
Acute poisoning

Acute poisoning
• Common medical emergency
• Its incidence varies in different countries
• Substances involved in poisoning vary as well
• Paracetamol poisoning is very common in UK (48% of all
cases of poisoning), while it is rare in Iraq.
• Organophosphorus poisoning on the other hand is very
common in developing countries including Iraq.

Assessment of an acutely poisoned
patient
• First aid measure
• History taking
• Standard clinical examination
• Laboratory investigation

First aid measure
First aid measure should ensure that:
• Airway is clear
• Breathing is adequate
• Circulation is not compromised
History taking
History taking should include:
• Establishing the diagnosis of poisoning
• Calculating the duration since exposure to the
toxic substance
• Identification of the drug or substance abused
• Asking about the cause of poisoning
• Considering the symptoms since poisoning
• Asking about past medical and psychiatric history
Clinical examination
Start standard clinical examination esp.
considering:
State of consciousness (better assessed by Glasgow
coma scale)
• Most cases of poisoning can lead to disturbance
of consciousness, but this is especially true in
case of psychotropic drugs.
• In an unconscious patient, carefully exclude
stroke, hypoglycemia, diabetic ketoacidosis, CNS
infection (meningitis and encephalitis), uraemia,
hepatic encephalopathy, and brain injury.
Clinical examination
Pupil size:
• Small (miosis): Opioids (narcotics)
OP (organophosphorus)
• Large (midriasis): Anticholenergics
TCAD
Alcohol
Antihistaminics
Clinical examination
Respiratory rate:
• Reduced: Opioids
Benzodiazapines
• Increased Salicylates
Clinical examination
Blood pressure:
• Hypotension TCAD
Salicylates
Phenthiazines
• Hypertension
agonists
Clinical examination
Heart rate:
• Tachycardia (or tachyarrhythmia): TCAD,
Digoxine
Theophylline
Anticholenergics
Antihistamines
• Bradycardia (or bradyarrhythmia): Digoxine
CCB (calcium channel blockers)
Blockers
Opioids
Clinical examination
Temperature:
• Fever: Anticholenergic
Salicylates
SSRI
• Hypothermia: CNS depressants
Phenthiazines
Clinical examination
• Cerebellar signs (esp. nystgmus):
Anticonvulsants
Alcohol
• Extrapyramidal signs: Phenthiazines
Metoclopromide
• Convulsions: TCAD
Theophylline
Anticonvulsants
NSAIDs
Clinical examination
• Sweating: Salicylates
OP
• Cyanosis: CNS depressants
Methaemoglobinaemia
• Jaundice: Paracetamol
• Needle tracts: Drug abuse

Toxicology study
• Urea, creatinine and electrolytes should be measured in
most patients.
• Arterial blood gases and acid base balance should be
checked in those with significant respiratory or circulatory
symptoms and when the poison is likely to affect acid base
balance
Toxicology laboratory is needed for
• The measurement of serum level of paracetamol (and to a
lesser extent of aspirin) to plan subsequent management.
• Other types of poisoning are diagnosed by urine or gas
chromatography (only in difficult cases and for medico-legal
indications).

General management of acute
poisoning
• A. Prevention of further absorption
• B. Supportive care
• C. Antidotes
• D. Psychiatric consultation

A. Prevention of further absorption
• Removal of clothing and skin washing with
soap and water in case of contamination by
chemicals or pesticides.
• Eye irrigation by normal saline for 15 min. in
case the eye is contaminated.
• Patients breathless or wheezy because of
inhaling toxic gases or fumes should receive
oxygen and bronchodilator nebulization
A. Prevention of further absorption
Ingested poisons are removed by:
• Gastric lavage
• Activated char coal
• Whole bowel irrigation
• Urinary alkalization
• Haemodialysis and haemoperfusion
A. Prevention of further absorption
Gastric lavage:
– Only if potentially life threatening amounts are ingested
(not to be used for acids, alkalis, or petroleum distillates
poisoning).
– No gastric lavage should be attempted in unconscious
patient unless the airways are protected by cuffed
endotracheal tube.
A. Prevention of further absorption
Activated charcoal:
– it adsorbs most toxins and is the method of choice to prevent
further drug absorption.
– For patients poisoned within one hour, 50 gm is given orally.
– The dose can be repeated every 4 hours for carbamazepine,
theophylline poisoning.
– For patients with disturbed consciousness or those who can not
swallow, activated charcoal is administered through nasogastric
tube and the airway should be protected to avoid aspiration
pneumonitis.
– If multiple doses are needed, a laxative (like sorbitol) is given to
avoid intestinal obstruction.
– Certain poisons are not adsorbed by charcoal, including iron,
lithium, acids, alkalis, ethanol, methanol and petroleum
distillates
A. Prevention of further absorption
Whole bowel irrigation:
– Polyethylene glycol is administered orally for potentially toxic
ingestion of iron, lithium, and theophylline.
– One litre is ingested every hour until the rectal effluent is clear.
– Contraindications include GI bleeding or ulceration
Urinary alkalinization:
– Indicated for severe salicylate poisoning
Haemodialysis or haemoperfusion:
– Effective methods of treating severe poisoning by salicylate,
theophylline, carbamazepine, and methanol

