
1
Fifth stage
Neurology
Lec-5
.د
بشار
18/12/2016
Epilepsy
Seizures: are disorders characterized by excessive or over synchronized discharges of
cerebral neurons.
A seizure is a transient disturbance of cerebral function caused by an abnormal neuronal
discharge.
Epilepsy
A condition in which an individual suffers from recurrent epileptic seizures which is not
temporary.
Epilepsy, a group of disorders characterized by recurrent seizures, is a common cause of
episodic loss of consciousness.
Convulsion
The overt, major motor manifestations of a seizure (rhythmic jerking of the limbs).
Aura
Subjective disturbance of perception that represents the start of certain seizures (actually
represents a focal electrical disturbance at the start of the seizure).
Ictus or Ictal phase
The seizure itself; the part of the event where the convulsion occurs or when the brain
activity consists of paroxysmal firing of brain neurons.
Post-ictal phase
The period after the convulsion or actual seizure where the “brain is tired” and the
individual is sleepy, confused, disoriented or experiences temporary neurological
dysfunction.
Interictal
Between seizure.
The recurrence rate after a single seizure is about 70 % within the first year, and most
recurrent attacks occur within a month or two of the first.
Furthur seizures are less likely if a trigger factor is definable and avoidable.

2
Trigger Factors
Sleep deprivation
Alcohol (particularly withdrawal)
Recreational drug misuse
Physical and mental exhaustion
Flickering lights, including TV and computer screens (primary generalized epilepsies
only)
Intercurrent infections and metabolic disturbances
