ENDOCRINE SYSTEM
DR.AMJAD H. ABID LECTURE (8)THE FEMALE SEX HORMONES
The gonads produce germ cells and sex hormones, these 2 functions are necessarily approximated in both genders (spermatogenesis and testosterone production in the testes and oogenesis and estradiol production in the ovaries).BIOSYNTHESIS AND METABOLISM OF OVARIAN HORMONES:
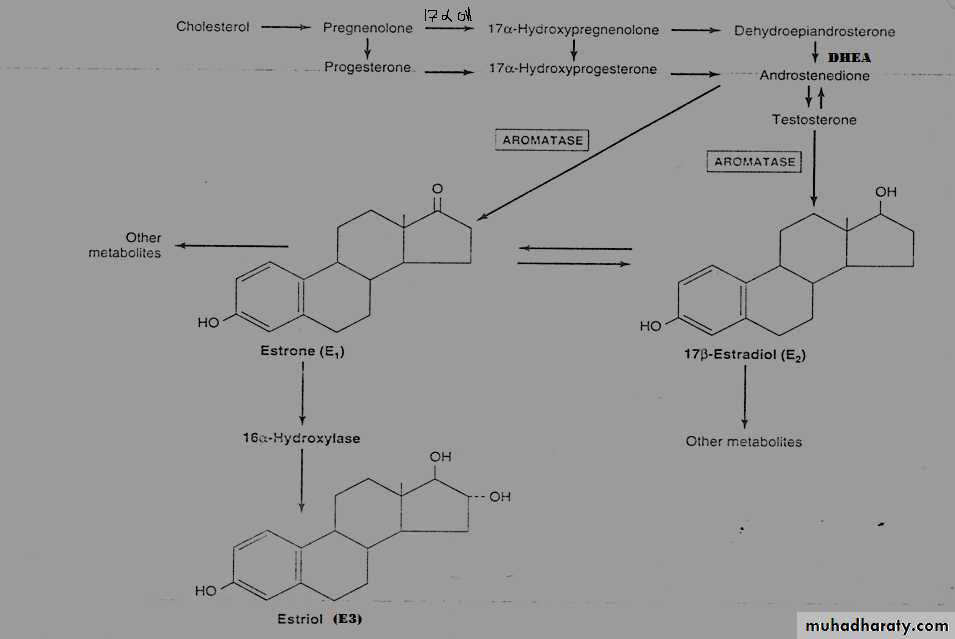
The estrogens are a family of hormones synthesized in a variety of tissues, 17 –β Estradiol is the primary estrogen of ovarian origin. Estrogens are formed by the aromatization of androgens in a complex process that involves 3 hydroxylation steps each of which requires O2 and NADPH. The aromatase enzyme is thought to include a P450 mixed- function oxidase.Estradiol is formed if the substrate of this enzyme complex is TT, whereas esterone results from the aromatization of androstenedione.
Theca cells are the source of androstendione and TT, these are converted by the aromatase enzyme in the granuloza cells to esterone and estradiol respectively.
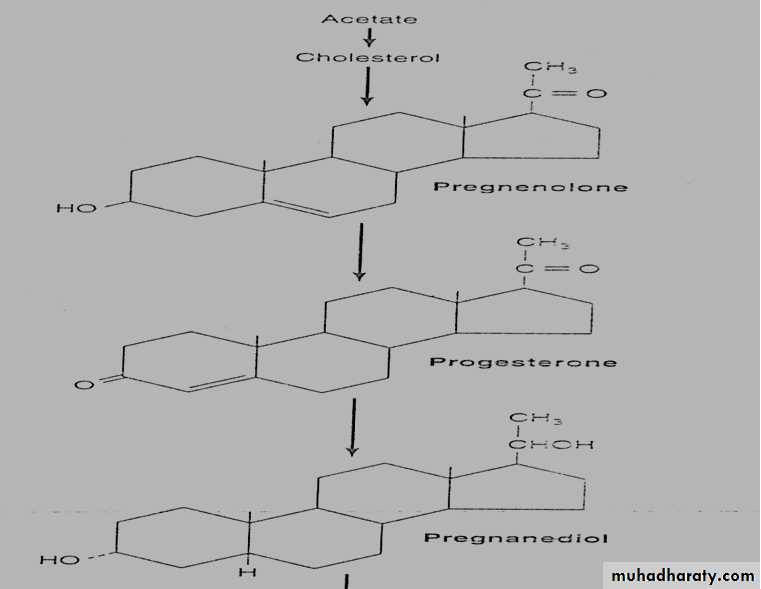
Progesterone is produced and secreted by the corpus luteum, which also makes some estradiol.