B. supportive care
1. Unconscious patients are better treated in
intensive care units with general treatment of
comatose patient provided. Regular recording of
Glasgow coma scale is important.
2. Convulsions are treated with IV diazepam 10mg
IV repeated as necessary.
3. If cardiac complications are present or expected,
the patient is put under continuous ECG
monitoring.
4. Ventilatory support may be needed for those
with respiratory depression.
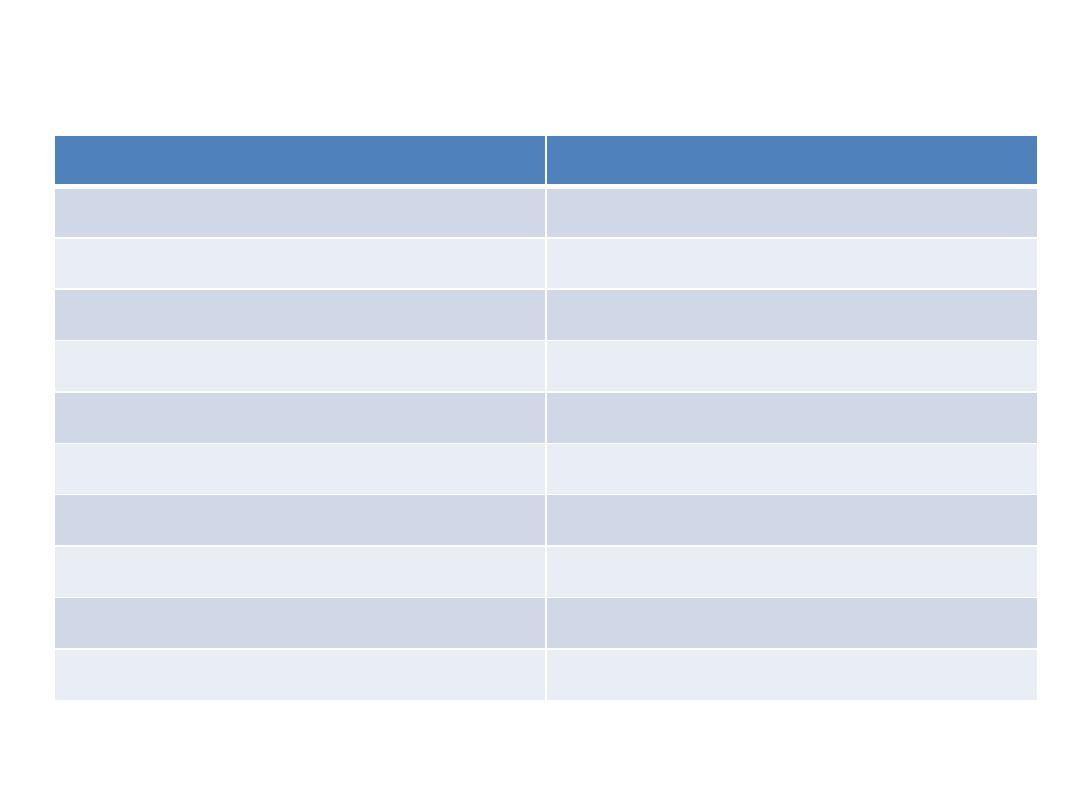
C. Antidotes
Antidote
Poison
Vitamin K, fresh frozen plasma
Anticoagulants (warfarine, rodenticides)
IV glucagon, adrenaline
blockers
Calcium gluconate (or chloride)
Calcium channel blockers
Cobalt edetate, Sodium thiosulphate, Nitrites,
Hydroxycobalamine
Cyanide
Ethanol, 4 methylpyrazol
Methanol,
Ethylene glycol
Naloxone
Opioids (narcotic analgesics)
Atropine, Oximes
OP (organophosphorus compounds)
N. acetylcysteine, Methionine
Paracetamol
Digoxine specific Ab fragments
Digoxine
Desferrioxamine
Iron salts

D. psychiatric consultation
• :
• This is essential for patients who have
attempted suicide.
• The psychiatrist should be consulted as soon
as the patient recovers.

