1
HEART FAILURE
DEFINITION
•
Heart failure describes the clinical syndrome that develops when the
heart cannot maintain adequate output, or can do so only at the
expense of elevated ventricular flling pressure.
•
In mild to moderate forms of heart failure, cardiac output is normal at
rest and only becomes impaired when the metabolic demand
increases during exercise or some other form of stress.
•
In practice, heart failure may be diagnosed when a patient with
signifcant heart disease develops the signs or symptoms of a low
cardiac output, pulmonary congestion or systemic venous congestion.
Almost all forms of heart disease can lead to heart failure. An accurate
aetiological diagnosis is important because treatment of the
underlying cause may reverse heart failure or prevent its progression

2
Types of heart failure
Left, right and biventricular heart failure
The left side of the heart comprises the functional unit of the LA and
LV, together with the mitral and aortic
valves; the right heart comprises the RA, RV, and tricuspid and
pulmonary valves.
•
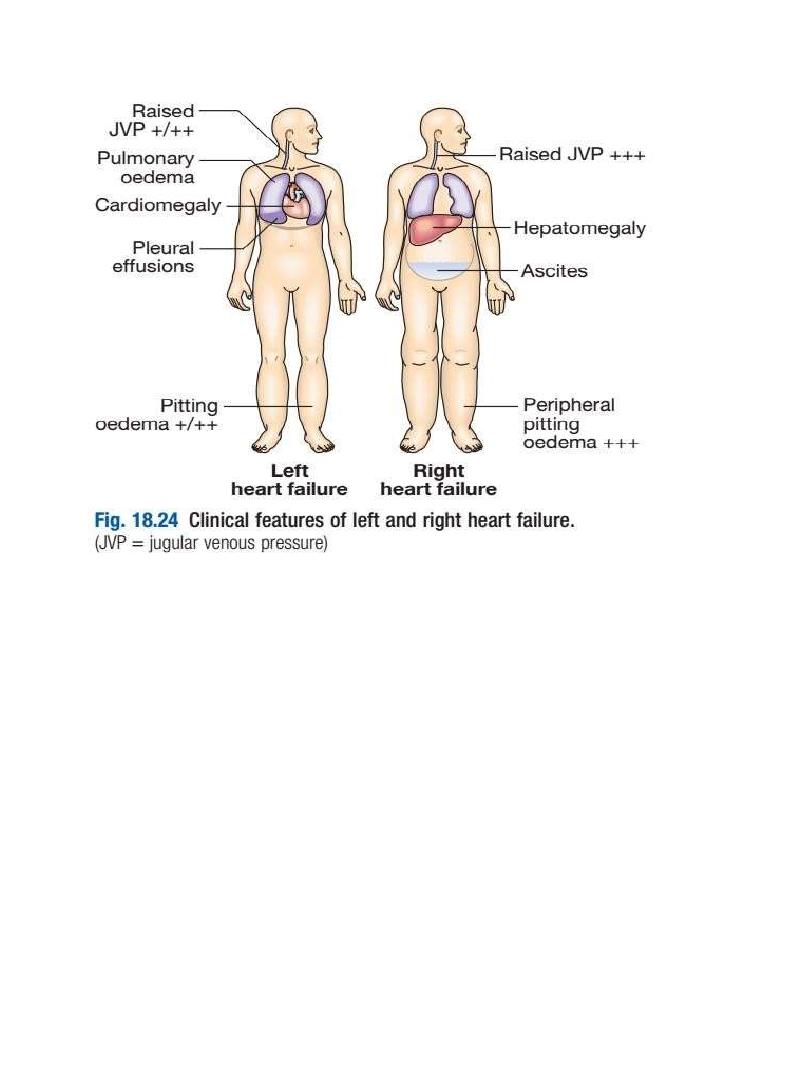
Left-sided heart failure :
There is a reduction in left ventricular output and an increase in left
atrial and pulmonary venous pressure. An acute increase in left atrial
pressure causes pulmonary congestion or pulmonary oedema; a more
gradual increase in left atrial pressure, as occurs with mitral stenosis,
leads to reflex pulmonary vasoconstriction, which protects the patient
from pulmonary oedema. This increases pulmonary vascular resistance
and causes pulmonary hypertension, which can, in turn, impair right
ventricular function.
