Dr.Fakhir Yousif


osteoporosis
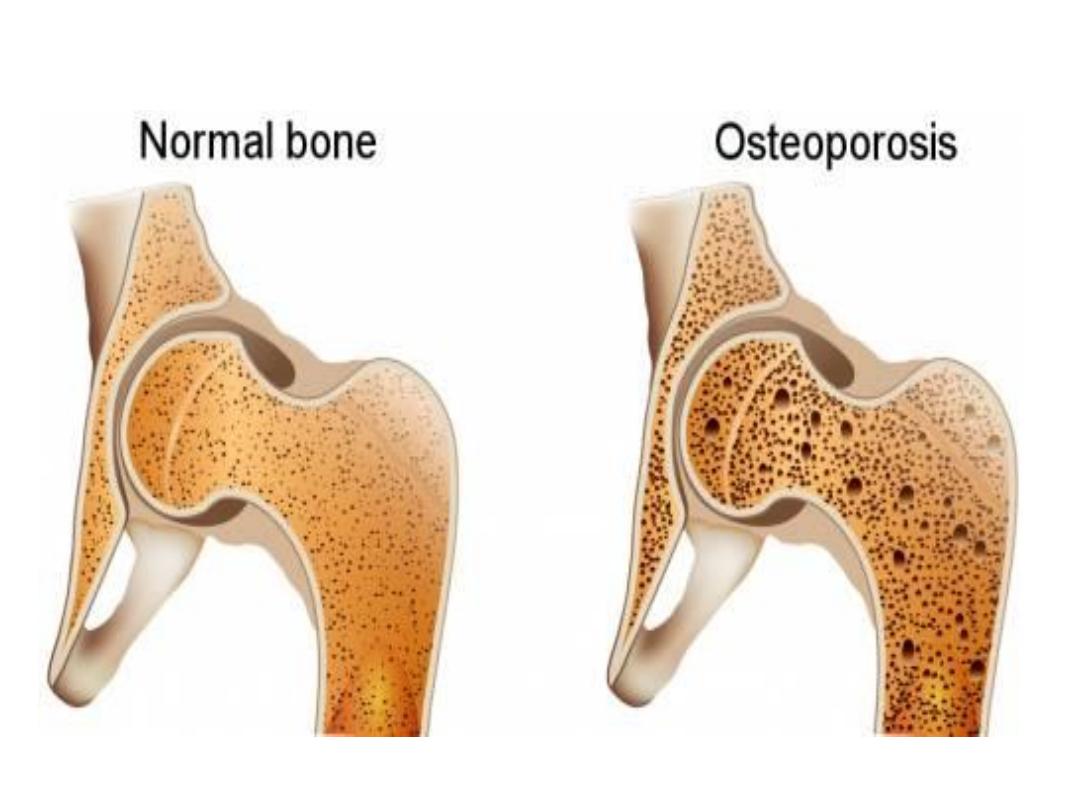
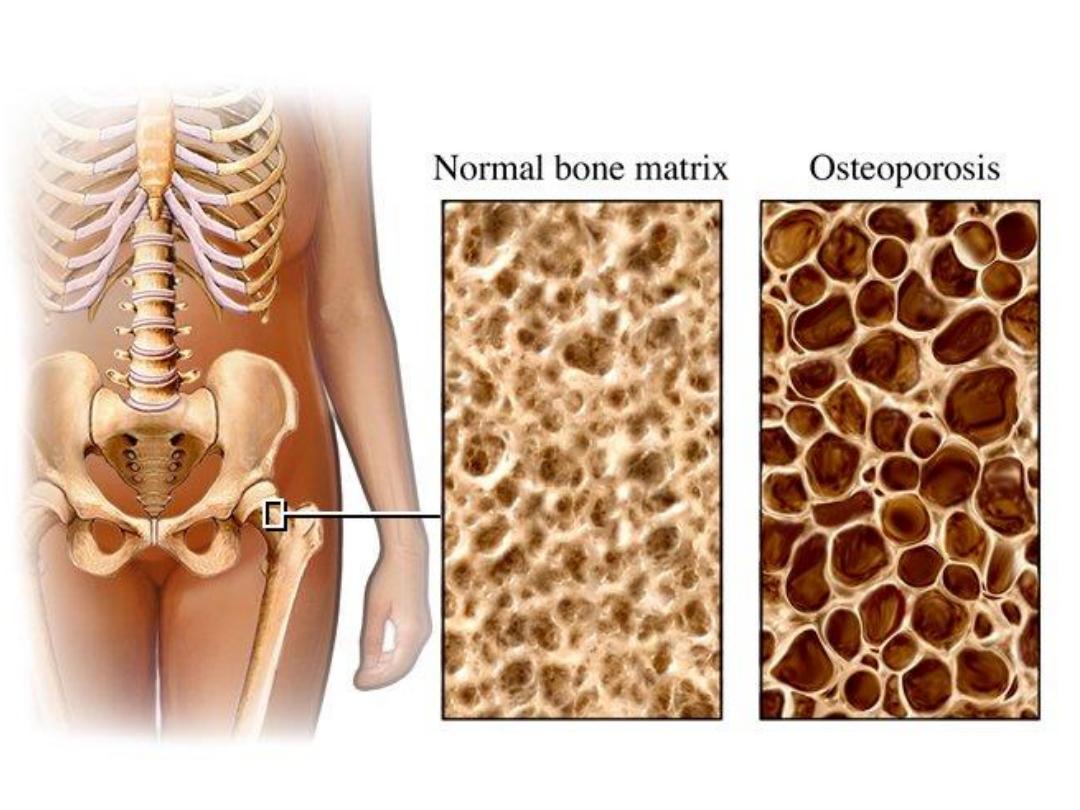
The most common bone disease
Characterized by
:
•
reduced bone density
•
micro-architectural deterioration of bone
tissue
•
increased risk of fractures
The risk of osteoporosis increases markedly
with age

