Small IntestineLec. 9dr.Rajaa Ahmad
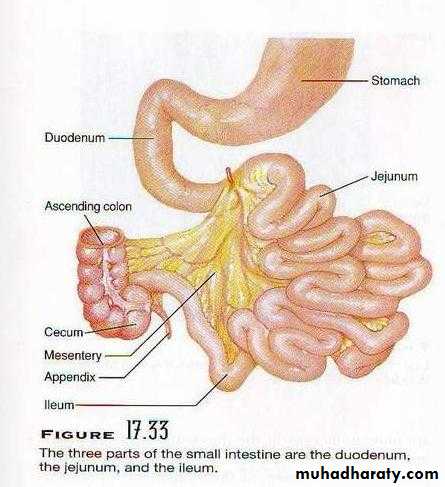
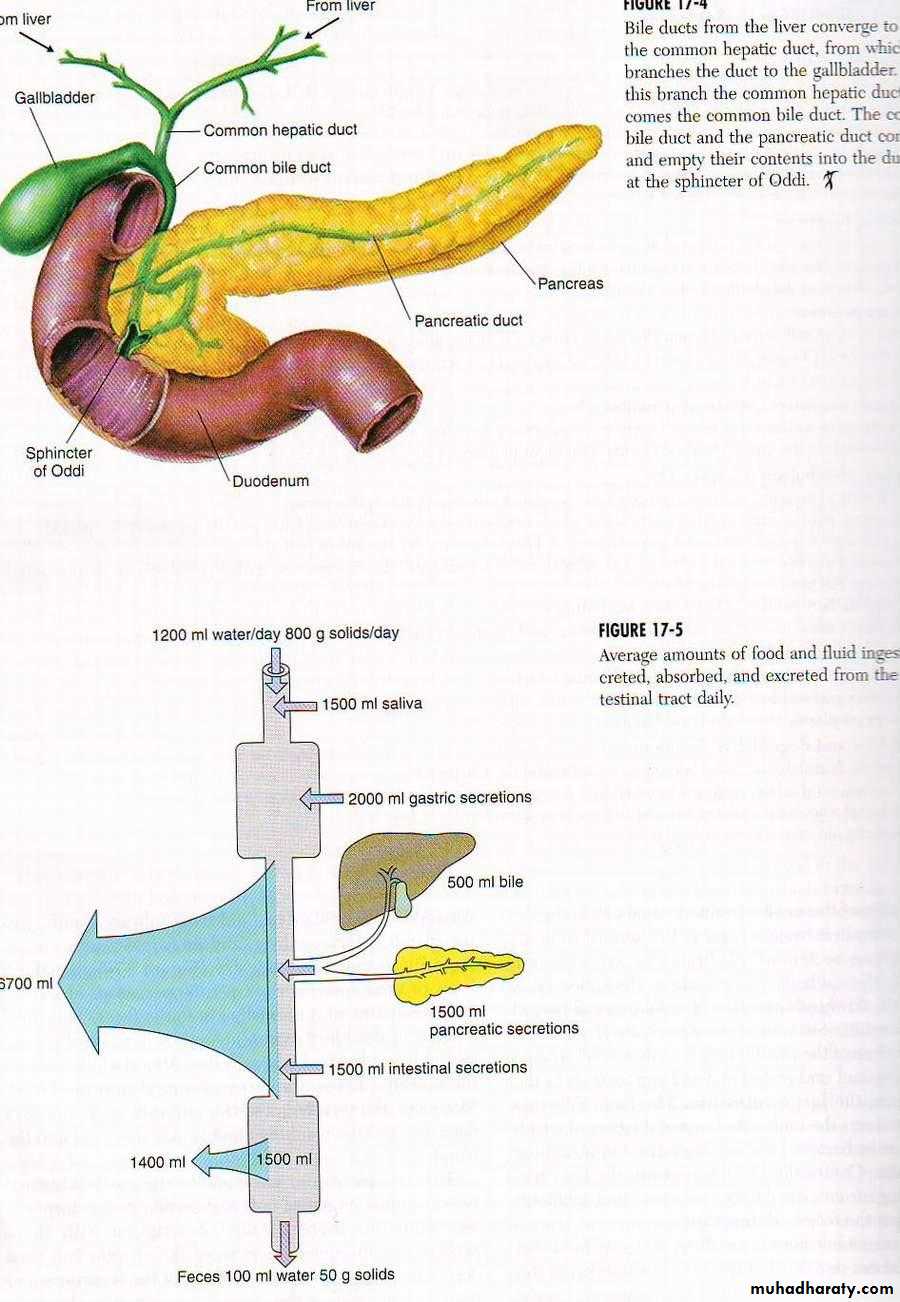
• Small intestine is divided into duodenum, jejunum and ileum.The intestinal contents are mixed with mucosal secretion, pancreatic juice and bile. Digestion which begins in the mouth is completed in the small intestine.9 liters of fluid enter the small intestine/day 2L. from dietary sources; 7L. (endogenous secretions). Seven L. are absorbed by the small intestine and 1.5-2L. are passed to the colon, 1.4-1.8mls are absorbed and only 100-200ml passed out.
