د.اشرف مزاحم الشاكر كلية طب نينوى
lec: 1
1
General and specific Perioperative Care of the Surgical
Patient
I. PREOPERATIVE EVALUATION AND MANAGEMENT
A. General Evaluation of the Surgical Patient. The goals of preoperative evaluation are to
(1) identify the patient's medical problems and functional status;
(2) determine if further information is needed to characterize the patient's medical status;
(3) estimate the patient's level of risk for the planned procedure;
(4) establish if the patient's condition is medically optimized.
Much of this can be accomplished with a thorough history and physical examination. For
minor surgical procedures and procedures on young, healthy patients, routine diagnostic
testing is often unnecessary. For patients with existing comorbidities, or in patients
undergoing certain complex procedures, preoperative laboratory studies and imaging should
be decided on an individual basis.
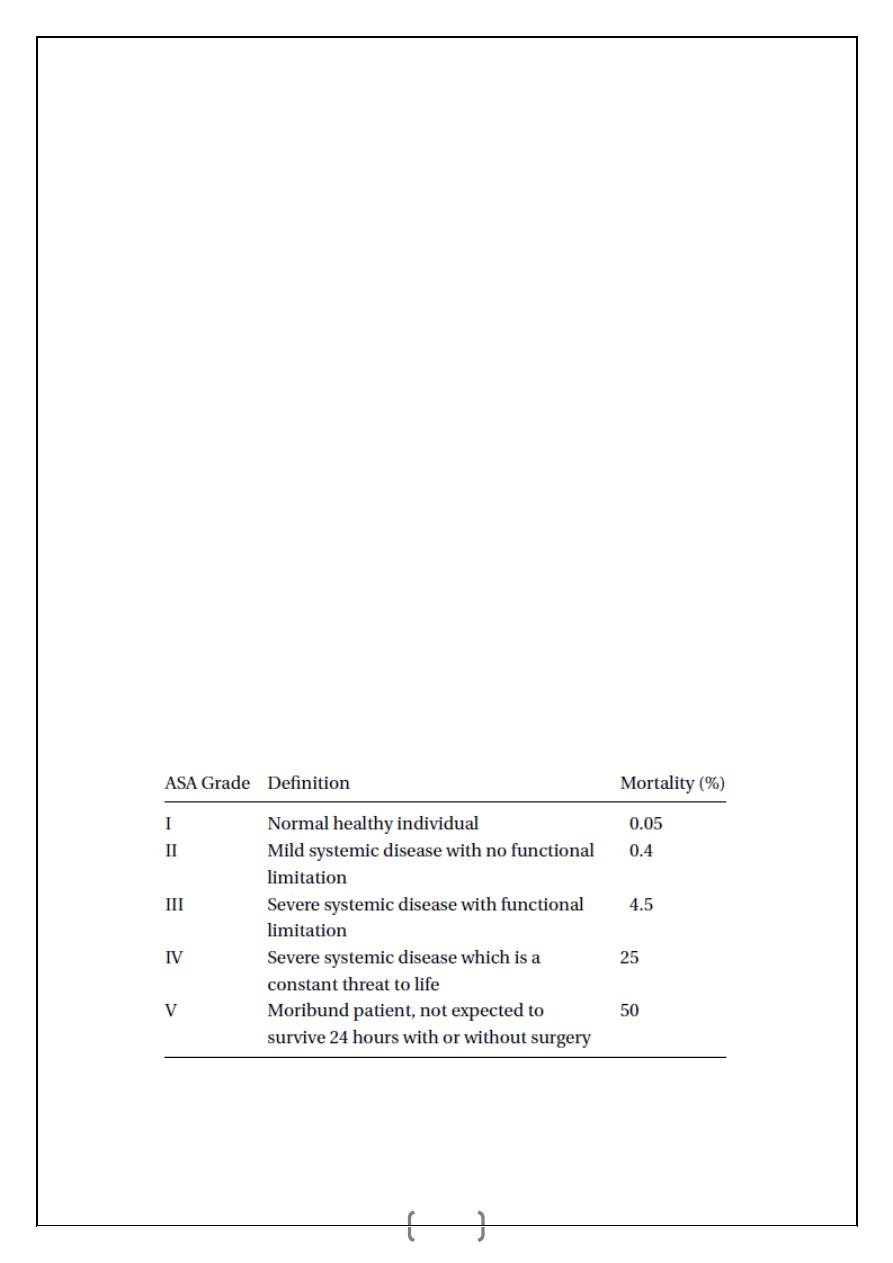
What is the ASA grading system?