Pathogenesis of
osteoporosis
• In normal individuals, bone mass increases
during skeletal growth to reach its peak at 20
– 40 years of age, and starts to fall thereafter.
• Bone remodeling (formation and resorption)
is responsible for renewal and repair of
skeleton in adult life.
• Osteoporosis can occur because of a defect
in attaining peak bone mass and/or because
of accelerated bone loss (bone resorption
exceeding bone formation).

Bone remodeling
o
It starts with attraction of osteoclast precursors
from the peripheral blood to the target sites.
o
Osteoclast precursors express RANK (receptor
activator of nuclear factor κB). Osteocytes contain
RANK ligand (RANKL) that activates the RANK
on osteoclast precursors to differentiate into
mature osteoclasts.
o
Bone formation follows with attraction of
osteoblast precursors to the resorption site
.

Pathogenesis of
osteoporosis
• Postmenopausal osteoporosis
• Age related (senile) osteoporosis
• Osteoporosis in men
• Secondary osteoporosis
• Corticosteroid-induced osteoporosis

Postmenopausal
osteoporosis
There is an accelerated phase of bone loss after
menopause.
Postmenopausal bone loss is caused by oestrogen
deficiency, which naturally stimulates bone
formation
Postmenopausal osteoporosis is caused by a
combination of low peak bone mass and
exaggerated postmenopausal bone loss.