Uncommonly: loud noises, music, reading, hot baths
Seizure type
Partial (simple or complex)
Partial with secondary generalization
Absence
Tonic-clonic
Tonic
Atonic
Myoclonic
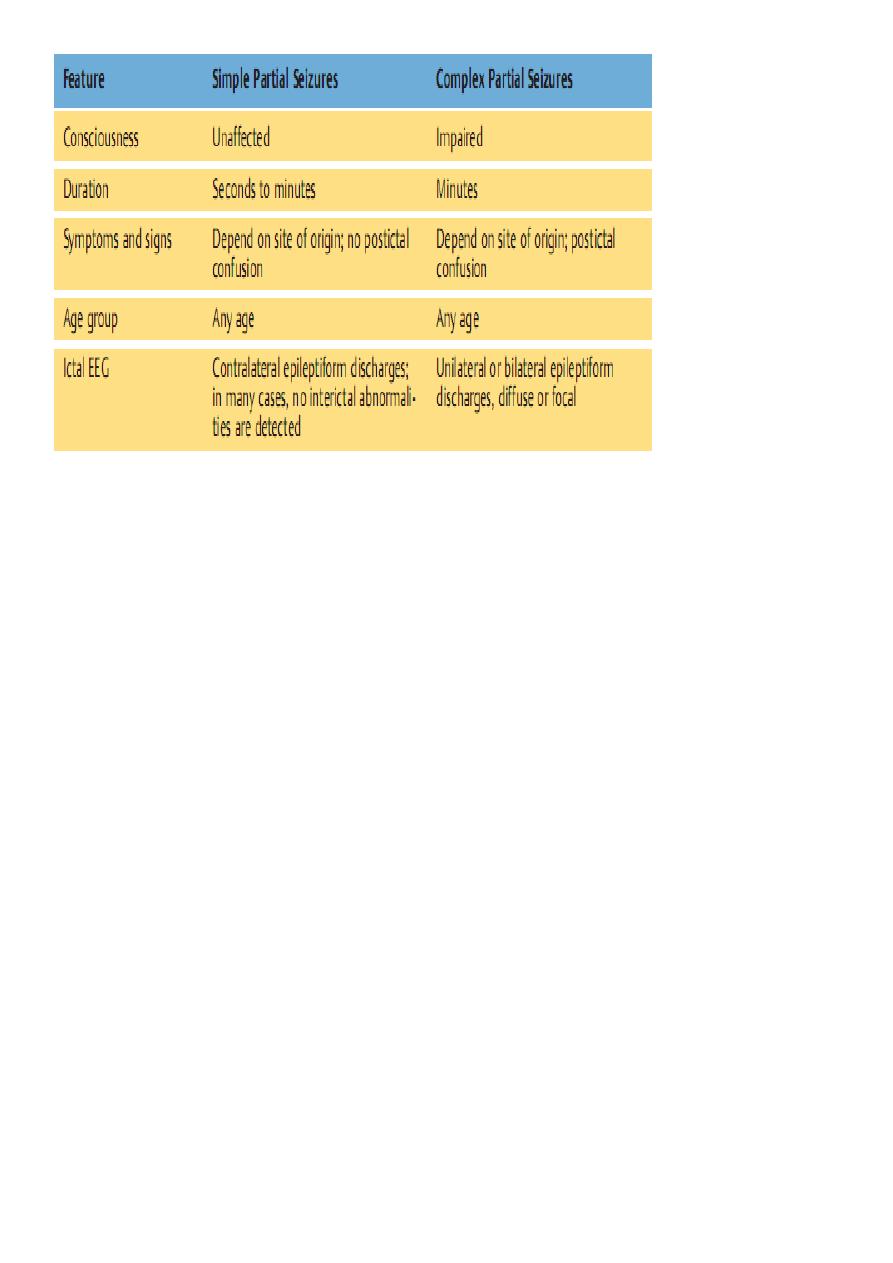
Partial Epilepsy
Partial seizures may arise from any disease of the cerebral cortex, congenital or acquired,
and frequently, generalize.
With the exception of few idiopathic partial epilepsies of benign outcome in childhood, the
presence of partial seizures signifies the presence of focal cerebral pathology.
Causes of partial epilepsy ))((لالطالع
Idiopathic
o Benign Rolandic epilepsy of childhood
o Benign occipital epilepsy of childhood
Focal structural lesions
Genetic
o Tuberous sclerosis
o Neurofibromatosis
o Von Hippel-Lindau disease
o Cerebral migration abnormalities
Infantile hemiplegia
Dysembryonic
3
o Cortical dysgenesis
o Sturge-Weber syndrome
Mesial temporal sclerosis (associated with febrile convulsions
Cerebrovascular disease
o Intracerebral hemorrhage
o Cerebral infarction
o Arteriovenous malformation
o Cavernous haemangioma
Tumors (primary and secondary)
Trauma (including neurosurgery)
Infective
o Cerebral abscess (pyogenic)
o Toxoplasmosis
Secondary generalized epilepsy
Generalized epilepsy may arise from spread of partial seizures due to structural disease, or
may be secondary to drugs or metabolic disorders. Epilepsy presenting in adult life is almost
always secondary generalized, even if there is no clear history of a partial seizure before the
onset of the major attack (an aura).
The occurrence of epilepsy in those over the age of 60 is frequently due to CVD.
