical treatment to use. Activated vitamin D and its analogues can inhibit skin cell proliferation.
Phototherapy
Phototherapy in the form of sunlight has long been used effectively for treatment. Wavelengths of 311–313 nm are most effective and special lamps have been developed for this application. The amount of light used is determined by a persons skin type. Increased rates of cancer from treatment appear to be small.
Psoralen and ultraviolet A phototherapy (PUVA) combines the oral or topical administration of psoralen with exposure to ultraviolet A (UVA) light. The mechanism of action of PUVA is unknown, but probably involves activation of psoralen by UVA light, which inhibits the abnormally rapid production of the cells in psoriatic skin. There are multiple mechanisms of action associated with PUVA, including effects on the skin immune system.
PUVA is associated with nausea, headache, fatigue, burning, and itching. Long-term treatment is associated with squamous cell carcinoma (but not with melanoma).
Systemic agents
Pictures of a patient with psoriasis (and psoriatic arthritis) at baseline and 8 weeks after initiation of infliximab therapy.
Psoriasis that is resistant to topical treatment and phototherapy is treated by medications taken internally by pill or injection (systemic). Patients undergoing systemic treatment are required to have regular blood and liver function tests because of the toxicity of the medication.
Pregnancy must be avoided for the majority of these treatments. Most people experience a recurrence of psoriasis after systemic treatment is discontinued.
The three main traditional systemic treatments are methotrexate, cyclosporine and retinoids. Methotrexate and cyclosporine are immunosuppressant drugs; retinoids are synthetic forms of vitamin A.
Biologics are manufactured proteins that interrupt the immune process involved in psoriasis. Unlike generalised immunosuppressant therapies such as methotrexate, biologics focus on specific aspects of the immune function leading to psoriasis. These drugs (interleukin antagonists) are relatively new, and their long-term impact on immune function is unknown, but they have proven effective in treating psoriasis and psoriatic arthritis. Biologics are usually given by self-injection or in a doctor's office.
Two drugs that target T cells are efalizumab and alefacept. Efalizumab is a monoclonal antibody which blocks the molecules that dendritic cells use to communicate with T cells. It also blocks the adhesion molecules on the endothelial cells that line blood vessels, which attract T cells. However, it suppressed the immune system's ability to control normally harmless viruses, which led to fatal brain infections. Efalizumab was voluntarily withdrawn from the US market in April, 2009 by the manufacturer. Alefacept also blocks the molecules that dendritic cells use to communicate with T cells and even causes natural killer cells to kill T cells as a way of controlling inflammation.
Several monoclonal antibodies (MAbs) target cytokines, the molecules that cells use to send inflammatory signals to each other. TNF-α is one of the main executor inflammatory cytokines. Four MAbs (infliximab, adalimumab, golimumab and certolizumab pegol) and one recombinant TNF-α decoy receptor, etanercept, have been developed against TNF-α to inhibit TNF-α signaling. Additional monoclonal antibodies have been developed against pro-inflammatory cytokines IL-12/IL-23 and Interleukin-17 and inhibit the inflammatory pathway at a different point than the anti-TNF-α antibodies. IL-12 and IL-23 share a common domain, p40, which is the target of the recently FDA-approved ustekinumab.
In 2008, the FDA approved three new treatment options available to psoriasis patients: 1) Taclonex Scalp, a new topical ointment for treating scalp psoriasis; 2) the Xtrac Velocity excimer laser system, which emits a high-intensity beam of ultraviolet light, can treat moderate to severe psoriasis; and 3) the biologic drug adalimumab (brand name Humira) was also approved to treat moderate to severe psoriasis.
Medications with the least potential for adverse reactions are preferentially employed. If the treatment goal is not achieved, then therapies with greater potential toxicity may be used. Medications with significant toxicity are reserved for severe unresponsive psoriasis. This is called the psoriasis treatment ladder. As a first step, medicated ointments or creams, called topical treatments, are applied to the skin. If topical treatment fails to achieve the desired goal, then the next step would be to expose the skin to ultraviolet (UV) radiation. This type of treatment is called phototherapy. The third step involves the use of medications which are taken internally by pill or injection. This approach is called systemic treatment.
The combination therapy for moderate to severe psoriasis using psoralen with ultraviolet A (PUVA) plus acitretin shows a 97.3% PASI improvement from baseline. Therapy limitations need to be taken into consideration in the treatment of moderate to severe psoriasis, such as the increased risk of skin cancer with phototherapy and birth defects with acitretin.