Postmenopausal
osteoporosis
Individual differences in the development of
postmenopausal osteoporosis are due to certain
additional factors:
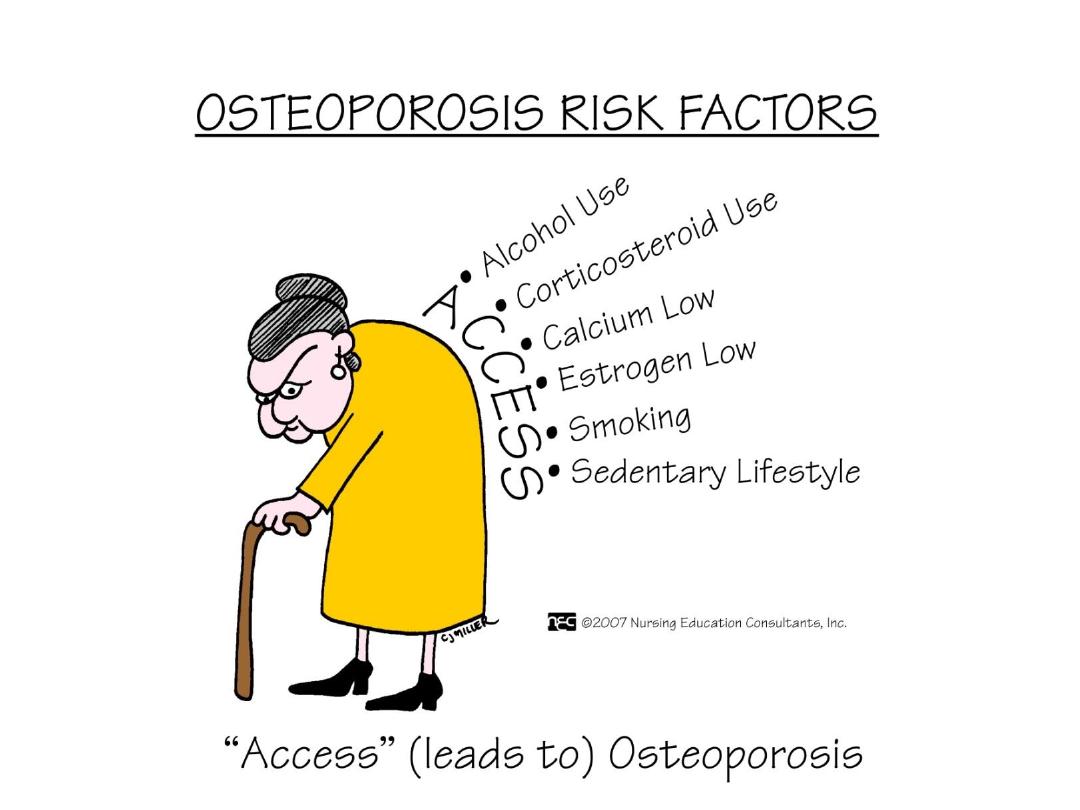
• Genetic factors
: account for 80% of the population
variance of the risk of osteoporosis
• Environmental factors:
– exercise and calcium intake during growth
– smoking increases the risk of postmenopausal
osteoporosis
– alcoholism is a recognized cause of osteoporosis

age related osteoporosis
• Gradual bone loss occurs with advancing
age in both genders.
• Bone resorption is not particularly increased,
but bone formation is reduced.
• The genetic and environmental factors are
also responsible for the individual variation
in age related osteoporosis