• Secretions of the small intestine
• 1. Brunner’s Glands: compound mucous glands they are located mainly between the pylorus and the papilla of vater. These glands secrete alkaline mucus in response to the followings:• 1) Tactile or Irritating stimuli of the mucosa.
• 2) Vagal stimulation.
• 3) GIT hormones, especially secretin.
• The function of the alkaline mucus secretion by Brunner’s glands is to protect the duodenal wall from digestion by the acidic gastric juice.
• Their bicarbonate is added to the pancreatic bicarbonate and liver HCO3 for neutralization of HCl.
Brunner’s glands secretion is inhibited by sympathetic stimulation such stimulation leave the duodenal bulb unprotected; and is one of the factors that cause this area of GIT to be the site of peptic ulcers in about 50% of the cases.
• 2.Crypts of Lieberkühn:
• On the entire surface of the small intestine are small pits called crypts of Lieberkühn. They lie between the intestinal villi. The surface of the crypts and villi are covered by an epithelium composed of:• 1)Goblet cells: secrete mucus that lubricates and protects the intestinal surfaces.
• 2) Enterocytes: secrete large quantities of H2O and electrolytes into the crypts; and over the surfaces. The villi, reabsorb the H2O and electrolytes with the end product of digestion.
The intestinal secretions are formed by the enterocytes of the crypts which is normally=1800ml/day it is almost extracellular fluid its PH=7.5-8.0. They are rapidly reabsorbed by the villi.
This circulation of fluid from the crypts to the villi supplies a watery vehicle for absorption of substances from the chyme as it comes with contract with the villi, which is a primary function of the small intestine.
The exact mechanism of the marked secretion of watery fluid by the crypts is not known. It may be due to two active secretory process:
1) Active secretion of Cl- into the crypt.
2) Active secretion of HCO3- into the crypt.
3) Both of them cause electrical drag of Na+ ions through the membrane, all three processes cause osmotic movements of water.
• Enzymes in the small intestine secretion
• The enterocytes of the mucosa especially those that cover the villi do contain digestive enzymes these enzymes are:• 1) Peptidases: split small peptides into a.a.
• 2) Four enzymes split disaccharides into monosaccharide (sucrase, maltase, isomaltase and lactase).
• 3) Small amount of intestinal Lipase, split nuetral fats into glycerol and fatty acids.
• These enzymes are mainly seen in the brush border of the enterocytes cause hydrolysis of food.
• The epithelial cells deep in the crypts continually undergo mitosis and the new cells migrate gradually along the basement membrane upward out of crypts towards the Tip of the villi, thus continually replacing aged villi, they are finally shed into the intestinal secretions.
• Seventeen billions of intestinal epithelial cells are replaced each day and the entire epithelium of the small intestine is replaced every 5 days. This allows rapid repair of excoriations of mucosa.
• Movement of the small intestine:
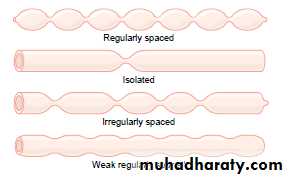
• 1) Mixing contraction (segmentation contraction).
• Distention with chyme lead to stretch the intestinal wall.
• Localized concentric contractions spread at interval along the intestine. The length of each one= 1cm ,each set of contractions causes segmentation of the small intestine which have the appearance of a chain of sausages. As one set of segmentation relaxes, a new set begins. Contraction this time occur mainly at new points between the previous contractions.so chop the chyme with intestinal secretion
• The segmentation contraction becomes exceedingly weak when the excitatory activity of the enteric nervous system is blocked by (Atropine).
• 2) Propulsive movements: (peristalsis) Occur in any part of the small intestine they move anal ward at a velocity of 0.5-2.0 cm/sec. it is much faster at proximal intestine and much slower in the terminal intestine. They die out after 3-5cm.it is very weak so3-5 hr. are required for passage of chyme from pylorus to ileocecal valve.
• Peristaltic activity of the small intestine increase after a meal .
• This is because• 1) Distention by chyme and stimulation of enteric nervous system.
• 2) gastrointestinal reflex.
• Hormonal factors which enhance intestinal motilities and secretion are:
• 1) Gastrin 2) CCK 3) Insulin 4) Serotonin
• Inhibitor for small intestinal motility are:
• 1) Secretin 2) glucagon
Control of Peristalsis by Nervous and Hormonal Signals
Perstaltic activity of the small intestine increase after a meal ,this is because:
1) Distention by chyme and stimulation of enteric nervous system
2) gastroenteric reflex.