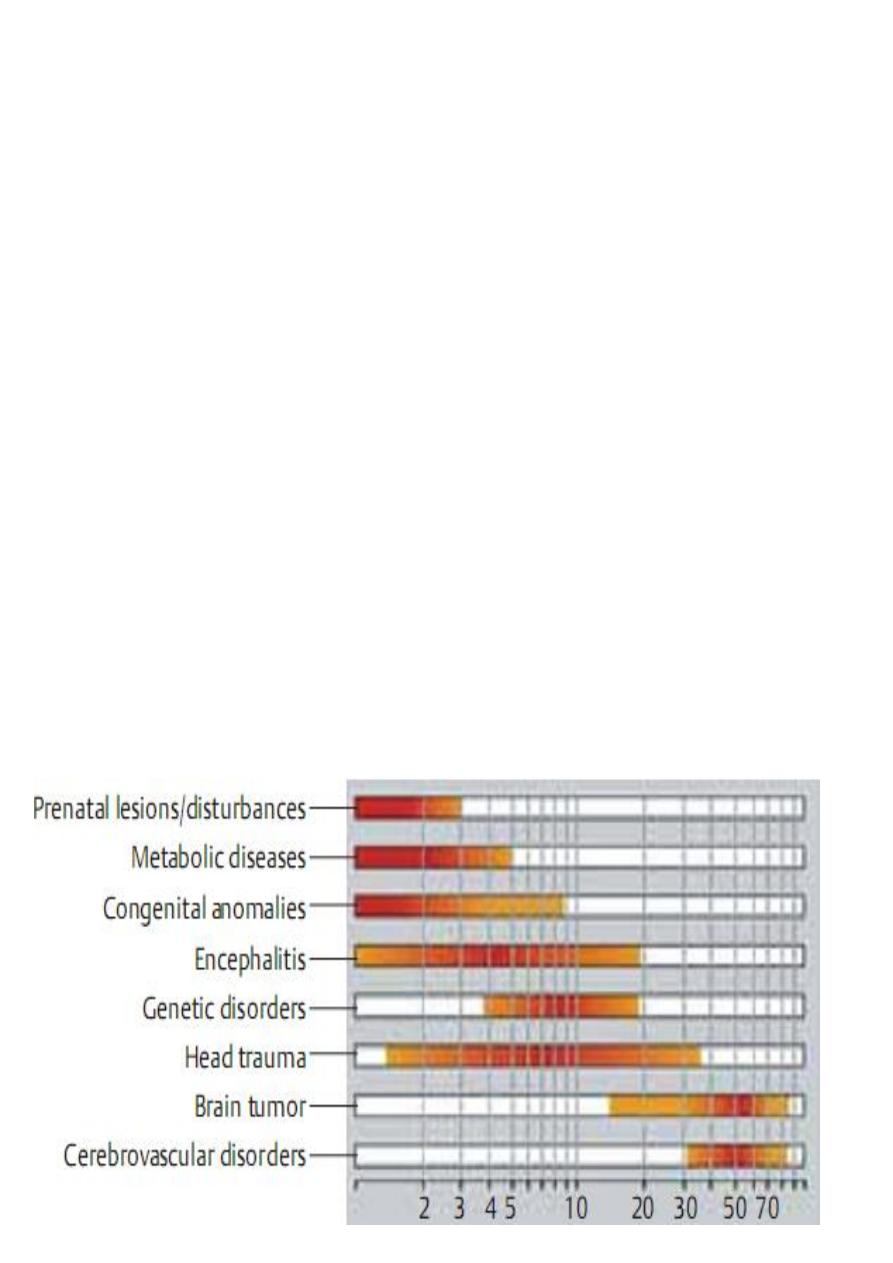
Etiology and age of onset )) ((مهم جدا

4
Pathophysiology
1- An epileptic seizure represents the abnormal (pathological) paroxysmal, synchronous
firing of a group of (usually) cortical neurons.
This group of neurons is referred to as the seizure focus.
2- Disturbance in the normal balance between inhibition and excitation
a) Neuronal depolarization vs. Repolarization.
b) Propagation vs. limitation of inter-neuronal transmission
c) Glutamate vs. GABA
New developments
In some inherited, familial epileptic syndromes, ion channel defects have been discovered
which are presumably responsible for the disturbance in neuronal excitability.
Example
1- Benign neonatal familial convulsions (BFNC)
2- Defect in a neuronal K+ channel
Tonic clonic seizures
A tonic clonic seizure may be preceded by a partial seizure (aura) which can take many
forms. However, a history of such aura is commonly not obtained probably because the
subsequent generalized seizure causes some retrograde amnesia for immediately preceding
events.
The patient then goes rigid and becomes unconscious, falling down heavily if standing and
often sustaining injury. During this phase, respiration is arrested and central cyanosis may
occur. After a few moments the rigidity is periodically relaxed, producing clonic jerks. Some
patients don’t have clonic phase and the rigidity is replaced by a flaccid state of deep coma
which can persist for many minutes.