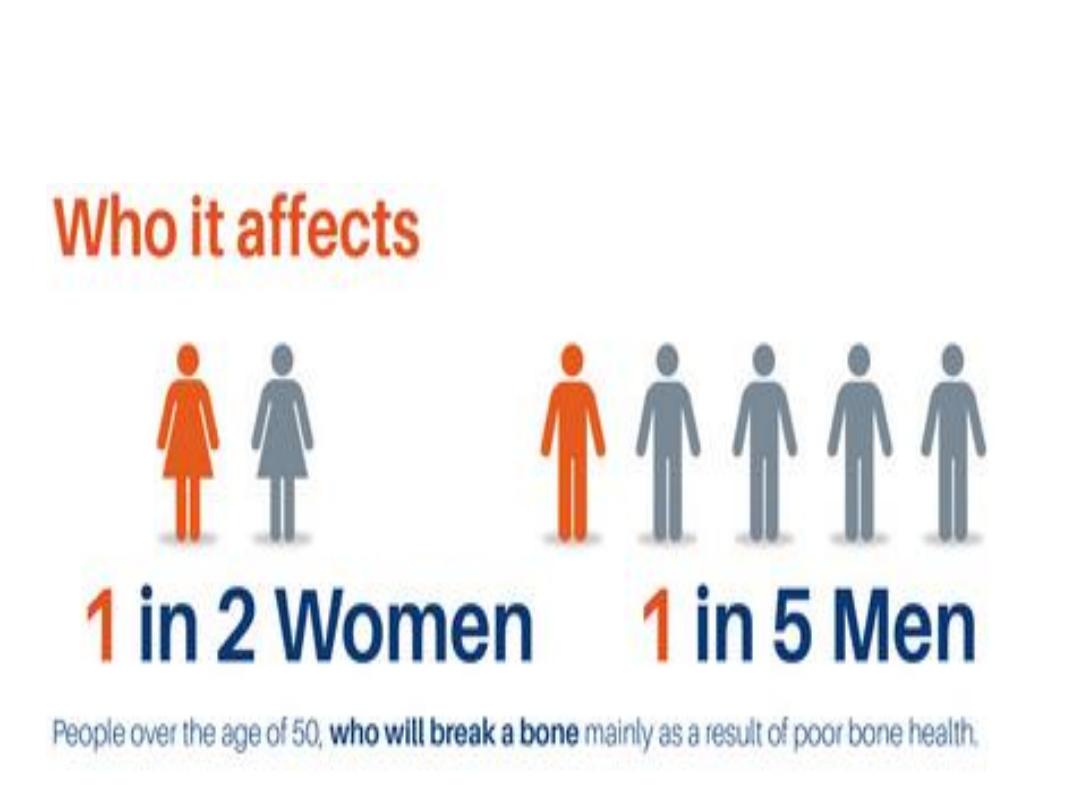
Osteoporosis in men
• Osteoporosis is less common in men than in
women.
• A secondary cause is identified in 50% of cases,
most importantly hypogonadism, corticosteroid
treatment and alcoholism.
• The mechanism of hypogonadism-induced
osteoporosis is similar to postmenopausal
osteoporosis
• In the remaining 50% of men, genetic susceptibility
is probably responsible.

Secondary osteoporosis
Osteoporosis occurring as a complication of diseases
or drug treatment
• Endocrine diseases:
hypogonadism,
hyperparathyroidism, thyrotoxicosis, Cushing's
syndrome
• Inflammatory diseases:
rheumatoid arthritis,
inflammatory bowel disease
• Drugs:
corticosteroid, thyroid hormones,
anticonvulsants and heparin
• GIT diseases:
malabsorption, chronic liver disease
• Miscellaneous:
anorexia nervosa, multiple
myeloma, immobilization

Corticosteroid induced
osteoporosis
• Corticosteroid therapy is an important cause of
osteoporosis.
• Corticosteroids also directly inhibit osteoblast
activity and stimulate their apoptosis.
• The risk is directly related to the dose and duration
of treatment.
• Osteoporosis is less likely with inhaled
corticosteroids and when corticosteroid dose is less
than 5 mg prednisolone per day.
• The risk is substantial when the dose exceeds 7.5
mg for more than 3 months.