The American Society of Anesthesiologists (ASA) grade is the most commonly used grading
system, which accurately predicts morbidity and mortality associated with anaesthesia and
surgery.
د.اشرف مزاحم الشاكر كلية طب نينوى
lec: 1
2
What are the most common reasons for cancellation of an operation on the day of
surgery?
_ Onset of new medical condition
_ Insufficient optimisation of co-existing conditions
_ Inadequate investigations of co-existing conditions
_ Lack of critical care beds (less common than above three factors)
B. Specific Considerations in Preoperative Management:
1. Cardiovascular disease
is one of the leading causes of death after noncardiac surgery.
Patients who experience a myocardial infarction (MI) after noncardiac surgery have a
hospital mortality rate of 15% to 25% (CMAJ. 2005;173:627).
a. Risk factors.
Patient factors: have been identified and are associated with perioperative cardiac
morbidity and mortality. These include age above 70 years, unstable angina, recent
(prior 6 months) MI, untreated CHF, diabetes mellitus, valvular heart disease, cardiac
arrhythmias, peripheral vascular disease, and functional impairment.
Factors related to the surgical procedure: Intrathoracic, intraperitoneal, major
vascular, emergency surgery, uncontrolled intraoperative bleeding.
e. Preoperative management:
(1) Patients with pacemakers should have their pacemakers turned to the uninhibited mode
before surgery. In addition, bipolar cautery should be used when possible in these patients. If
unipolar cautery is necessary, the dispersive electrode should be placed away from the heart.
(2) Patients with internal defibrillators should have these devices turned off during
surgery.
(3) Perioperative beta-blockade: recent studies, including the PeriOperative ISchemic
Evaluation (POISE) trial, suggest that beta-blockers reduce perioperative ischemia and may
reduce the risk of MI and cardiovascular death in high-risk patients (Lancet. 2008;371:1839-
1847). Beta-blockers should ideally be started days to weeks before elective surgery.
Preoperatively, each patient's dose should be titrated to achieve adequate heart rate control to
benefit from betablockade while avoiding the risks of hypotension and bradycardia
(Circulation. 2009;120:2123- 2151).
د.اشرف مزاحم الشاكر كلية طب نينوى
lec: 1
3
(4) Patients with recent angioplasty or stenting: Several studies have shown a high
incidence of cardiovascular complications when noncardiac surgery is performed shortly
after coronary angioplasty or stenting. Current guidelines are to delay noncardiac surgery at
least 6 weeks after coronary angioplasty or placement of bare metal stents, which require 6
weeks of dual antiplatelet therapy with aspirin and clopidogrel. In contrast, dual antiplatelet
therapy should be continued for at least 12 months following placement of a drug-eluting
stent (DES), which can affect timing of elective operations.
2. Pulmonary disease.
Preexisting lung disease confers a dramatically increased risk of
perioperative pulmonary complications. Risk factors for pulmonary complications include
chronic obstructive pulmonary disease, smoking, asthma, obstructive sleep apnea, advanced
age, obesity, surgical site located near the diaphragm, and functional status.
a. Preoperative evaluation and screening
(1) Physical examination should be performed carefully, with attention paid to signs of lung
disease (e.g., wheezing, prolonged expiratory/inspiratory ratio, clubbing, or use of accessory
muscles of respiration).
(2) Diagnostic evaluation
(a) A chest x-ray (CXR) should only be performed for acute symptoms related to
pulmonary disease, unless it is indicated for the specific procedure under consideration.
(b) An arterial blood gas (ABG) can be considered in patients with a history of lung disease
or smoking to provide a baseline for comparison with postoperative studies, but is not
reliable to accurately predict postoperative pulmonary complications.
(c) Preoperative pulmonary function testing is controversial and probably unnecessary in
stable patients with previously characterized pulmonary disease undergoing nonthoracic
procedures.
b. Preoperative prophylaxis and management
(1) Pulmonary toilet. Increasing lung volume by the use of preoperative incentive
spirometry is potentially effective in reducing pulmonary complications.
(2) Antibiotics do not reduce pulmonary infectious complications in the absence of
preoperative infection. Elective operations should be postponed in patients with respiratory
infections. If emergent surgery is required, patients with acute pulmonary infections should
receive intravenous (IV) antibiotic therapy.
