
1
Hematuria
What is hematuria?
Macroscopic
Visible haematuria
Pink or red
Microscopic
•Gold standard – Microscopy
•Presence of >3 RBCs per high-powered field
Dipsticks
•
Positive – >1 RBCs per high-powered field
•
Higher false positives
Symptomatic vs. non-symptomatic
•
Lower Urinary Tract Symptoms (LUTS)
•
Eg. Dysuria, hesitancy, frequency, urgency

2
Macroscopic Haematuria
Microscopic Haematuria
3
Causes
Renal
•
Malignant renal mass
•
Benign renal mass
•
Glomerular bleeding
•
Structural diseases
•
Pyelonephritis
•
Hydronephrosis
•
Hypercalcinuria / Hyperuricosuria
•
Renal vein thrombosis
•
Renal artery embolism
•
Arteriovenous malformation
Ureteric
•
Malignancy
•
Calculi
•
Strictures
•
Fibroepithelial polyp
•
Fistulas
Bladder
•
Malignancy
•
Radiation
•
Cystitis
•
Prostate/Urethra
•
Benign prostatic hyperplasia
•
Prostate carcinoma
•
Catheterisation
•
Urethritis
History and Examination
•History
•
Time course
•
Infective symptoms
•
Urinary symptoms
•
Associated symptoms
•
Past history
•
Social history
•
Family history
4
•Examination
•
Vital signs
•
Abdominal
•
DRE
Workup
•
Significant haematuria:
•
Single episode of macroscopic haematuria
•
