ENDOCRINE SYSTEM
DR.AMJAD H. ABID LECTURE (7)HORMONES OF THE GONADS
The gonads are bifunctional organs that produce germ cells and the sex hormones. The ovaries produce ova and the steroid hormones [estrogen and progesterone] while the testes produce spermatozoa and [testosterone]. The productions of these hormones are tightly regulated through a feed- back loop that involves the pituitary and hypothalamus. Three kinds of highly specialized cells carry out these functions:-Spermatogonia: highly differentiated germ cells that are located in the seminiferous tubules.
-The leyding cells: (also called interstitial cells) which are scattered in the connective tissue between the coiled seminiferous tubules and produce testosterone in response to leutinizing hormone (LH) from the pituitary gland.
-The Sertoli cells: which form the basement membrane of the seminiferous tubules and provide the environment necessary for germ cell differentiation and maturation, through the production of the androgen binding protein (ABP) under the effect of follicular stimulating hormone (FSH).
This ABP has a very high affinity for Testosterone (TT) and so TT will enter to inside leading to a very high intracellular concentration of TT (*100 times). This very high concentration will ensure differentiation and maturation of sperms.
BIOSYNTHESIS OF TESTESTERONE:
Testicular androgens are synthesized in the interstitial tissue by the Leyding cells. The immediate precursor of the gonadal steroids- as for the adrenal steroids- is the cholesterol which is delivered to the inner membrane of the mitochondria by a transport protein known as steroidogenic acute regulatory protein (STARP).Once in the proper location, the side chain cleavage enzyme P450SCC acts upon it. The conversion of cholesterol to pregnenolone is identical in adrenal glands, ovaries, and testes, except that in the later, the reaction is promoted by LH rather than by ACTH. This occurs in the mitochondria and following the formation of pregnenolone; it will leave the mitochondria to the endoplasmic reticulum where all the subsequent steps will occur over there.
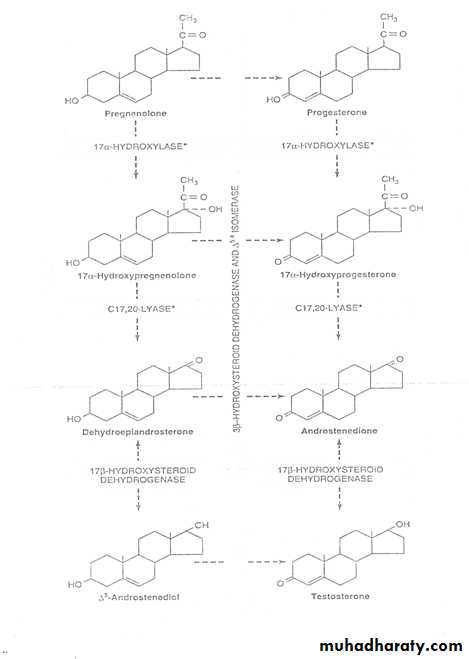
The conversion of pregnenolone to testosterone requires the action of five active enzyme activities; these are: *3β-hydroxysteroid dehydrogenase (3βOHSD) and D5,4isomerase.*17α-hydroxylase and C17, 20 lyase.*17β-hydroxysteroid dehydrogenase (17bOHSD).This sequence is referred to as the progesterone (or D4) which is on the right side of the following figure.
Pregnenolone can also be converted to testosterone by the dehydroepiandrosterone (or D5pathway) which is on left side of the figure. The route [D5pathway] appears to be the preferred pathway in human testes. Therefore the formation follows 2- pathways: -The upper pathway (D5pathway).-The lower pathway (D4pathway).The TT can be converted into another hormone in the testes as in peripheral target tissue or even in the liver and therefore TT is considered to be a hormone and a pre-hormone as well. The reduction of ring A at position 5 through the action of the enzyme (5-α-reductase) leads to the production of 5a-dihydroxytestosterone. Two types of (5α reductase) are present; Type I which is present in the liver and Type II which is present in the peripheral target tissue.
During the day about 5mg of TT is synthesized and on the other hand the testes produce about 0.1mg of DHT, however about 0.3-0.4 mg of DHT is being produced in the extra-testicular tissues making the day production of DHT up to about 1\10 of the daily production of TT (0.5mg\day for DHT to 5mg\day for TT).