د.اشرف مزاحم الشاكر كلية طب نينوى
lec: 1
4
(3) Cessation of smoking. All patients should be encouraged to and assisted in smoking
cessation before surgery.
(4) Bronchodilators. In the patient with obstructive airway disease and evidence of a
significant reactive component, bronchodilators may be required in the perioperative period.
Elective operation should be postponed in the patient who is actively wheezing.
3. Renal disease
a. Preoperative evaluation of patients with existing renal insufficiency:
Risk factors: Patients without preexisting CRI ranges may be at risk of developing
postoperative acute renal failure (ARF), elevated preoperative BUN or creatinine,
CHF, advanced age, intraoperative hypotension, sepsis, aortic cross-clamping,
intravascular volume contraction, and use of nephrotoxic and radionucleotide agents.
(1) Evaluation
(a) History. Patients with hypertension or diabetes and CRI are at a substantially increased
risk of perioperative morbidity and mortality. The timing and quality of the patient's last
dialysis session, the amount of fluid removed, and the preoperative weight provide important
information about the patient's volume status. In nonanuric patients, the amount of urine
made on a daily basis should also be documented.
(b) Physical examination should be performed to assess the volume status. Elevated jugular
venous pulsations or crackles on lung examination can indicate intravascular volume
overload.
(c) Diagnostic testing
(i) Laboratory data. Serum electrolyte and bicarbonate levels should be measured, as well
as blood urea nitrogen (BUN) and creatinine. A complete blood cell count (CBC) should be
obtained to evaluate for significant anemia or a low platelet level. Normal platelet numbers
can mask platelet dysfunction in patients with chronic uremia.
(2) Management
(a) Timing of dialysis. Dialysis should be performed within 24 hours of the planned
operative procedure.
(b) Intravascular volume status. Cardiac events are the most common cause of death in
patients with CRI. Both hypovolemia and volume overload are poorly tolerated, and invasive
monitoring in the intraoperative and postoperative periods may assist in optimizing fluid
balance.
د.اشرف مزاحم الشاكر كلية طب نينوى
lec: 1
5
(3) Prevention
(a) Intravascular volume expansion. Adequate hydration is the most important preventive
measure for reducing the incidence of ARF.
(b) Radiocontrast dye administration. Patients undergoing radiocontrast dye studies have
an increased incidence of postoperative renal failure. Fluid administration (1 to 2 L of
isotonic saline) alone appears to confer protection against ARF.
(c) Other nephrotoxinsÑincluding aminoglycoside antibiotics, nonsteroidal anti-
inflammatory drugs (NSAIDs), and various anesthetic drugs can predispose to renal failure,
as well, and should be avoided in patients at high risk for postoperative renal failure.
4. Infectious complications
: Infectious complications are a major cause of morbidity and
mortality following surgery. They may arise at the surgical site itself or in other organ
systems.
a. Assessment of risk: Risk factors for infectious complications after surgery can be
grouped into procedure-specific and patient-specific risk factors.
(1) Procedure-specific risk factors include the type of operation, the degree of wound
contamination (whether the case is classified as clean, clean/contaminated, contaminated, or
dirty), and the duration and urgency of the operation.
(2) Patient-specific risk factors include age, diabetes, obesity, immunosuppression,
malnutrition, preexisting infection, and other chronic illness.