Single episode of symptomatic microscopic haematuria
•
Persistent non-symptomatic microscopic haematuria
•
Initial investigations
•
Exclude transient causes
•
Eg. UTIs, exercise induced, trauma, menstruation
•
Urine cultures
•
Serum creatinine and eGFR
•
Measure for proteinuria
•
Protein:Creatinine ratio (PCR)
•
Albumin:Creatinine ratio (ACR)
•
Blood pressure
Urological Referral
•
All patients with macroscopic haematuria
•
All patients with symptomatic microscopic haematuria
•
All patients with asymptomatic microscopic haematuria who are
aged 35 and over
5
Nephrological Referral
•
Consideration of nephrological referral
•
Declining GFR
•
>10ml/min within the previous 5 years
•
>5ml/min within the last 1 year
•
Stage 4 or 5 CKD (eGFR <30)
•
Significant proteinuria
•
PCR ≥50mg/mmol
•
ACR ≥30mg/mmol
•
Isolated haematuria with hypertension who are aged ≤40
•
Haematuria with coinciding intercurrent infection
6
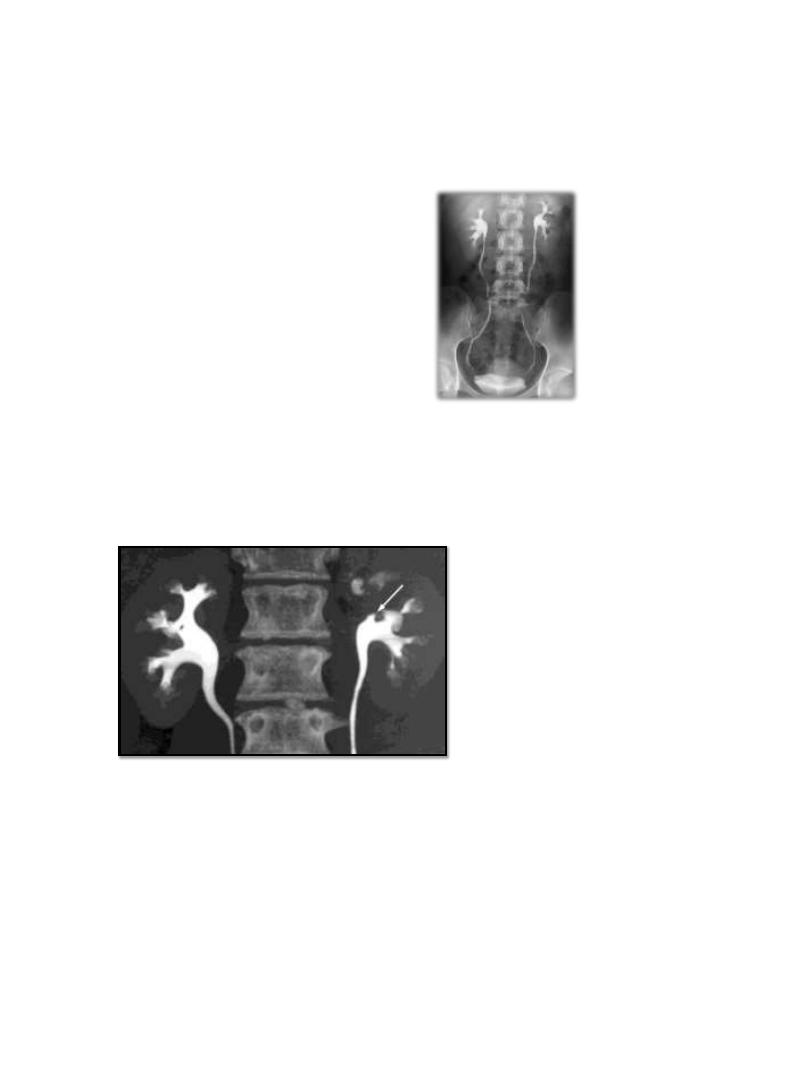
Imaging
•
CT Urography
•
Non-contrast
•
Arterial phase
•
Renal parenchymal phase
•
Excretory phase
•
MR Urography
•
Without and with IV contrast
•
Ultrasound
•
Retrograde pyelogram
•
XR IVP
CT Urography
Procedure
•