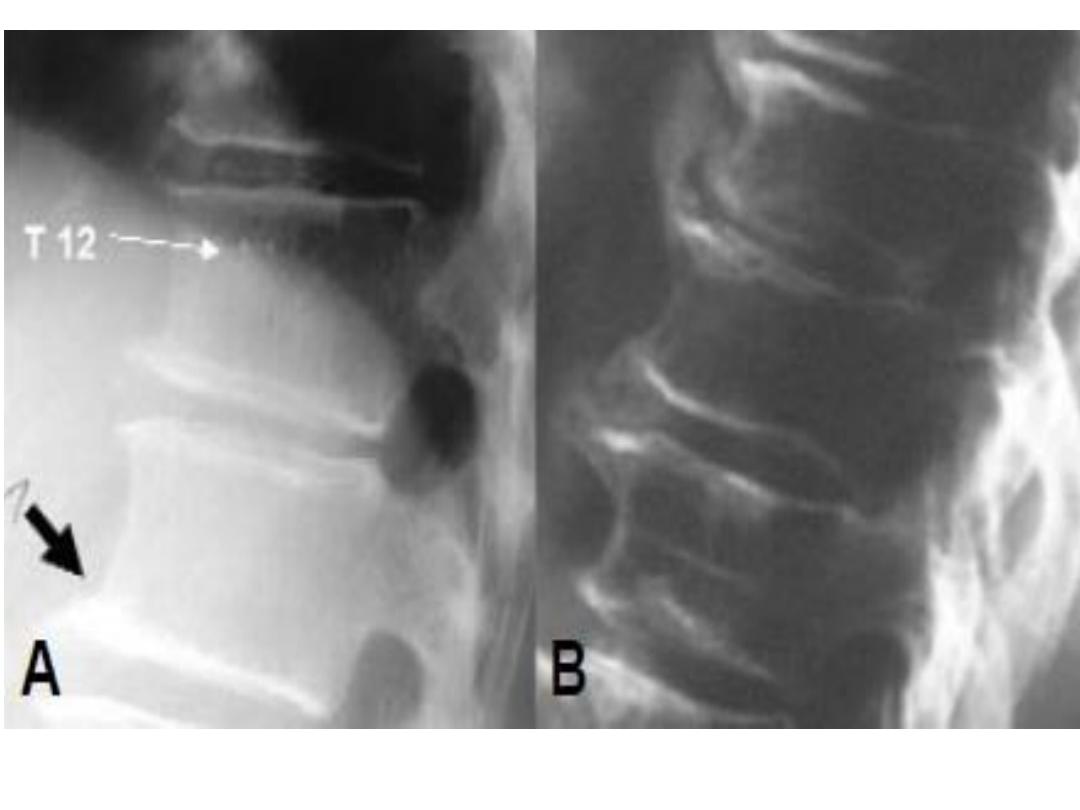
Clinical features of
osteoporosis
• Asymptomatic until fracture occurs
• Fractures due to bone fragility are the most
common manifestation.
• Back pain, height loss, kyphosis and discovery of
radiological osteopenia during evaluation for other
conditions are also important.
• Osteoporotic fractures can affect any bone but the
most common sites are the forearm (Colles
fracture), spine (vertebral fractures) and femur (hip
fracture).