Substances of low toxicity
Certain substances are of very low toxicity even if
ingested in high doses. Examples include:
• most antibiotics (except antiTB, and tetracyclines)
• antiulcer drugs (H2 blockers and PPIs)
• oral contraceptive pills
• chalk
• paper glue
• washing liquids

Common poisoning

Paracetamol poisoning
• Paracetamol in overdosage can cause severe
cenrilobular hepatic necrosis.
• The toxic dose is 10 – 15 gm, while fatal fulminant
hepatic failure is usually associated with ingestion of
25 gm.
• Paracetamol is metabolized to a toxic reactive
metabolite. However, this metabolite is detoxified by
binding to glutathione. When the level of glutathione
depletes, toxicity is expected.
• Symptoms of toxicity include nausea, vomiting,
diarrhea, and right upper abdominal pain.

Management of paracetamol poisoning
• If the patient presents within 1 hour, activated
charcoal is administered.
• Antidote administration is guided by the
results of paracetamol serum level, plotted
against time
• The antidote works by providing glutathione
to detoxify paracetamol toxic metabolite.
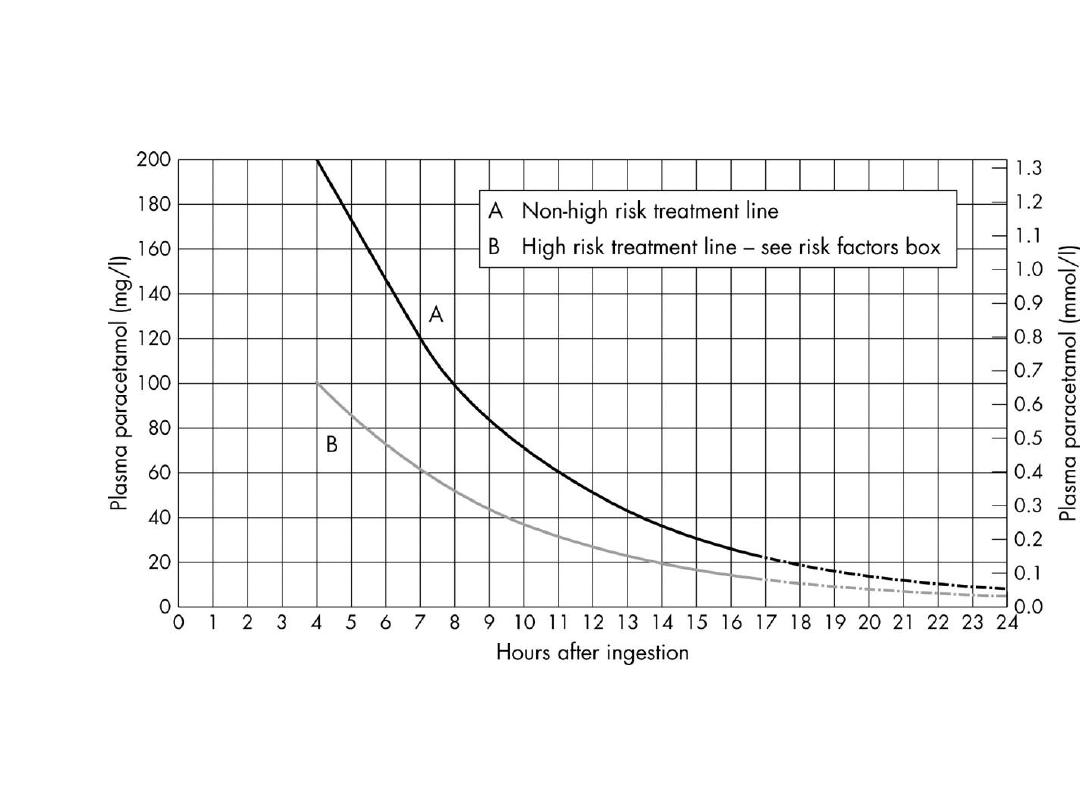

Management of paracetamol poisoning
• The serum level of paracetamol should be taken
4 hours after ingestion.
• If the patient presents after 8 hours, the antidote
should be started before the result of the serum
level is available, because its efficacy diminishes
after 10 h of ingestion.
• For patients who present after 15 h, antidote
therapy is started, liver function tests and
prothrombin time is asked, and liver
transplantation center is consulted.

Management of paracetamol poisoning
• The antidote of choice is N. acetylcysteine which
is highly protective if given in the first 10 hours.
The dose is:
150mg/kg in 200 ml N.S. /15min.
50mg/kg in 500 ml N.S. /4h.
100mg/kg in 1 litre N.S. /20 h.
• Alternatively, methionine 12 gm is given orally
every 4 hours, to be repeated 4 times.