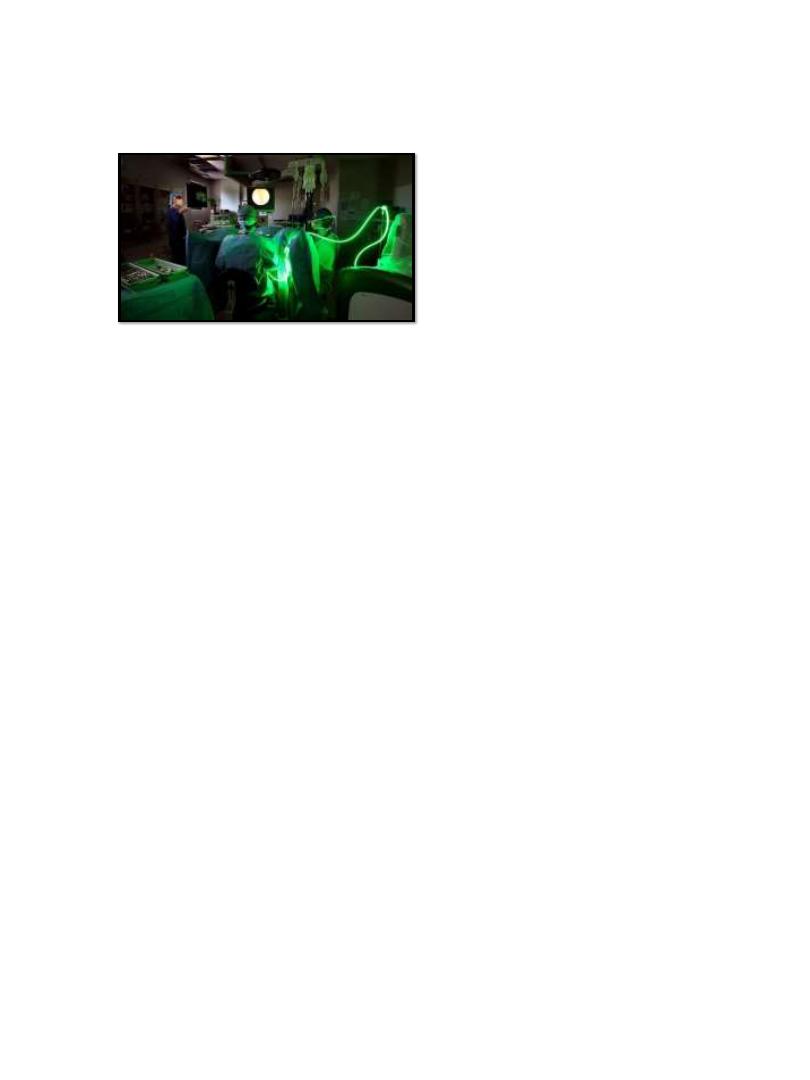
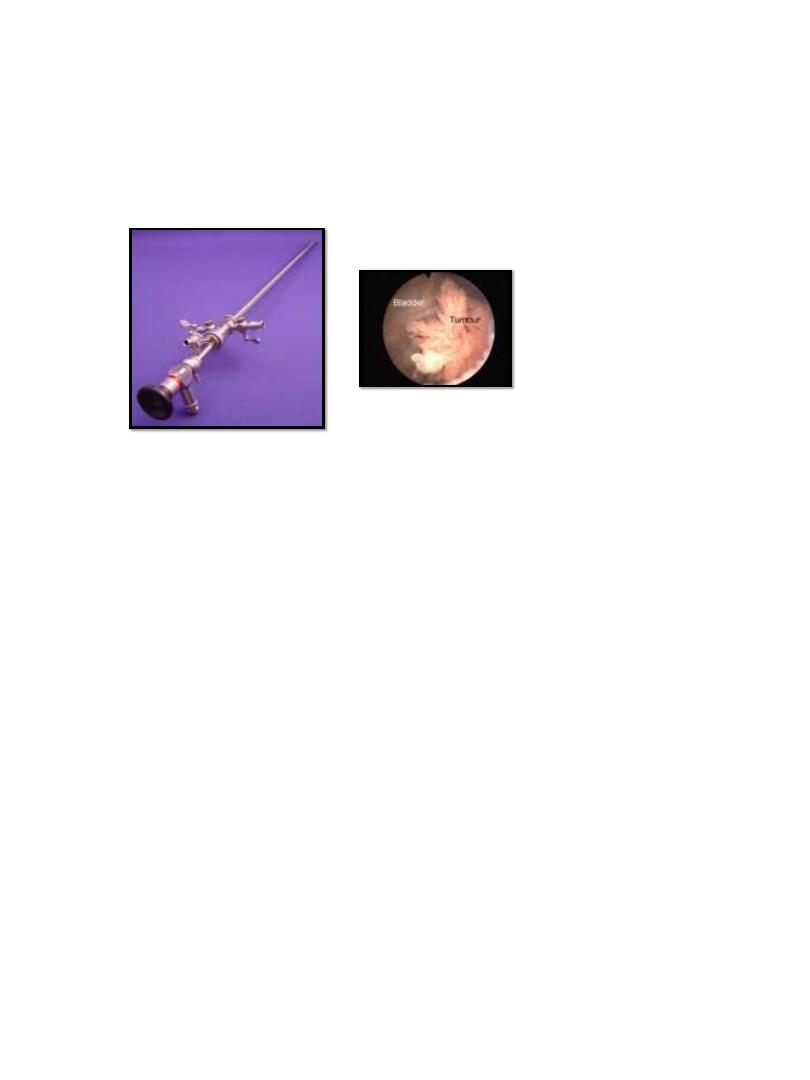
Cystoscopy
•
Full visualisation of the bladder, prostate and urethra
7
•
All haematuria patients aged 35 years and over
•
All patients with risk factors for urinary tract malignancy
Risk Factors
•
Male gender
•
Aged 35 and over
•
Past or current smoker
•
Occupational exposure to chemicals
•
Analgesic abuse
•
History of gross haematuria
•
History of urologic disorder or disease
•
History of irritative voiding symptoms
•
History of pelvic irradiation
•
History of chronic urinary tract infections
•
History of exposure to known carcinogens or chemotherapy
•
History of chronic indwelling foreign body
8
Procedure
Negative Urological Workup
•
Annual assessment
•
Creatinine / eGFR
•
PCR / ACR
•
Blood pressure
•
Monitor
•
Voiding LUTS
•
Macrohaematuria
•
Significant proteinuria
•
Worsening renal function
•
Repeat full urological work-up if persistent haematuria
•
Consider nephrological referral
•
Follow up not required
•
2x consecutive negative annual urinalyses
•
Rigid cystoscopy
9
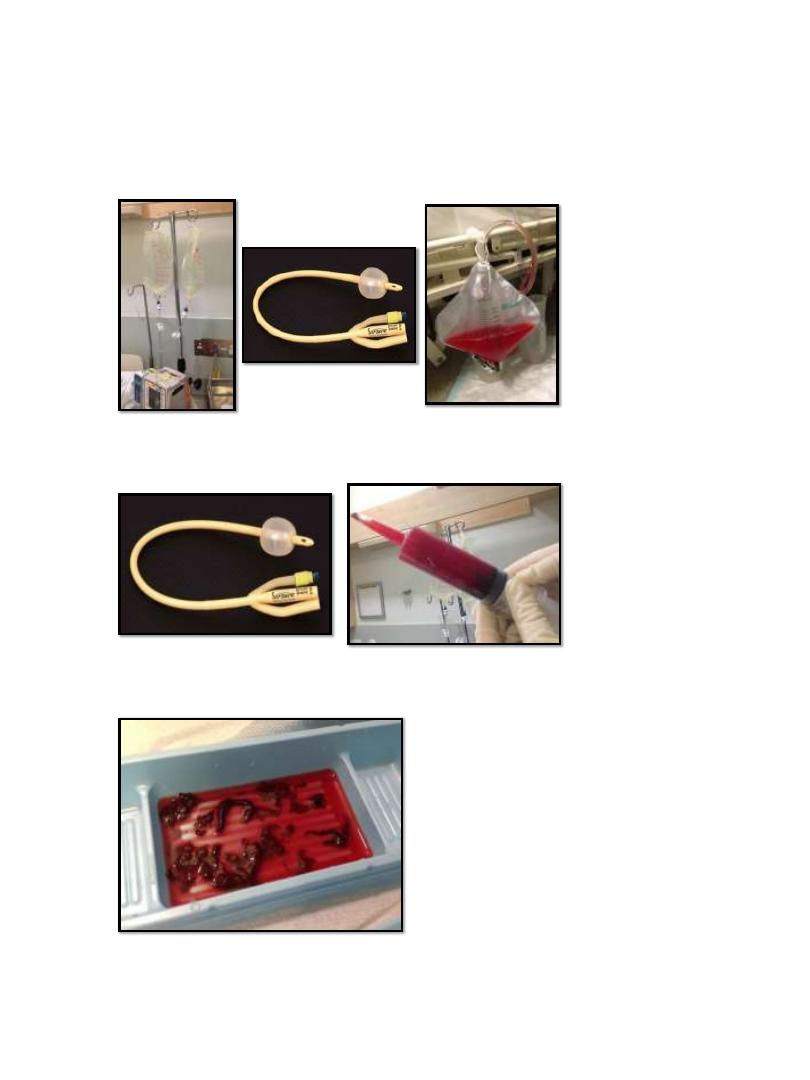
Continuous Bladder Irrigation
Manual Bladder Washout
Manual Bladder Washout
