1
Tremor
WHAT IS TREMOR AND HOW SHOULD WE DESCRIBE IT?
Tremor is a rhythmic oscillation of a body part.
Further description can include which part or parts of the body it
affects and its frequency of oscillation, usually in Hertz (1 Hz = 1 tremor
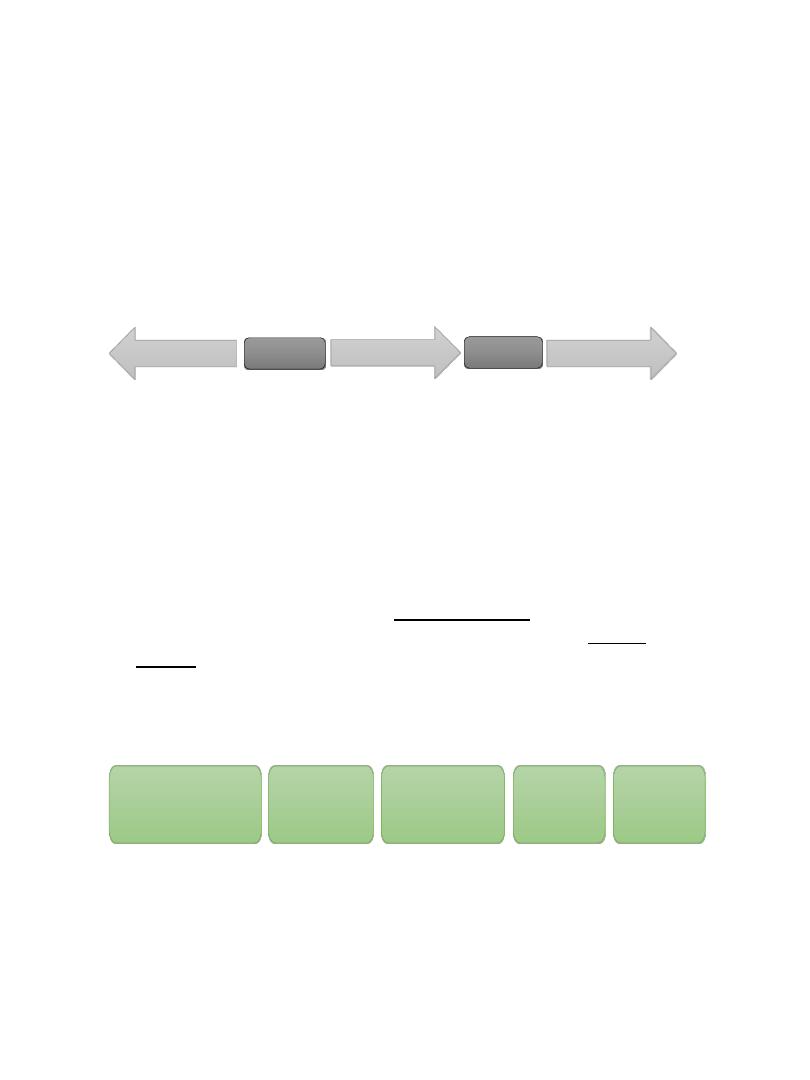
oscillation per second). the frequency of tremors can be separated into
different categories: low frequency, less than 4 Hz; mid-frequency, 4
Hz to 7 Hz; high frequency, more than 7 Hz).
A tremor might also be described on the basis of its amplitude: some
tremors have a very small amplitude (usually called fine tremors),
while others have large amplitude (usually called coarse tremors).
Some tremors are variable in amplitude and frequency and may be
described as jerky.
Tremors are usually also described by the context in which they are
present, as follows:
1. Rest tremor.
2. Action tremor. Which include Postural tremor: tremor present
when the arms (typically) are held up by the patient. Kinetic
tremor: tremor present during movement; may significantly
worsen toward the end of movement, as in ‘‘finger-nose’’ testing
(this is called an intention tremor).
NB So to describe tremor we should mention;
For example, the description ‘‘A 60-year-old man with tremor’’
presents a long differential diagnosis list, whereas ‘‘A 60-year-old
7
Hz
4
Hz
High frequency
Low frequency
Mid frequency
Rythmic oscillation
Part of body
Frequency in Hz
amplitude
contex
2
man with a coarse 3-Hz to 4-Hz tremor affecting the right hand,
present at rest, re-emerging on posture after a few seconds,
absent during movement’’ or ‘‘A 60-year-old man with a fine, 6-
Hz to 8-Hz, bilateral, symmetrical, postural, and kinetic tremor
affecting the arms’’ offer much smaller lists of possibilities,
(Parkinson disease [PD] in the first case and essential tremor,
hyperthyroidism, or drug side effects in the second).
TREMOR PRESENT MAINLY AT REST
Parkinson Disease
Parkinson Disease is the most common cause of resting tremor, other
causes include
1. Drug-induced parkinsonism
2. Vascular parkinsonism
The resting tremor of Parkinson disease usually start on one side of the
body first and over time spread to involve the other side, Many patients
with PD are initially not aware of their tremor, and it is often noticed by
a relative or friend first.