The patient then gradually regains consciousness, but is in a confused and disoriented state
for half an hour or more after regaining consciousness. Full memory functions may not be
recovered for some hours.
During the attack urinary incontinence and tongue biting may occur. A severe bitten
bleeding tongue after an attack of loss of consciousness is pathognomonic of a generalized
seizure. After generalized seizure the patient feels terrible, may have headache and often
wants to sleep.

5
Witnesses of a seizure are usually frightened by the event often believe the patient to be
dying and may not give a clear account of the episode. This in itself can be a helpful
diagnostic pointer since syncope seldom produce such fear in onlookers. Patients may have
no tonic or clonic phase and may not become cyanosed or bite their tongues.
However, postictal confusion is useful in differentiating seizures from syncope
Absence seizure
They always start in childhood. The attacks may be mistaken for complex partial seizures
but are shorter in duration, they occur much more frequently (20 – 30 times per day) and
are not associated with post-ictal confusion. They do not cause loss of posture.
Atonic seizures
Sudden loss of postural tone with a collapse to the ground (“drop attack). If more
restricted, can just involve nuchal and head muscles (head nod).
Can often be intermixed with other seizure types (atypical absence, myoclonic). Often
causes injury.
Tonic & Clonic fits
Tonic seizures are characterized by continuing muscle contraction that can lead to fixation
of the limbs and axial musculature in flexion or extension and are a cause of drop attacks;
the accompanying arrest of ventilatory movements leads to cyanosis. Consciousness is lost,
and there is no clonic phase to these seizures.
Clonic seizures are characterized by repetitive clonic jerking accompanied by loss of
consciousness. There is no initial tonic component.
Myoclonic epilepsy
Sudden, usually generalized, single body jerk, often throwing individual to the
ground.
Can affect single body part (in this case, not a generalized seizure).
Soo brief, cannot really know if consciousness is affected.
Can occur one after another repetitively or in clusters

6
Complex partial seizures
Involve episodes of altered consciousness without the patient collapsing to the ground,
especially if they arise from the temporal and less frequently the frontal lobes.
Patients stop what they are doing and stare blankly, often blinking repetitively , making
smacking movements of the lips, or displaying other automatisms, such as picking at their
clothes.
After a few minutes, consciousness returns but the patient may be muddled and feels
drowsy for a period of up to an hour.
Immediately before such an attack the patient may report alteration of mood, memory or
perception (such as undue familiarity- Déjà vu – or unreality – Jamais vu ) , or complex
hallucinations involving sound , smell , taste , vision , emotion (fear , sexual arousal ) or
visceral sensations (nausea , epigastric discomfort ).
If these changes of memory or perception occur without subsequent alteration in
awareness, the seizure is said to be simple partial seizure.
If these seizures arise from the anterior parts of the temporal lobes, they may produce
bizarre behavior patterns including limb posturing, sleep walking, or even ill –directed
motor activities with incoherent screaming.
These can sometimes be very difficult to distinguish from psychogenic attacks. However
abruptness of onset and relative brevity may help point to frontal seizures, as may a
tendency to occur out of sleep.
Partial motor seizures
Epileptic activity arising in the pre central gyrus causes partial motor seizures in the
contralateral face, arm, trunk or legs.
Seizures are characterized by rhythmical jerking or sustained spasm of the affected parts.
They may remain localized to one part or may spread to involve the whole side.
Some attacks begin in one part of the body (e.g. mouth, thumb, great toe) and spread
(march) gradually to other parts of the body; this is known as Jacksonian seizure.
Attacks vary in duration from a few seconds to several hours (epilepsia partialis continua).
More prolonged episodes may be followed by paresis of the involved limb lasting for
several hours after the seizure ceases (Todd palsy).