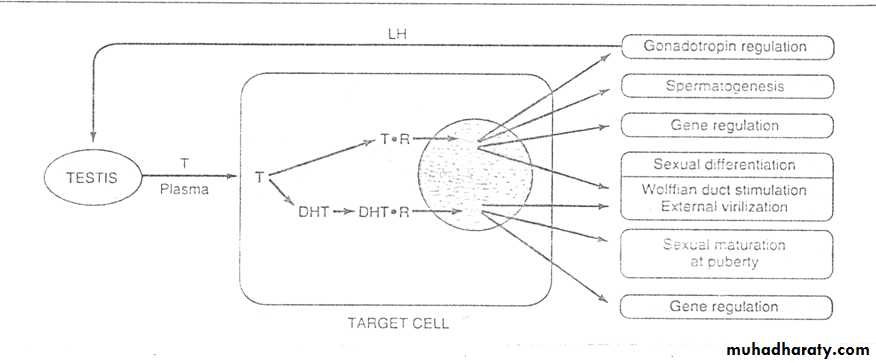
Target tissues in the body which are sensitive to TT include spermatogonia, muscle, liver and brain as well as kidney. On the other hand there are certain organs which are sensitive to DHT such as: prostate, seminal vesicle, external genitalia and genital skin.
The testes as well as extra-testicular tissues can also participate in the production of small amount of estrogen specially estradiol (E2) through aromatization of ring A. This small amount of E2 plays a vital role in the feed back control of spermatogenesis through feed- back inhibition on FSH together with inhibin, DHT, TT but the inhibin is the most potent inhibitor. E2 has also an additional effect on modifying the functions of the testes.
PLASMA TRANSPORT OF TESTESTERONE
TT binds to a kind of β-globulin that binds TT with specificity, relatively high affinity and limited capacity. This is called sex hormone binding globulin (SHBG) or testosterone-estrogen binding globulin (TEBG) which is produced in the liver. Its production is increased by:* estrogen (women have twice the serum conc. Of SHBG as men), *certain types of liver diseases, and *hyperthyroidism.However, it is decreased by androgens, advancing age, and by hypothyroidism. TT binds to SHBG and albumin at the rate of 97-99% and so only 1%-3% presents in free (active) form. The primary function of SHBG may be to attenuate the free concentration of TT in the serum, so any change in the level of SHBG causes a greater change in the free TT level than in free estradiol because it has less affinity to bind with SHBG. An increase in SHBG leads to increase free E2: TT ratio.
METABOLIC FUNCTION OF TT:
1-Sexual differentiation.
2-Spermatogenesis.3-Development of secondary sexual features.4-Developments of anabolic effects on somatic growth of tissues including bone, muscles and cartilage.5-General anabolic effect (promoting synthesis effects).
Male FemaleTotal TT 11-33nmol\l 0.5-2.5nmol\lSHBG 58% 97% Albumin-bound 40% 2% Free 2% 1%
Metabolism of TT:
TT is metabolized by 2 pathways:-1st. Involves oxidation at the 17-position.- 2nd. Involves reduction of the A ring double bond and the 3-ketone.Metabolism by the1st pathway occurs in many tissues including liver and produces 17-ketosteroids that are generally inactive or less active than the parent compound. However, the metabolism via the 2nd pathway which is less efficient occurs primarily in the target tissues and produces the potent metabolite DHT.
TESTOSTERONE a-5reductase DHT
NADPH
The most important metabolic product of TT metabolism is the DHT since in many tissues including prostate, external genitalia, and some areas of the skin; it’s the active form of hormone. Plasma content in adult male is 1\10 of TT and about 400mg of DHT is produced daily while TT 5mg.
Two form of 5a-reductase are present (type II and I). Type I is predominantly expressed in the liver, while type II is predominant in reproductive tissues and peripheral targets. Mutations of type II enzyme producing gene are associated with male pseudohermaphroditism.
The major 17-ketosteroid metabolites, androsterone and etiocholanolone are conjugated with glucoronide and sulfate in the liver to make them water soluble and excretable compounds.
REGULATION of "TT" PRODUCTIONLH stimulates steroidogenesis and testosterone production by binding to the receptors on the plasma membrane of leyding cells (an analogous LH receptor is found in the ovary on cells of corpus luteum) and activating adenylate cyclase, thus increasing intracellular cAMP. This action enhances the rate of cholesterol transport and side chain cleavage by P450SCC. TT provides feedback control at the hypothalamus through inhibition of GnRH release, GnRH production or both.