Part of body The tremor often involves the thumb and forefinger; this
gives rise to the term ‘‘pill-rolling’’ although it can present as wrist
flexion/extension or forearm pronation/supination tremor.
Patients with PD may also have tremor outside the arms, most typically
the leg and jaw. Head tremor is not a common feature of PD and occur
in ET.
Dopamine receptor blocking drug like
antipsychotic and antiemetic plasil and
stemetil also other Ca channel blocker,
Depakin, Amiodarone.
3
The frequency is typically 4 Hz to 6 Hz, amplitude is coarse.
Contex resting tremor It is also important to note that tremor is not a
cardinal feature of PD, as rigidity and bradykinesia are, and about 40% of
patients with PD do not have tremor.
NB
TREMOR PRESENT MAINLY ON POSTURE
Essential Tremor
ET is the most common cause of postural tremor.
Age of onset is in the sixties or seventies although a second peak occur at
20 years but it is rare and other causes need to be excluded.
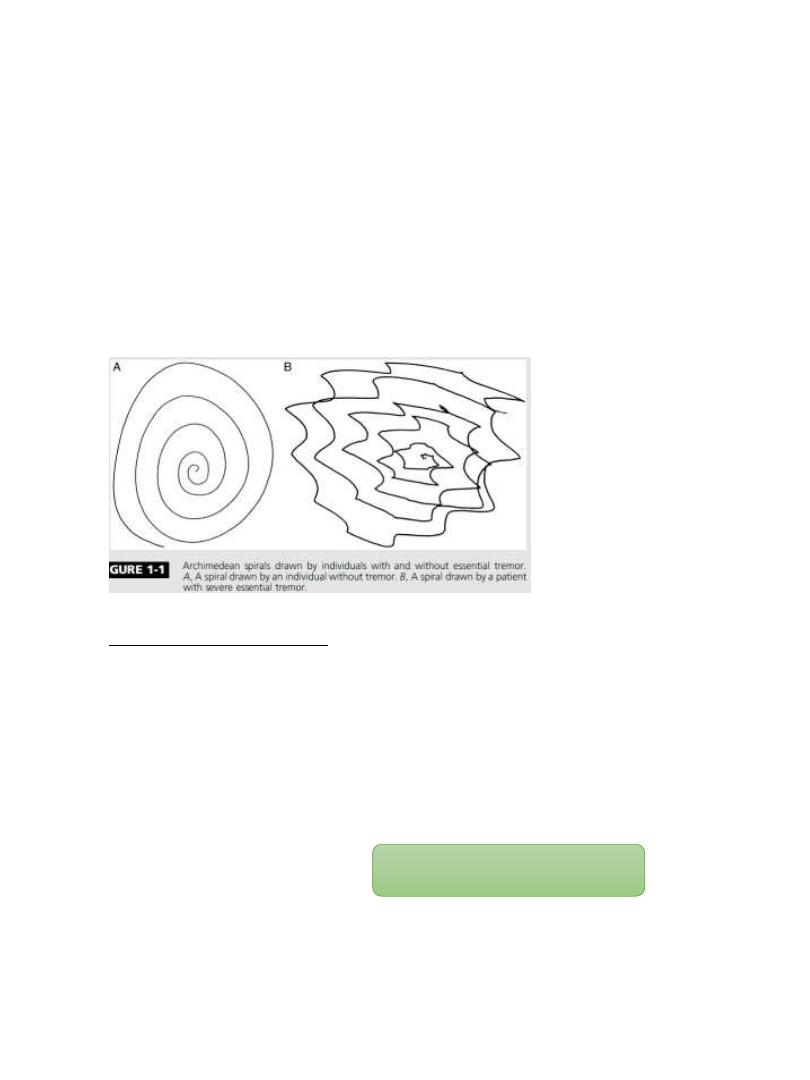
Description part of body bilateral symmetrical affect hand and forearm,
sometimes head frequency 4-12 Hz, amplitude fine tremor, contex
postural and kinetic.
Patients with ET should not develop other neurologic signs (eg, dystonia,
cognitive decline).
Most patients with ET notice a very slow progression of symptoms over
years, and some patients are severely affected (hence, the change in name
from ‘‘benign essential tremor’’ to ‘‘essential tremor’’).
A proportion of patients will report a beneficial effect of a small amount of
alcohol on their tremor.
PD
It is postural tremor but can occur during rest but it is
symmetrical
ET
It is rest tremor but can occur during posture
4
Dystonic Tremor
Other Causes of Mainly Postural Tremor
1. Physiologic tremor.
2. enhanced physiologic tremor. Anxiety and fatigue are commonly
enhance physiological tremor.
3. Drugs
4. Metabolic disturbance, especially due to hyperthyroidism.
TREMOR PRESENT MAINLY DURING MOVEMENT
An important distinction needs to be made between tremor that occurs
during movement of the limb and a true intention tremor, which occurs
only (or very clearly worsens) at the end of movement as in finger-nose
testing which indicate cerebellar cause.