•
Right-sided heart failure
There is a reduction in right ventricular output and an increase in right
atrial and systemic venous pressure. Causes of isolated
right heart failure include chronic lung disease (cor pulmonale),
pulmonary embolism and pulmonary valvular stenosis.
• Biventricular heart failure
Failure of the left and right heart may develop because the disease
process, such as dilated cardiomyopathy or ischaemic heart disease,
affects both ventricles or because disease of
the left heart leads to chronic elevation of the left atrial pressure,
pulmonary hypertension and right heart failure.
Diastolic and systolic dysfunction
Heart failure may develop as a result of impaired myocardial
contraction (systolic dysfunction) but can also be due to poor
ventricular flling and high flling pressures stemming from abnormal

3
ventricular relaxation (diastolic dysfunction). The latter is caused by a
stiff, noncompliant ventricle and is commonly found in patients with
left ventricular hypertrophy. Systolic and diastolic
dysfunction often coexist, particularly in patients with coronary artery
disease.
High-output failure
A large arteriovenous shunt, beri-beri , severe anaemia or
thyrotoxicosis can occasionally cause heart failure due to an
excessively high cardiac output.
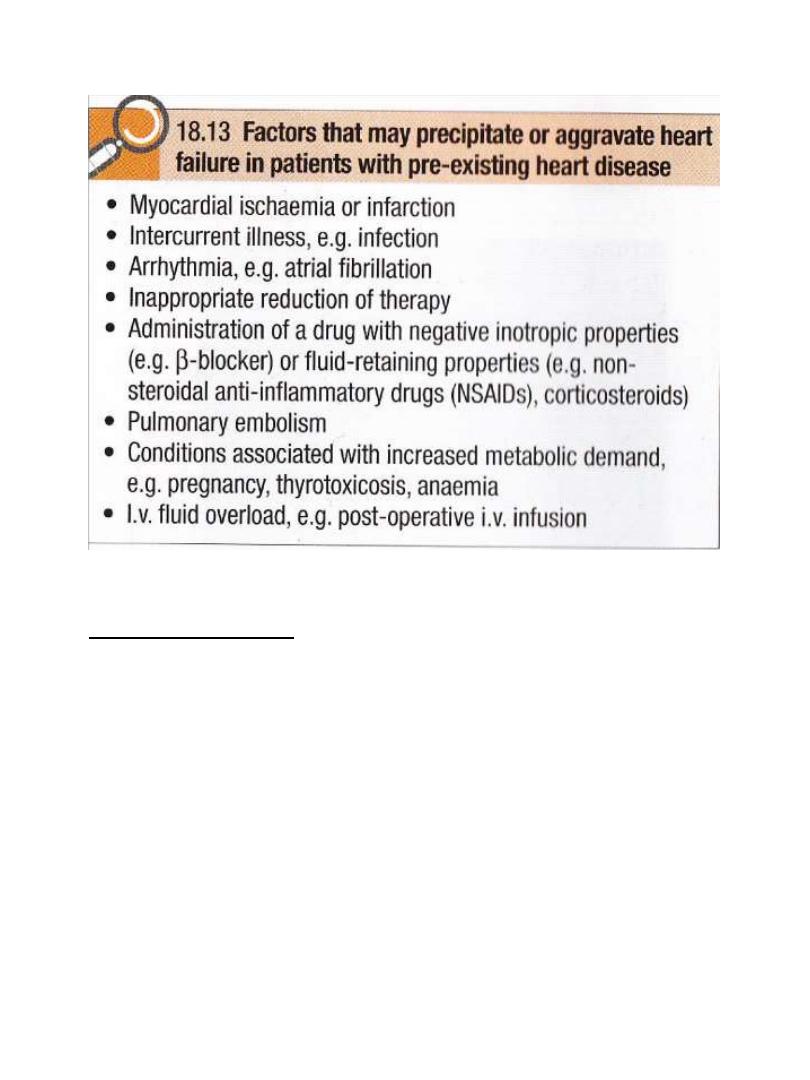
Acute and chronic heart failure
Heart failure may develop suddenly, as in MI, or gradually, as in
progressive valvular heart disease. When there is gradual impairment
of cardiac function, several compensatory changes may take place.