Partial sensory seizures
Seizures arising in the sensory cortex cause unpleasant tingling or electric sensations in the
contralateral face or limbs. Jacksonian march may also occur.
7
Investigations
After a first seizure, cerebral imaging with CT or MRI is advisable, particularly in patients
over 20 years of age, although the yield of structural lesions is low unless there are focal
features to the seizure or there are focal signs. Other investigations for infective, toxic and
metabolic causes may be appropriate.
An EEG performed immediately after a seizure may be more helpful in showing focal
features than if performed after a delay. An EEG is often useful when more than one
seizure has occurred, in order to establish the type of epilepsy and guide therapy.
Epileptic nature of attacks?
o Ambulatory EEG
o Videotelemetry
Type of epilepsy?
o Standard EEG
o Sleep EEG
o EEG with special electrodes (foramen ovale, subdural
(
Structural lesion?
o CT
o MRI
Metabolic disorder?
o Urea and electrolytes
o Liver function tests
o Blood glucose
o Serum calcium, magnesium
Inflammatory or infective disorder?

8
o Full blood count, erythrocyte sedimentation rate (ESR), C-reactive protein
(CRP)
o Chest X-ray
o Serology for syphilis, HIV, collagen disease
o CSF examination
The increasing sophistication of imaging techniques now allows the identification of the
cause of epilepsy in an increasing number of patients, especially those with partial seizures.
Investigations should be pursued more vigorously if the epilepsy is intractable to treatment.
The EEG may help to establish a diagnosis and characterize the type of epilepsy.
Interictal records are abnormal in about 50 % (sharp waves or spikes) of patients with
definite epilepsy so that the EEG cannot be reliably used to exclude epilepsy. However
epileptiform changes on the EEG are fairly specific for epilepsy (falsely positive in 1/1000).
The sensitivity can be increased to about 80 % prolonging recording time or including a
period of natural or drug-induced sleep.
Ambulatory EEG recording or video EEG monitoring may provide helpful information when
attacks are frequent.
Primary Generalized Epilepsy
Absence Seizure
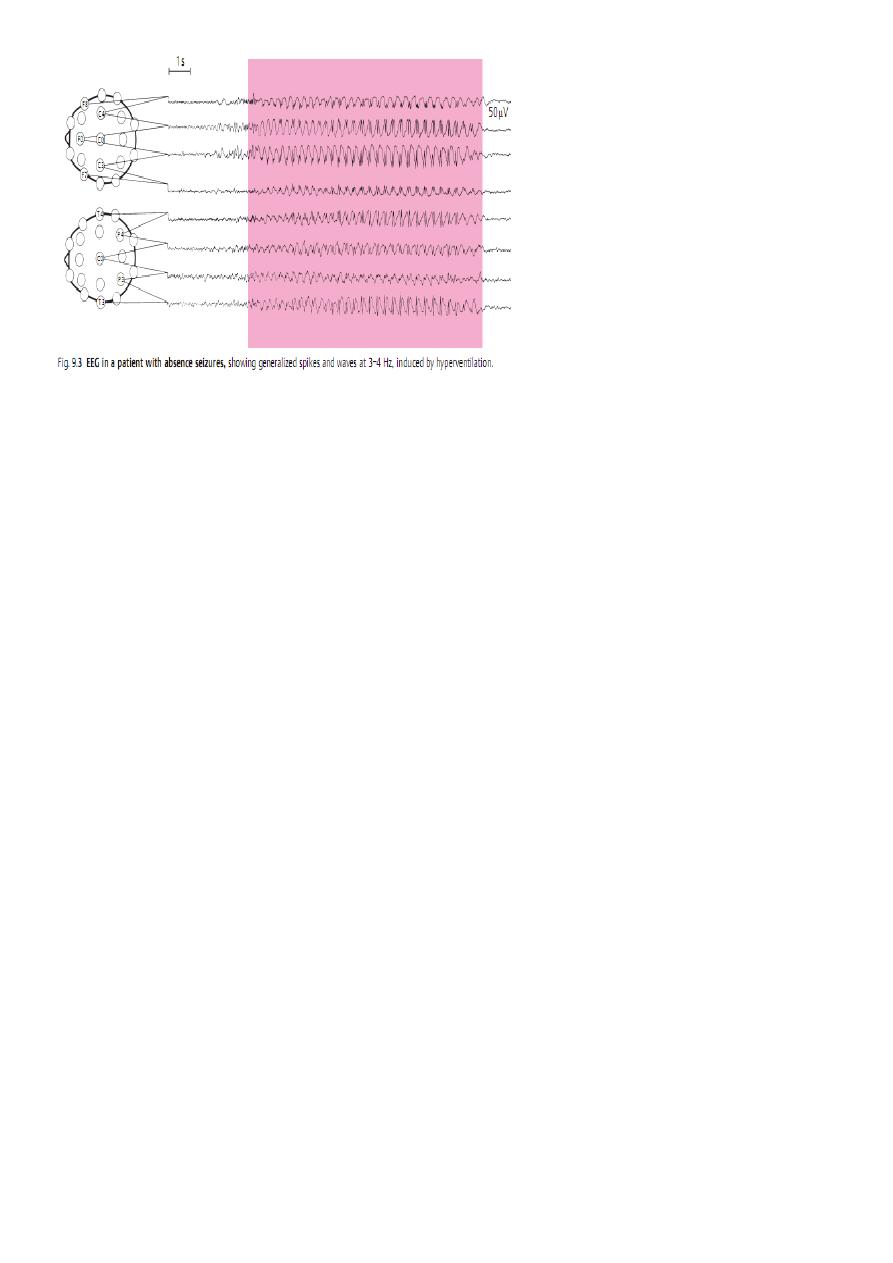
9
Indications for imaging
Epilepsy starts after the age of 20 years
Seizures have focal features clinically
EEG shows a focal seizure source