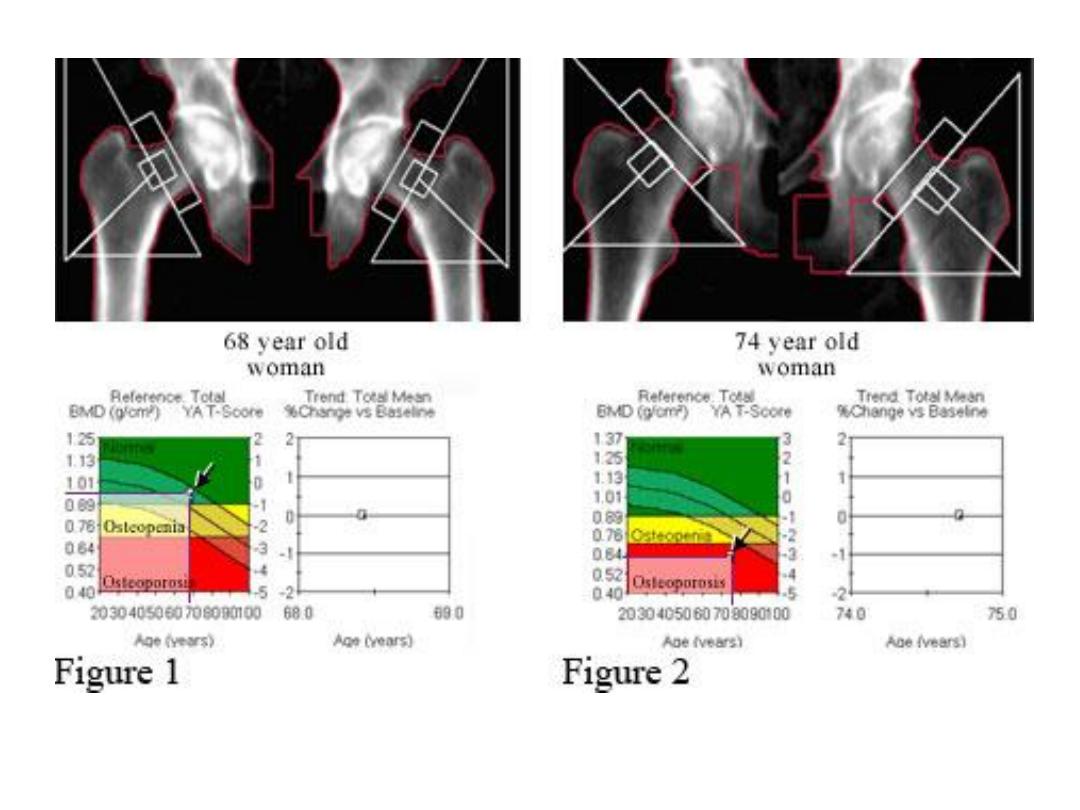
Investigations
• Diagnosis of osteoporosis requires the
measurement of bone mineral density (BMD).
• The preferred technique is
dual energy X ray
absorptiometry (DEXA)
of the hip and spine
• The machine gives the result of T-score and Z-
score.
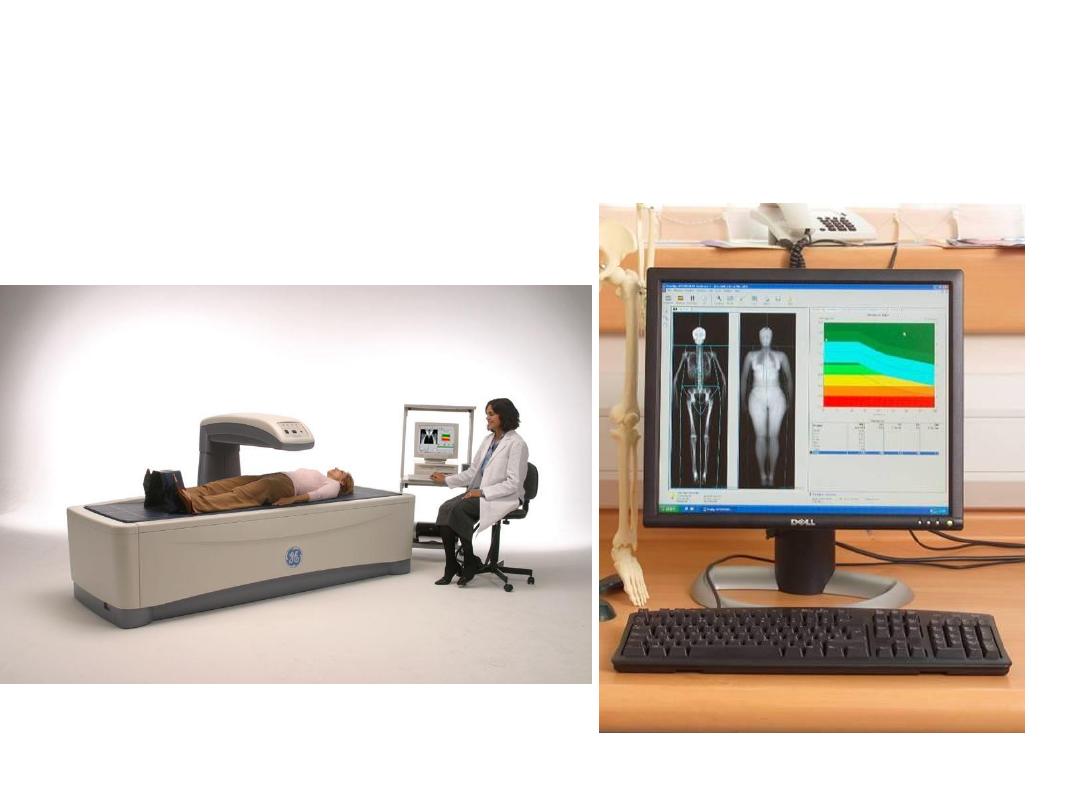
Dual energy X ray
absorptiometry (DEXA)
Dual energy X ray
absorptiometry
• T-score
measures how many standard deviations
(SD) the patient BMD differs from that of a
healthy control
• Z-score
measures how many SD the BMD of the
patients differ from that of an aged matched
control.
T-score: - 2.5 or below indicates osteoporosis
between – 1.0 to – 2.5 is considered osteopenia.
Values above - 1.0 are considered normal