The term ‘compensated heart failure’ is sometimes used to describe
the condition of those with impaired cardiac function, in whom
adaptive changes have prevented the development of
overt heart failure. A minor event, such as an intercurrent infection or
development of atrial fbrillation, may precipitate overt or acute heart
failure . Acute left heart failure occurs, either de novo or as an acute
decompensated episode, on a background of chronic heart failure: so-
called acute-onchronic heart failure.
4
Clinical Assessment
• Acute left heart failure
Acute de novo left ventricular failure presents with a sudden onset of
dyspnoea at rest that rapidly progresses to acute respiratory distress,
orthopnoea and prostration. The precipitant, such as acute MI, is often
apparent from the history.
The patient appears agitated, pale and clammy. The peripheries are
cool to the touch and the pulse is rapid.
Inappropriate bradycardia or excessive tachycardia should be identifed
promptly, as this may be the precipitant for the acute episode of heart
failure. The BP is usually high because of sympathetic nervous system
activation, but may be normal or low if the patient is in cardiogenic
shock The jugular venous pressure (JVP) is usually elevated,
particularly with associated fluid overload or right heart failure. In
acute de novo heart failure, there has been no time for ventricular

5
dilatation and the apex is not displaced. A ‘gallop’ rhythm, with a third
heart sound, is heard quite early in the development of acute leftsided
heart failure. A new systolic murmur may signify acute mitral
regurgitation or ventricular septa rupture. Auscultatory fndings in
pulmonary oedema are fine basal end-inspiratory crepitations at the
lung bases, or throughout the lungs if pulmonary oedema is severe.
Expiratory wheeze often accompanies this.
Acute-on-chronic heart failure will have additional features of long-
standing heart failure. Potential precipitants, such as an upper
respiratory tract infection or inappropriate cessation of diuretic
medication, should be identifed.
• Chronic heart failure
Patients with chronic heart failure commonly follow a relapsing and
remitting course, with periods of stability and episodes of
decompensation, leading to worsening symptoms that may
necessitate hospitalisation. The clinical picture depends on the nature
of the underlying heart disease, the type of heart failure that it has
evoked, and the neurohumoral changes that have developed
Low cardiac output causes fatigue, listlessness and a poor effort
tolerance; the peripheries are cold and the BP is low. To maintain
perfusion of vital organs, blood flow is diverted away from skeletal
muscle and this may contribute to fatigue and weakness. Poor renal
perfusion leads to oliguria and uraemia.
Pulmonary oedema due to left heart failure presents as above and
with inspiratory crepitations over the lung bases. In contrast, right
heart failure produces a high JVP with hepatic congestion and
dependent peripheral oedema. In ambulant patients, the oedema
affects the ankles, whereas, in bed-bound patients, it collects around
the thighs and sacrum. Ascites or pleural effusion may occur .
Chronic heart failure is sometimes associated with marked weight loss
(cardiac cachexia), caused by a combination of anorexia and impaired
absorption due to gastrointestinal congestion, poor tissue perfusion
due to a low cardiac output, and skeletal muscle atrophy due to
immobility.
