Fatal Growth Restriction
By
Dr Tahani Ali
This lecture contain headlines to simplify the subject
For more information and details you can return to the text books .NOTE
Determinants of birth weight are multifactorial, and reflect the influence of the natural growth potential of the fetus dictated largely by the fetal genome and by the intrauterine environment.
Which is influenced by both maternal and placental factors.
SO The ultimate birthweight is the result of the interaction between
( fetal genome+ the maternal uterine environment)
Determinants of fetal birthweight
Fetal growth is dependent on adequate transfer of nutrients and oxygen across the placenta. This in itself is dependent on appropriate maternal nutrition and placental perfusion.
Factors are important in determining fetal growth and include, for example, fetal hormones. They affect the metabolic rate, growth of tissues and maturation of individual organs.
In particular, insulin-like growth factors (IGFs) coordinate a precise and orderly increase in growth throughout late gestation. Insulin and thyroxine (T4) are required through late gestation to ensure appropriate growth in normal and adverse nutritional circumstances.
Fetal hyperinsulinaemia, which occurs in association with maternal diabetes mellitus when maternal glycaemiccontrol is suboptimal, results in fetal macrosomia with, in particular, excessive fat deposition.
It is failure of a fetus to reach its full growth potential .
SGA means that the weight of the fetus is less than the tenth centile for its gestationIt is associated with a significant increased risk of perinatal morbidity and mortality.
Definition And Risks
not all small for gestational age (SGA) fetuses are growth restricted; some of these babies are constitutionally small and have reached their full growth potential.
however
, not all growth-restricted fetuses are SGA in that while their birthweight is within the normal range for gestation BUT they have failed to reach their full growth potential.
SO
One of the challenges in obstetric practice is to identify potentially growth-restricted fetuses and then, from this group, those that are ‘small and healthy’ and those that are ‘small and unhealthy’.
In addition
Growth-restricted fetuses are more likely to suffer intrauterine hypoxia/asphyxia and, as a consequence, be stillborn.
are more prone to neonatal hypothermia, hypoglycaemia, infection and necrotizing enterocolitis. or demonstrate signs and symptoms of hypoxic-ischaemic encephalopathy (HIE), including seizures and multiorgan damage or failure in the neonatal period.
low birthweight infants are more likely to develop hypertension, cardiovascular disease (ischaemic heart disease and stroke) and diabetes in adult life, indicating the impact that FGR is long lasting.
RISKS
They are grouped into two main categories:
factors that directly affect the intrinsic growth potential of the fetus_ genetic syndromes
_ fetal infections.
External influences that affect fetal growth
maternal systemic factors .
placental insufficiency.
Maternal under-nutrition is globally the major cause of FGR.
Low maternal oxygen saturation
Smoking, alcohol and cocaine
poor placental function
Multiple pregnancy
Aetiology
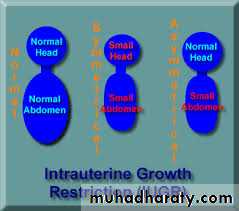
FGR is frequently classified as
Symmetrically small fetuses are associated with factors that directly impair fetal growth, such as chromosomal disorders and fetal infections.Asymmetrical growth restriction is classically associated with which leads to reduced oxygen transfer to the fetus and impaired excretion of carbon dioxide by the placenta. A fall in PO2 and a rise in pCO2 in the fetal blood induces a chemoreceptor response in the fetal carotid bodies with resulting vasodilatation in the fetal brain, myocardium and adrenal glands, and vasoconstriction in the kidneys, splanchnic vessels, limbs and subcutaneous tissues. The liver circulation is also severely reduced
Pathophysiology
In brief, the detection of an SGA infant contains two elements:
first, the accurate assessment of gestational age andsecond, the recognition of fetal smallness.
Early measurement of the fetal crown–rump length before 13 weeks plus 6 days gestation or head circumference between 16 and 20 weeks remains the method of choice for confirming gestational age.
Thereafter, the most precise way of assessing fetal growth is by ultrasound biometry (biparietal diameter, head circumference, abdominal circumference and femur length)
Management
When a diagnosis of SGA has been made, the next step is to
# clarify whether the baby is normal and simply constitutionally small or whether it is FGR.ultrasound examination of the fetal anatomy should be made looking for fetal abnormalities that may explain the size.
the presence of symmetrical growth restriction in the presence of a normal amniotic fluid volume raises the suspicion of a fetal genetic defect and the parents should be counselled accordingly.
Amniocentesis and rapid fetal karyotype should be offered.
# Features suspicious of uteroplacental insufficiency are an asymmetrically growth restricted fetus with a relatively small abdominal circumference, oligohydramnios and a high umbilical artery resistance.
treatments available for FGR related to uteroplacental insufficiency.
Obvious contributing factors, such as smoking, alcohol and drug abuse, should be stopped and the health of the women should be optimized.
Low-dose aspirin may have a role in the prevention of FGR in high-risk pregnancies but is not effective in the treatment of established cases.
When growth restriction is severe and the fetus is too immature to be delivered safely, bed rest in hospital is usually advised in an effort to maximize placental blood flow although the evidence supporting this practice is limited. The aim of these interventions is to gain as much maturity as possible before delivering the fetus, thereby reducing the morbidity associated with prematurity. However, timing the delivery in such a way that maximizes gestation without risking the baby dying in utero demands intensive fetal surveillance.
treatment
The prognosis of FGR is highly dependent upon the
cause,severity
the gestation at delivery.
When FGR is related to a congenital infection chromosomal abnormality, subsequent development of the child will be determined by the precise abnormality.
babies with FGR secondary to uteroplacenta insufficiency, some babies will suffer morbidity or mortality as a result of prematurity.
For the survivors, the long-term prognosis is good with low incidences of mental and physical disability and most infants demonstrate ‘catch-up growth’ after delivery when feeding is established.
A link between FGR and the adult onset of hypertension and diabetes has been established. It remains to be seen whether other associations will be found in the future.
Prognosis