Alternative therapy
Some studies suggest psoriasis symptoms can be relieved by changes in diet and lifestyle. Fasting periods, low energy diets and vegetarian diets have improved psoriasis symptoms , and diets supplemented with fish oil have also shown beneficial effects. Fish oils are rich in the two omega-3 fatty acids eicosapentaenoic acid (EPA) and docosahexaenoic acid (DHA) and contain Vitamin E, furthermore cod liver oil contains Vitamin A and Vitamin D.It has been suggested that cannabis might treat psoriasis, due to the anti-inflammatory properties of its cannabinoids, and the regulatory effects of THC on the immune system.Prognosis:Psoriasis is typically a lifelong condition. There is currently no cure, but various treatments can help to control the symptoms. Many of the most effective agents used to treat severe psoriasis carry an increased risk of significant morbidity including skin cancers, lymphoma and liver disease.
Epidemiology: Psoriasis affects both sexes equally, and can occur at any age, although it most commonly appears for the first time between the ages of 15 and 25 years.The prevalence of psoriasis in Western populations is estimated to be around 2-3%. Around one-third of people with psoriasis report a family history of the disease, and researchers have identified genetic loci associated with the condition. Studies of monozygotic twins suggest a 70% chance of a twin developing psoriasis if the other twin has psoriasis. The concordance is around 20% for dizygotic twins. Onset before age 40 usually indicates a greater genetic susceptibility and a more severe or recurrent course of psoriasis.
Papulosquamous disorders:
Psoriasis, Pityriasis rosea , Lichen planus, Pityriasis rubra pilaris,…Parapsoriasis,…Mycosis fungoides,..Pityriasis lichenoides…DLE…Tinea…Nummular eczema…Seborrhoeic dermatitis..Secondary syphilis …Drug eruptions)Pityriasis rosea The cause un known. An infectious agent has always seemed likely but has not yet been proven: human herpesvirus 7 is the latest suspect.The disorder seems not to be contagious. is common, during winter. It mainly affects children and young adults, and second attacks are rare. Most patients develop one plaque (the ‘herald’ or ‘mother’ plaque) before the others. It is larger (2–5 cm in diameter) than later lesions, and is rounder, redder and more scaly. After several days many smaller plaques appear, on the trunk, neck and extremities. About half of the patients complain of itching. An individual plaque is oval, salmon pink and shows a delicate scaling, adherent peripherally as a collarette. Their longitudinal axes run down and out from the spine, along the lines of the ribs. Purpuric lesions are rare. A minority of patients have systemic symptoms such as aching and tiredness. The eruption lasts between 2 and 10 weeks and then resolves spontaneously, sometimes leaving hyperpigmented patches.DDX: ringworm,guttate psoriasis and secondary syphilis. Gold and captopril are the drugs most likely to cause a pityriasis rosea-like drug reaction,but barbiturates, penicillamine, some antibiotics.
IX: Because secondary syphilis can mimic pityriasis rosea so closely, testing for syphilis is usually wise. Treatment No treatment is curative, active treatment is seldom needed. A moderately potent topical steroid or calamine lotion will help the itching. 1% salicylic acid in soft white paraffin or emulsifying ointment reduces scaling. Sunlight or UVB relieves pruritus and may hasten resolution.