Hormonal factors which enhance intestinal motilities and secretion are:
1) Gastrin 2) CCK 3) Insulin 4) Serotonin
Inhibitor for small intestinal motility are:
1) Secretin 2) glucagon
• Function of the peristaltic waves in the small intestine is:
• 1) Progression of the chyme toward the ileocecal valve.• 2) Spread out the chyme along the intestinal mucosa.
• On reaching the ileocecal valve, the chyme evacuation is sometime blocked for several hours until a person eat another meal, when a new gastroenteric reflex intensify peristaltic waves and forces the remaining chyme evacuated through ileocecal valve into the cecum.
• Peristaltic rush:
• Peristalsis in the small intestine is very weak normally. Intense irritation of the intestinal mucosa as occurs in some sever cases of infectious diarrhea, cause powerful and rapid peristalsis called peristaltic rush.
• Peristaltic rush is initiated by the following reflexes:
• Extrinsic nervous reflexes to the autonomic nervous system ganglia and the brain stem and then back again to the gut.• Direct enhancement of the myentric plexus reflexes.
• * The powerful peristaltic contractions then travels long distances in the small intestine within minutes.
• Sweeping the contents of the intestine into the colon and relieving the small intestine of either irritative chyme or excessive distention.
• Movement caused by the muscularis mucosae and muscle fiber of the villi:
• Musularis mucosae can cause short or long folds to appear in the intestinal mucosa.
• It cause the folds to move to newer areas of mucosa.
• Their individuals fibers extend from the muscle into the intestinal villi and cause them to contract intermittently.
• The mucosal folds increase the surface area exposed to the chyme and increase the rate of absorption.
• Contraction of the villi (shortening and elongating and shortening again (milking) allow lymph flow freely from the cental lacteals into the lymphatic system. both mucosal and villious contractions are initiated by local nervous reflexes in the submucosal plexus in response to distention of the small intestine by chyme exposed to absorption.
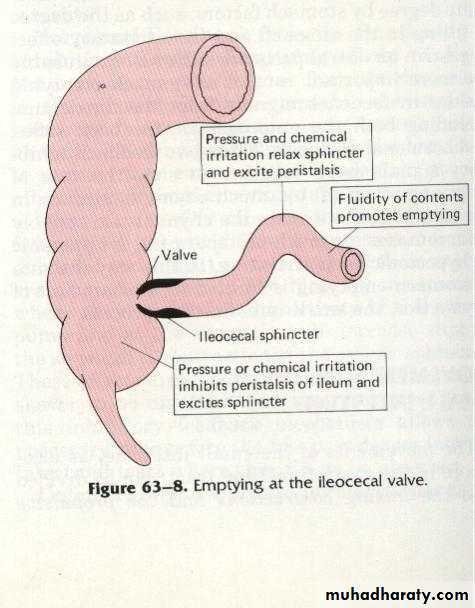
Function of the ileocecal valve:
A principle functions is to prevent backflow of fecal content from the colon into the small intestine.Lips of the ileocecal valve protrude into the lumen of the cecum and are forcefully closed when excess pressure builds up in the cecum and tries to push the cecal contents backwards against the lips.
The valve resist reverse pressure of 50-60cm H2O.
The wall of the ileum few cms preceding the valve has a thickened musculature called ileocecal sphincter.
The sphincter remain normally mildly constricted and slow the emptying of ileal contents into the cecum except immediately after a meal. When gastroileal reflex intensifies the peristalsis in the ileum.
• The resistance to emptying at the ileoecal valve prolong the stay of chyme in the ileum and their by increase absorption.
• Normally (1500)ml. of chyme empty into the cecum daily.
• There are some factors that promote emptying of the ileum those factors are:
• Intense peristalsis in the distal ileum.
• Fluidity of the content promaote emptying.
• Pressure and chemicals, irritation, relax the ileocecal sphincter and excite peristalsis.
• Gastrin secretion increase emptying by increasing peristaltic waves.
• 5) Gastroileal reflexes immediately after a meal increases peristalsis and promote emptying.
• Factors that inhibit emptying of the ileum:
• When cecum is distended, the contraction of the ileocecal sphincter is intensified this inhibit ileal peristalsis and emptying.
• Irritant substances, chemicals in the cecum delays or inhibit emptying ex. inflamed appendix cause intense spasm of the ileocecal sphincter and paralysis of the ileum which block ileal emptying.
•
1)Intense peristalsis in distal ileum
4)Gastrin secretion increase emptying by increasing perstalsis.3
2
2) Distention of the cecum increase contraction of I.C.S. cause inhibition of ileal perstalsis and emptying.
3) Inflammation of the appendix cause spasm of the ileocecal sphincter cause paralysis of the ileum block emptying (prevertebral sympathetic ganglia.