6
Investigations
1. Blood gas analysis
2. Renal function test
3. Hb & PCV
4. Thyroid function test
5. ECG
6. BNP (brain natriuretic peptide)
7. Echocardiography
8. Chest X ray

7
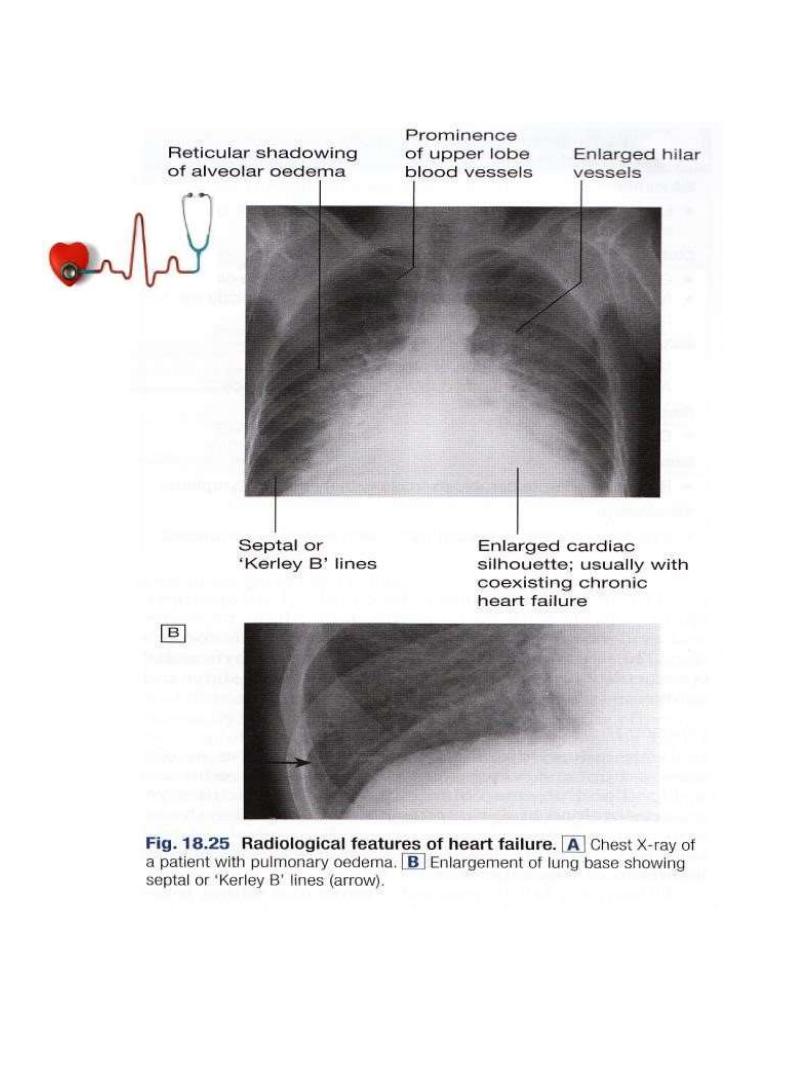
Chest X ray
High pulmonary venous pressure in left-sided heart failure frst shows
on the chest X-ray as an abnormal distension of the upper lobe
pulmonary veins (with the patient in the erect position). The
vascularity of the lung felds becomes more prominent, and the right
and left pulmonary arteries dilate. Subsequently, interstitial oedema
causes thickened interlobular septa and dilated lymphatics. These are
evident as horizontal lines in the costophrenic angles (septal or ‘Kerley
B’ lines). More advanced changes due to alveolar oedema cause a hazy
opacifcation spreading from the hilar regions, and pleural effusions
X ray findings in heart failure
•
Chronologically…
•
In CXR..
•
Hilar opacities
•
Bat wing or butterfly appearance
•
Prominent upper lobe vessels
•
Kerley B lines
•
Encysted fissural edema (vanishing tumor) which is accumulation of
fluid in the fissural space between 2 lobes, giving in x-ray an opacity
that look like a tumor ,which however, resolve by diuretics
•
Later… cardiomegaly,,, and in advanced heart failure,there may be
pleural effusion
8

9
Mx of Acute Pulmonary Edema
This is an acute medical emergency:
•
Sit the patient up to reduce pulmonary congestion, with complete bed
rest.
•
Give oxygen (high-flow, high-concentration).
Non-invasive positive pressure ventilation (continuous positive airways
pressure (CPAP) of 5–10 mmHg) by a tight-ftting facemask results in a
more rapid clinical improvement.
•
Administer nitrates, such as IV glyceryl trinitrate (10–200 µg/min or
buccal glyceryl trinitrate 2–5 mg, titrated upwards every 10 minutes),
until clinical improvement occurs or systolic BP falls to less than 110
mmHg.
•
Administer a loop diuretic, such as furosemide (50–100 mg IV).
The patient should initially be kept rested, with continuous monitoring
of cardiac rhythm, BP and pulse oximetry. Intravenous opiates, like
morphin 5-10mg must be used sparingly in
distressed patients, as they may cause respiratory depression and
exacerbation of hypoxaemia and hypercapnia.
If these measures prove ineffective, inotropic agents(Dobutamine)
may be required to augment cardiac output, particularly in
hypotensive patients. Insertion of an intra-aortic balloon pump may be
benefcial in patients with acute cardiogenic pulmonary oedema and
shock.