Lichen planus :The cause is unknown, but seems to be mediated immunologically. Lymphocytes abut the epidermal basal cells and damage them. Chronic graft-vs.-host disease can cause an eruption rather like lichen planus in which histoincompatibility causes lymphocytes to attack the epidermis. LP is associated with autoimmune disorders, ( alopecia areata, vitiligo and ulcerative colitis), Drugs can cause LP. Some patients also have a hepatitis B or C infection .Presentation Typical lesions are violaceous or lilac-coloured, intensely itchy, flat-topped papules that usually arise on the extremities, particularly on the volar aspects of the wrists and legs.Variants of lichen planus.(Annular,Atrophic. Bullous, Follicular, Hypertrophic, Ulcerative) a white streaky pattern on the surface of these papules (Wickham’s striae). White asymptomatic lacy lines, dots, and small white plaques, in the mouth, inside the cheeks, (50% of patients) and oral lesions may be the sole manifestation of the disease. The genital skin may be similarly affected . the skin plaques are usually itchy, patients rub rather than scratch, so that excoriations are uncommon. As in psoriasis, the Koِbner phenomenon may occur. 10% of patients show nails ( longitudinal grooves to destruction of the entire nail fold and bed ) Scalp lesions cause a patchy scarring alopecia.Course may last for months and the eruption as a whole last 1 year. the hypertrophic variant with thick warty lesions around ankles lasts for many years. As lesions resolve, they become darker, flatter and leave discrete brown or grey macules.1/6 will have a recurrence.Complications: Nail and hair loss. The ulcerative form in the mouth may lead to SCC. Ulceration,over bony prominences, disabling, especially on the soles. Any association with liver disease is probably caused by the coexisting hepatitis infections.DDX.(papulosquamous diseases.Lichenoid drug reactions ( Gold and other heavy metals, antimalarials,B blockers, NSAID,para-aminobenzoic acid, thiazide diuretics and peni-cillamine. Contact with chemicals used in colour film ,DLE,Oral candidiasis). biopsy will confirm the diagnosis if necessary.Treatment can be difficult. If drugs are suspected as the cause, they should be stopped and unrelated ones substituted. Potent topical steroids .Systemic steroid only in special situations (e.g. unusually extensive involvement, nail destruction or painful and erosive oral LP).photochemotherapy (PUVA) or with narrow-band UVB may reduce pruritus and help to clear up the skin lesions. Acitretin Antihistamines.Mucous membrane lesions:a corticosteroid or tacrolimus in a gel base.
Pityriasis rubra pilaris Several types have been described, but their causes are unknown. A defect in vitamin A metabolism was suggested but disproved. The familial type AD inheritance. The familial type develops gradually in childhood and persists throughout life. The more common acquired type begins in adult life with redness and scaling of the face and scalp. Later, red or pink areas grow quickly and merge, so that patients with PRP are often erythrodermic. Small islands of skin ‘spared’ from this general erythema, but even here the follicles may be red and plugged with keratin. Similarly, the generalized plaques, although otherwise rather like psoriasis, may also show follicular plugging. The palms and soles become thick, smooth and yellow. They often fissure rather than bend. The acquired form of PRP generally lasts for 6–18 months, but may recur. Even when the plaques have gone, the skin may retain a rough scaly texture with persistent small scattered follicular plugs.
DDX: Psoriasis The thickening of the palms and soles, the follicular erythema in islands of uninvolved skin, and follicular plugging within the plaques, especially over the knuckles .Investigations A biopsy may help to distinguish psoriasis from PRP;
Treatment The disorder responds slowly to systemic retinoids such as acitretin (in adults, 25–50 mg/day for 6–8 months; Oral methotrexate in low doses, once a week. Topical steroids and keratolytics (e.g. 2% salicylic acid in soft white paraffin) reduce inflammation and scaling, but usually do not suppress the disorder completely. Systemic steroids are not indicated..
Pityriasis lichenoides uncommon. two forms. The numerous small circular scaly macules and papules of the chronic type are easy to confuse with guttate psoriasis However, their scaling is distinctive in that single silver-grey scales surmount the lesions (mica scales). The acute type is characterized by papules that become necrotic and leave scars like those of chickenpox. More often than not there are a few lesions of the chronic type in the acute variant and vice versa. UVB radiation can reduce the number of lesions and spontaneous resolution occurs eventually.
Erythroderma/exfoliative dermatitis Sometimes the whole skin becomes red and scaly There is a history of a previous skin disease. Sometimesthe histology is helpful but often it is non-specific. Erythroderma’ is the term used when the skin is red with little or no scaling, while the term ‘exfoliative dermatitis’ is preferred if scaling predominates. lymphadenopathy, and many have hepatomegaly. If chronic ectropion, scalp and body hair may be lost, and the nails become thickened and may be shed. Temperature regulationis impaired and heat loss through the skin, patient feel cold and shiver. Oedema, high output cardiac failure, tachycardia, anaemia, failure to sweat and dehydration. Treat the underlying condition.
W i t h b e s t w i s h e s
وستسأل عنها موج البحر وستسأل فيروز الشطأن
وتجوب بحارا وبحارا وتفيض دموعك أنهاراوسيكبر حزنك حتى يصبح أشجارا
وسترجع يوما ياولدي
مهزوما مكسور الوجدان
وستعرف بعد رحيل العمر
بأنك كنت تطارد خيط دخان
فحبيبة قلبك ياولدي
ليس لها أرض أو وطن أو عنوان
ما أصعب أن تهوى أمرأة ياولدي
ليس لها عنوان ... / نزار قباني
اعجبني تعليقات