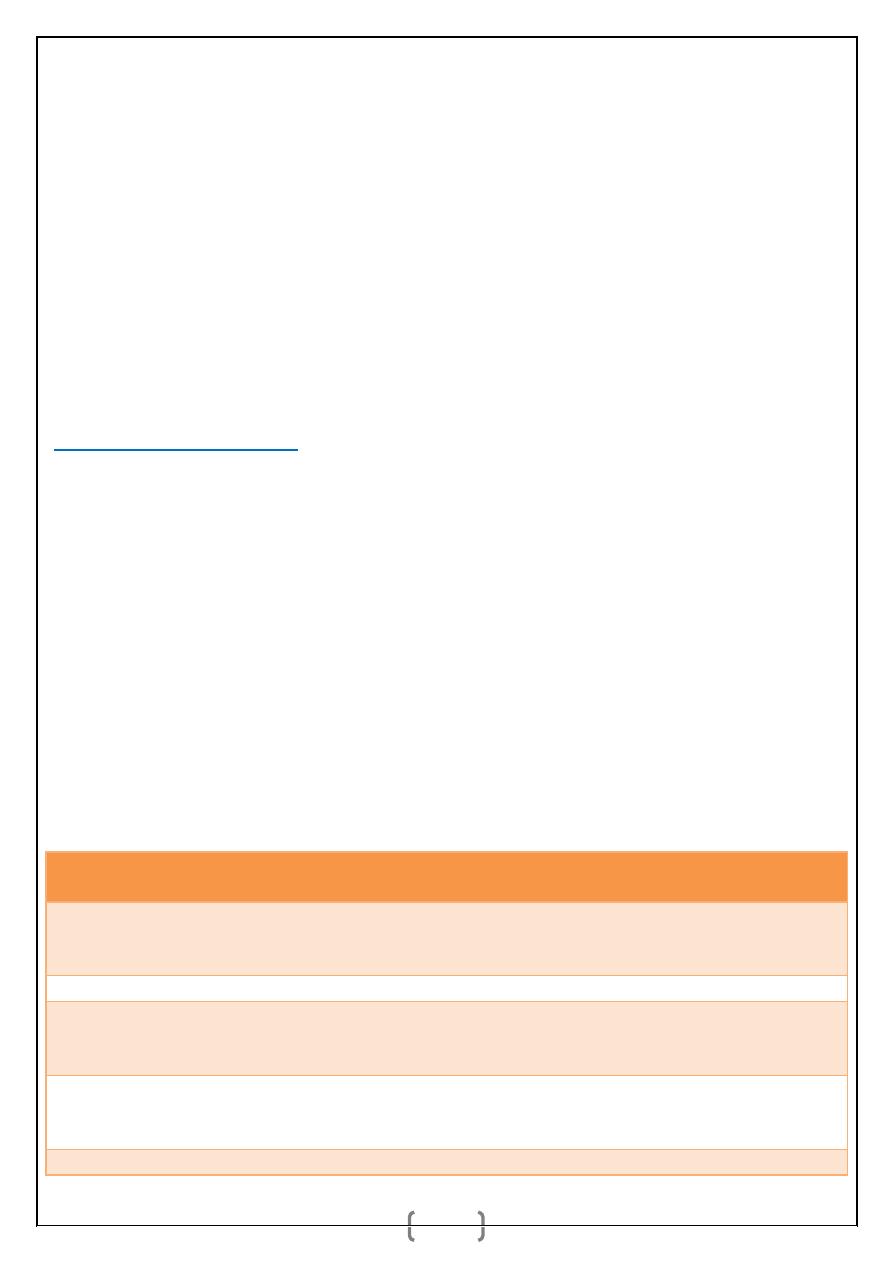
b. Prophylaxis:
(1) Surgical site infection:
Operation
Likely Pathogens
Recommended
Antibiotics prophylaxis
Cardiac: Prosthetic valve
and other procedures
Staphylococci,
corynebacteria, enteric
Gramnegative bacilli
Vancomycin and Cefazolin
Vancomycin and Aztreonam
Thoracic
Staphylococci
Cefazolin Vancomycin
Vascular: Peripheral
bypass or aortic surgery
with prosthetic graft
Staphylococci,streptococci,
Enteric Gram-negative
bacilli, clostridia
Cefazolin
Vancomycin and
Aztreonama
Orthopedic: Total joint
replacement or internal
fixation of fractures
Staphylococci
Cefazolin
Vancomycin
Upper GI and
Enteric Gramnegative bacilli,
Cefazolin Cefotetan
د.اشرف مزاحم الشاكر كلية طب نينوى
lec: 1
6
hepatobiliary
enterococci, clostridia
Cefoxitin
Colorectal
Enteric Gramnegative bacilli,
anaerobes, enterococci
Cefoxitin Cefotetan
Ertapenem Cefazolin
and Metronidazole
Appendectomy (no
perforation)
Enteric Gramnegative bacilli,
anaerobes, enterococci
Cefoxitin
Cefotetan
Obstetrics/gynecology
Enteric Gramnegative bacilli,
anaerobes, group B
streptococci, enterococci
Cefotetan Cefoxitin
Cefazolin Clindamycin and
Gentamicin
(2) Respiratory infections. Risk factors and measures for preventing pulmonary
complications are discussed above.
(3) Genitourinary infections may be caused by instrumentation of the urinary tract or
placement of an indwelling urinary catheter. Preventive measures include avoiding
catheterization for short operations, sterile insertion of the catheter, and removal of the
catheter on postoperative day 1. Some operations that include a low pelvic dissection, will
require longer catheterization because of local trauma.