Significant amounts of estrogens are produced by the peripheral aromatization of androgens in human male.
The peripheral aromatization of TT to E2 accounts for 80% of the production of E2. In females; adrenal androgens are important substrates, since as much as 50% of the E2 produced in pregnancy comes from aromatization of androgenes.
The conversion of androstenedione to esterone is the major source of estrogens in postmenopausal female. Aromatase activity is present in adipose cells and also in liver, skin, and other tissues. The increased activity of this enzyme may contribute to the “estrogenization” that characterizes such disease as cirrhosis of liver, hyperthyroidism, aging, and obesity.
ESTROGENS AND PROGESTINS BINDING TO PLASMA PROTEINS
Estrogens are bound to SHBG and progestins to CBG. The (SHBG) binds estradiol about five times less avidly than it binds TT or DHT, while progesterone and cortisol have little affinity for this protein. In contrast, progestines and cortisol bind with nearly equal affinity to CBG, which in turn has little avidity for estradiol and even less for TT, DHT, or esterone.The metabolic clearance rates of these steroids are inversely related to the affinity of their binding to SHBG, hence esterone is cleared more rapidly than estradiol, which in turn is cleared more rapidly than TT or DHT. The rate of secretion of ovarian steroids varies considerably during the menstrual cycle and is directly related to rate of production in the ovary. There is no storage of these compounds and, in fact, they are secreted when they are produced.
METABOLISM OF ESTROGENS AND PROGESTERONE
A. Estrogens : the liver converts estradiol and esterone to estriol so the E2,E1,E3 are substrates for hepatic enzymes that add glucuronide or sulfate moieties then the conjugated steroids are water soluble and don’t bind to transport proteins, so excreted in bile ,feces and urine. B. Progestins: they are also metabolized by liver to several compounds and excreted in the urine as "sodium-pregnanediol 20- glucuronide". So it is ineffective when given orally, other derivatives of 17-alpha hydroxy- progesterone and 17alpha -alkyl-substituted 19-nortestosterone compounds have progestins activity and avoid hepatic metabolism so can be used as contraceptive drugs.BIOSYNTHESIS OF PROGESTERONE
HORMONAL REGULATION OF THE MENESTRUAL CYCLE
The human menestrual cycle results from complex interactions between hypothalamus, pituitary and ovaries. The cycle normally varies between 25- 35 days in duration. It is divided into follicular phase, leuteal phase and menestrual phase.
Follicular phase:
A particular follicle begins to enlarge under the general influence of FSH. Estradiol levels here are very low during the first week, but they start to increase progressively as the follicle enlarge to reach the maximal level 24 hr before the LH peaks and sensitizes the pituitary to the actions of GnRH.
LH is released either in response to this high level of estradiol in a positive feedback manner or in response to a sudden decline of estradiol from this high level. The continuous administration of estrogen by OCCP suppresses the LH and FSH release and inhibits the action on the pituitary gland. Progesteron levels are very low in this phase, the LH peaks at the end of the follic. Phase and precedes ovulation by 16- 18 hrs.
B. Leuteal phase:
After ovulation, the granuloza cells of the ruptured follicle luteinize and form the corpus luteum; a structure that soon begins to produce progesterone and some estradiol. Estradiol peaks about mid-way through the luteal phase and then declines to a very low level.The major hormone of the luteal phase of the menstrual cycle is the progesterone which is required for the preparation and maintenance of the secretory endometrium that provides early nourishment for the implanted blastocyst. LH is required for the early maintenance of the corpus luteum and the pituitary gland supplies it for about 10 days.
Maintenance of Pregnancy by Placental Hormonal Activity:
Human placenta is an endocrine organ that aids in keeping the pregnancy going on. It releases the following hormones:1. HCG: can be detected within few days from the commencement of the pregnancy and measuring HCG represents the basis for the "pregnancy test".
2. Progestine: synthesized in the first 6-8 weeks of the pregnancy.
3. Estrogens: The "estriol" is synthesized in the highest amounts among other estrogens reflecting a number of its crucial fetoplacental functions.
4. Placental lactogen: also called as "chorionic somatomamotropin" or "placental growth hormone". It has some biological properties of prolactin and growth hormone (GH) of the pituitary. However, the exact function of PL is uncertain, since women who lack this hormone appear to have normal gestation and deliver normal babies.