Intention tremors can be combined with resting and postural tremor.
Usually unilateral called rubral or Holmes tremor and is related usually to
an ipsilateral lesion in the brainstem. Although classical descriptions
suggested a lesion in the red nucleus (hence the term ‘‘rubral tremor’’),
most often the lesion is in the midbrain tegmentum outside the red
nucleus, especially in the superior cerebellar peduncle or posterior part of
the thalamus.
A similar tremor, often with a very severe worsening seen when the patient
holds arms in front, flexed at the elbows (a bat’s wing tremor), is
sometimes seen in people with Wilson disease.
psychogenic tremor.
Beta
-
agonists (eg,
salbutamol)
Antidepressant TCA
Anticonvulsants (
especially
sodium
valproate)
Thyroxine
Cocaine
Amphetamines
Caffeine
Nicotine
Alcoholism, mercury
5
How to recognize that the tremor is psychogenic
The best distraction task is to ask patients to tap with one hand in time to a
rhythm set by the examiner that speeds up and slows down unpredictably.
The treating physician should look for a distinct change in the tremor (eg,
long pauses, shift in frequency) or ‘‘entrainment’’ where the tremor adopts
the frequency of the tapping.
An additional useful maneuver is to ask patients to reach quickly to a target,
such as the examiner’s finger, presented suddenly. A brief pause in the
tremor is often seen.
TREMOR HISTORY TAKING AND EXAMINATION
• History
Ask about the following:
1. Age of onset.
2. body part or parts affected.
3. Onset (sudden or gradual).
4. Coarse (static, progressive).
5. Exacerbating factors (including task-specific worsening).
6. Relieving factors (eg, alcohol).
7. Associated neurologic symptoms( gait difficulty), associated systemic
symptoms (hyperthyroidism).
8. Family history.
Examination
1. Examine the patient with his or her arms relaxed, ideally on the arms of a
chair or on the patient’s lap, semi-pronated, Ask the patient to close his
or her eyes and count backward from 100 this distraction task often
brings out tremor.
2. Examine the arms on posture, stretched out in front of the patient,
fingers open. Ask the patient to close his or her eyes and count backward
again. Ask patient to flex his or her arms at the elbows, then slowly
supinate and pronate the arms, looking for position specificity of the
tremor.
6
3. Examine the patient’s arms during movement by doing the finger-nose
test, looking for tremor during movement (kinetic tremor) and any clear
worsening at the end points (intention tremor).
4. Ask the patient to write and copy a Archimedes spiral; this is useful as a
measure of tremor severity for comparison after treatment and also to
look for task-specific tremor.
5. Examine for other neurologic signs, especially parkinsonism, cerebellar
signs and dystonia.
6. Examine for systemic signs (signs of hyperthyroidism).
TREATMENT OF TREMOR
As with many neurologic disorders, treatment of tremor is primarily
symptomatic.
Certain causes of tremor have specific treatments. Therefore, tremor due
to PD is best treated by dopaminergic medications, Other drugs, such as
amantadine, can also reduce tremor due to PD. Tremor due to drug use
or metabolic disturbance such as hyperthyroidism is best treated by
withdrawal of the offending drug or treatment of the metabolic
disturbance, respectively.
For Postural tremor

7
beta blockers, particularly propranolol, have class A evidence. Important
side effects include postural hypotension and bradycardia, and in those
with a history of asthma, propranolol can trigger breathing difficulties.
Hypoglycemic warning symptoms can be masked with beta-blockers.
propranolol can be given at a dose of 10 mg 2 to 3 times per day, and
slowly increased to 20 mg to 30 mg 3 times per day.
Primidone, which is metabolized to phenobarbital, has class A evidence
to support its use in tremor but is problematic, particularly in older
patients, because of sedative side effects and tolerance.
A normal starting dose would be about 25 mg once daily, increasing
slowly to 50mg to 100 mg 3 times per day.
Clonazepam a long-acting benzodiazepine. Side effects include sedation.
Some patients find this a useful drug to use on an ‘‘as needed’’ basis, for
example, taking it before a social engagement.
Starting dose is 0.25 mg daily, increasing slowly to 0.5 mg to 1 mg 3 times
per day. Other medication usually unsuccessful include topiramate and
gabapentin.
For parkinsonism, the regular anti-Parkinson medication should be tried
first, since it has a high likelihood of improving tremor.
Trihexyphenidyl is an anticholinergic medication particularly
effectiveness for dystonic tremor and is also used to treat tremor in PD. It
causes dry mouth and, in older people especially, can cause confusion.
Starting dose is 1 mg daily, increasing slowly to 1 mg to 2 mg 3 times per
day.
Botulinum Toxin it is especially effective for dystonic tremor, head and
jaw tremor.
For Resting tremors

8
Surgery
Patients with severe refractory tremor may benefit from brain
surgery. Thalamotomy (lesioning of a specific part of the thalamus)
and, more recently, deep brain stimulation of the thalamus (VIN
nucleus ventral intermediate) can both produce dramatically
beneficial effects on tremor.