Indications BMD measurement include:
• low trauma fractures
• height loss and kyphosis
• osteopenia on X ray
• corticosteroid therapy
• family history of osteoporosis fracture
• BMI< 18
• menopause <45
• diseases causing osteoporosis
• high FRAX score

Osteoporosis : cause
identification
• History
should be taken to identify causes as early
menopause, smoking, alcohol intake and steroid
therapy.
• Clinical examination
should search for endocrine
disorders, multiple myeloma or inflammatory
diseases.
• Routine investigations
• Sex hormones and gonadotropines
should be
assessed in men with osteoporosis and in women
with amenorrhoea before 50.

Management of osteoporosis
Patients with osteopenia are advised on life style
modification including:
• smoking and alcohol cessation
• increasing dietary calcium
• encouragement of exercise
Indications for drug therapy
1. T-score below -2.5
2. Corticosteroid induced osteoporosis with T-score
below -1.5
3. Vertebral fractures irrespective to BMD

Bisphosphanates
• The most commonly prescribed drugs for
osteoporosis.
• Synthetic pyrophosphate analogues that adsorb on
bone surface and inhibit osteoclast function.
• Increase in BMD of 5 – 8 % after 2 years of
therapy.
• Alendronate (70 mg/week) and risedronte
(35mg/week) are the most commonly prescribed
oral bisphosphanates. Zolendronic acid (5mg IV
annually) is also effective
• These drugs prevents postmenopausal bone loss
and reduces the risk of vertebral and non-vertebral
fractures. Bisphosphanates are also effective in the
prevention and treatment of corticosteroid induced
and male osteoporosis.

Bisphosphanates
• Oral bisphosphanates are poorly absorbed from
the GIT and should be taken on empty stomach,
with plain water only, avoiding food for 30-45
min. after being swallowed.
• Dyspepsia is a recognized side effect, and they
should be prescribed cautiously in patients with
GERD and avoided in those with oesophageal
stricture or achalasia.
• Osteonecrosis of the jaw (rare) and influenza like
illness (with zolendronic acid) are other side
effects

Calcium and vitamin D
supplement
• Calcium in a dose of 500 mg/day, and
vitamin D in a dose of 800 unit/day are
adjunctive to other treatments.
• Monotherapy with calcium and vitamin D
prevents fragility fracture in those with
vitamin D deficiency, but not in other
patients.

Hormone replacement
therapy (HRT)
• HRT prevents postmenopausal bone loss
and reduces the risk of osteoporotic
fractures.
• The use of HRT as a treatment of
osteoporosis has markedly reduced after
confirming the excess risk of breast cancer,
thromboembolism, stroke and CHD.
• Testosterone is indicated for male
osteoporosis caused by hypogonadism.

Follow up after treatment
• Monitoring response to treatment is ideally
made by repeating BMD measurement or by
measuring markers for bone turnover (like
N-telopeptide) in serum or urine
• Second assessment of BMD is made after 2
– 3 years of treatment because of the slow
effect of antiresorptive therapy