Rotating tourniquet to reduce preload
Hemofiltration is among last choices in unresponsive cases
Mechanical ventilation in unresponsive hypoxia, hypercapnia,
disturbed level of consciousness with low spO2
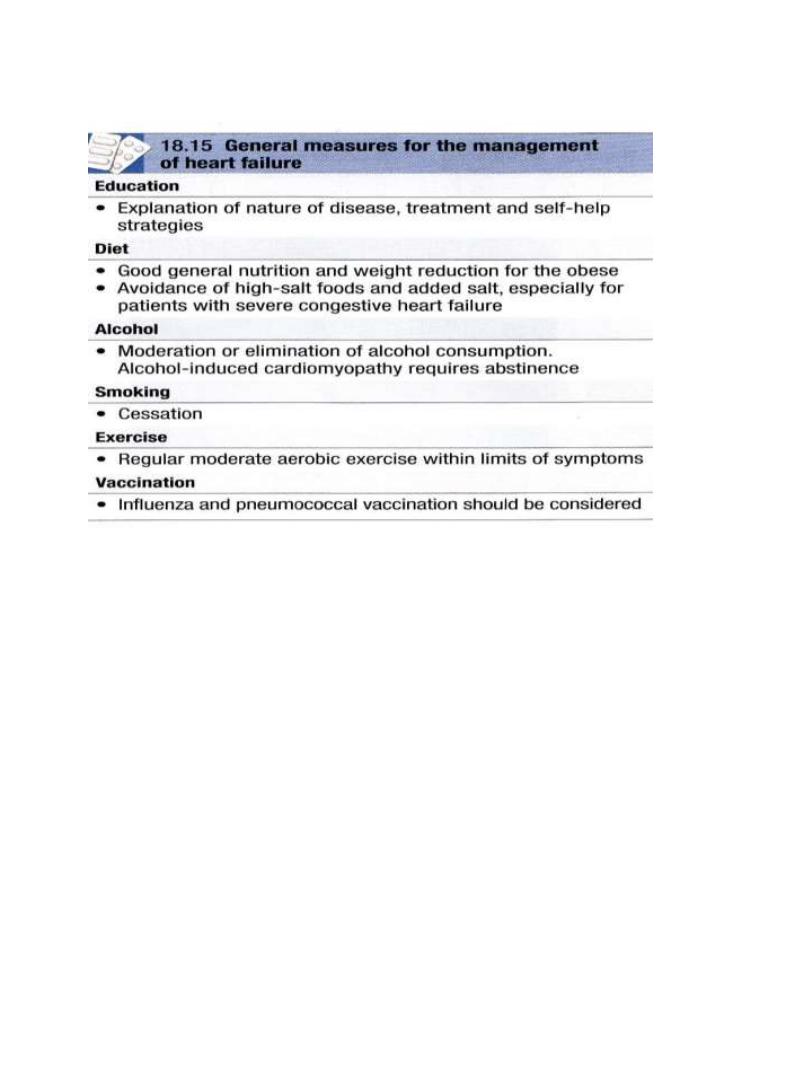
Management of chronic heart failure
•
General measures
•
Drug therapy
10
General measures
Drug therapy
•
Diuretic therapy (FUROSEMIDE & SPIRONOLACTONE)
•
Vasodilator therapy (Venodilator..nitrates ,,arteriodilator..hydralazine)
•
Angiotensin-converting enzyme (ACE) inhibition therapy.
•
Angiotensin receptor blocker (ARB) therapy.
•
Beta-adrenoceptor blocker therapy, small dose ..ex Bisoprolol
•
Digoxin (HF with AF only..)
•
Amiodarone (chemical cardioverter)
•
Ivabradine
•
For details,, see DAVIDSON P.551, 552, 553

11
Drugs that improve prognosis in heart failure
•
B- blockers
•
Spironolactone
•
ACE inhibitors
•
Nitrates
•
Angiotensin neprilysin inhibitor
Non pharmacological Options
•
IMPLANTABLE CARDIAC DEFIBRILLATOR
•
CORONARY REVASCULARISATION
•
CARDIAC RESYNCRONIZATION THERAPY
•
VENTRICULAR ASSIST DEVICE
•
CARDIAC TRANSPLANTATION
•
CARDIOPULMONARY TRANSPLANTATION