Aspirin (salicylate) poisoning
• Aspirin is toxic when ingested at doses greater
than 150 mg/kg.
• Nausea, vomiting, tinnitus, and deafness are the
initial manifestations.
• Direct stimulation of the respiratory tract causes
hyperventilation (central hyperventilation).
• Moderately severe poisoning is associated with
peripheral vasodilatation, profuse sweating,
petechiae, and subcojunctival haemorrhage.
• Serious poisoning is associated with metabolic
acidosis, renal failure, CNS depression (agitation,
confusion, coma, and fits). Cerebral and
pulmonary oedema may develop

Management of aspirin poisoning
• Activated charcoal is used in multiple doses for
adsorption of the ingested drug.
• Metabolic acidosis is treated with 8.4% NaHCO
3
.
• IV normal saline is required to control severe
dehydration (from sweating and vomiting). Fluids
should be given with caution to avoid precipitating
pulmonary oedema.
• In severe poisoning, urinary alkalinization is needed;
one litre of 1.26% NaHCO
3
is infused over 3 hours,
keeping urine pH around 7.6 – 8.5. Alkaline urine
facilitates aspirin excretion.
• Haemodialysis is very effective in removing salicylate,
and correcting acid base imbalance

Organophosphorus poisoning
• OPs are widely used as pesticides in
agriculture, and as chemical warfare agents.
• There are 3 million cases worldwide each year
around 300000 deaths.
• OP inactivate acetylcholine estase (AchE)
enzyme by phosphorylation leading to
accumulation of acetyl choline (Ach) at
cholinergic synapses (muscarinic, nicotinic,
and central).

Organophosphorus poisoning
• Muscarinic effects:
miosis bradycardia (tachycardia in 20% of cases)
bronchorhoea salivation
lacrimation abdominal pain
bronchoconstriction
• Nicotinic effects:
muscle fasciculation
hyperreflexia
flaccid paralysis and hyporeflexia
• CNS effects:
headache dizziness
confusion coma
fits respiratory depression

Management of OP poisoning
• Atropine (1.8 – 3 mg) is injected as a bolus immediately (3 -6
ampoules), repeated every 5 minutes until atropinization (clear
lung, dry tongue, normal pulse rate, and dilated pupils).
• Once atropinization is complete, 20 – 30% of the bolus dose
required is infused/ hour.
• Treatment should be continued for several days to avoid
relapse.
• Atropine is a muscarinic receptor antagonist, effective in
relieving the muscarinic effects of the toxins only.
• Oxime derivatives (pralidoxime and obidoxime) reactivate
phosphorylated AchE, and can reverse the nicotinic effects of
OP toxins.
• CNS effects are treated by diazepam for convulsions, oxygen
and ventilatory support for respiratory failure

Delayed complications of OP poisoning
• After the acute cholinergic crisis is over, some
patients develop an intermediate syndrome
(around 48 hours later). Muscle weakness and
respiratory paralysis develop due to
downregulation of the nicotinic receptors due to
accumulated Ach.
• Rarely, OP induced delayed polyneuropathy may
occur 1 – 3 weeks after the initial exposure due
to degeneration of long myelinated nerve fibers.
The disability it causes may recover partially after
1- 2 years.

Digoxine poisoning
Clinical features:
• nausea, vomiting, diarrhoea
• visual symptoms
• confusion
• hyperkalaemia
• variable brady-, tachyarrhythmia.

Digoxine poisoning
Treatment:
• Specific antidote (digoxine antibody Fab
fragments)
• Continuous ECG monitoring
• Volume replacement in case of hypotension (
enotropics)
• Correction of hypokalaemia and
hypomagnesaemia
• Atropine for bradyarrythmias
• Tachyarrythmias, accordingly
Tricyclic antidepressants poisoning
Clinical features:
• hypotension and variable arrhythmias (negative
enotropic effect and arrythmogenic)
• warm dry skin
• convulsions
Treatment:
• volume replacement
vasopressor agent
• cotiuous ECG monitoring
• sodium bicarbonate (NaHCO3) 8.4%; in case of
prolonged QRS complex or tachyarrhythmias

Selective serotonin reuptake inhibitors
(SSRIs)
• These drugs are less cardiotoxic than TCAD.
• However, in large doses SSRIs can still cause
hypotension and arrhythmias, as well as
fever.
• The treatment of toxicity is similar to TCAD.
Clinical manifestation
Drug poisoning
Drowsiness, disturbed consciousness,
and coma.
Cerebellar signs, fits
Cardiovascular toxicity
Anticonvulsants (carbamazepine,
phynetoin)
Arrhythmias, fits and coma
Theophylline
Epigastric pain, nausea, and vomiting
Convulsions (10 – 20%)
NSAIDs
Hypotension, drowsiness, and fits
Phenthiazines
Drowsiness, cardiac arrhythmias
Antihistamines
Vomiting, haematamesis, abdominal
pain, fits
Iron salts