Control of seizures is difficult or deteriorates
Management
Explain the nature and cause of seizures to patients and their relatives.
Instruct relatives in the first aid management of major seizures.
Epilepsy is common-affects 0.5 – 1%of the population.
Good control of seizures is expected in 80 % of patients
First aid (by relatives and witnesses)
Move person away from danger (fire, water, machinery, furniture)
After convulsions cease, turn into 'recovery' position (semi-prone)
Ensure airway is clear
Do NOT insert anything in mouth (tongue-biting occurs at seizure onset and cannot
be prevented by observers)
If convulsions continue for more than 5 minutes or recur without person regaining
consciousness, summon urgent medical attention
Person may be drowsy and confused for some 30-60 minutes and should not be left
alone until fully recovered

11
Immediate management of seizures
Ensure airway is patent
Give oxygen to offset cerebral hypoxia
Give intravenous anticonvulsant (e.g. diazepam 10 mg) ONLY IF convulsions are
continuous or repeated (if so, manage as for status epilepticus)
Consider taking blood for anticonvulsant levels (if known epileptic)
Investigate cause
Lifestyle modification
Patients should be made aware of the riskiness of any activity where loss of awareness
would be dangerous, until good control of seizures has been established. This includes work
or recreational activities involving exposure to heights, dangerous machinery, open fires or
water. Only shallow baths or showers should be taken, and then with someone else in the
house and with the bathroom door unlocked. Cycling should be discouraged until at least 6
months' freedom from seizures has been achieved. Activities requiring prolonged proximity
to water (e.g. swimming, fishing or boating) should always be in the company of someone
who is aware of the risk of a seizure and able to rescue the patient if necessary. In the UK
and many other countries, legal restrictions regarding vehicle driving apply to patients with
epilepsy, defined as more than one seizure over the age of 5 years. The patient should
inform the licensing authorities about the onset of seizures. It is also wise for patients to
notify their motor insurance company. Certain occupations, such as airline pilot, are not
open to anyone who has ever had an epileptic seizure;
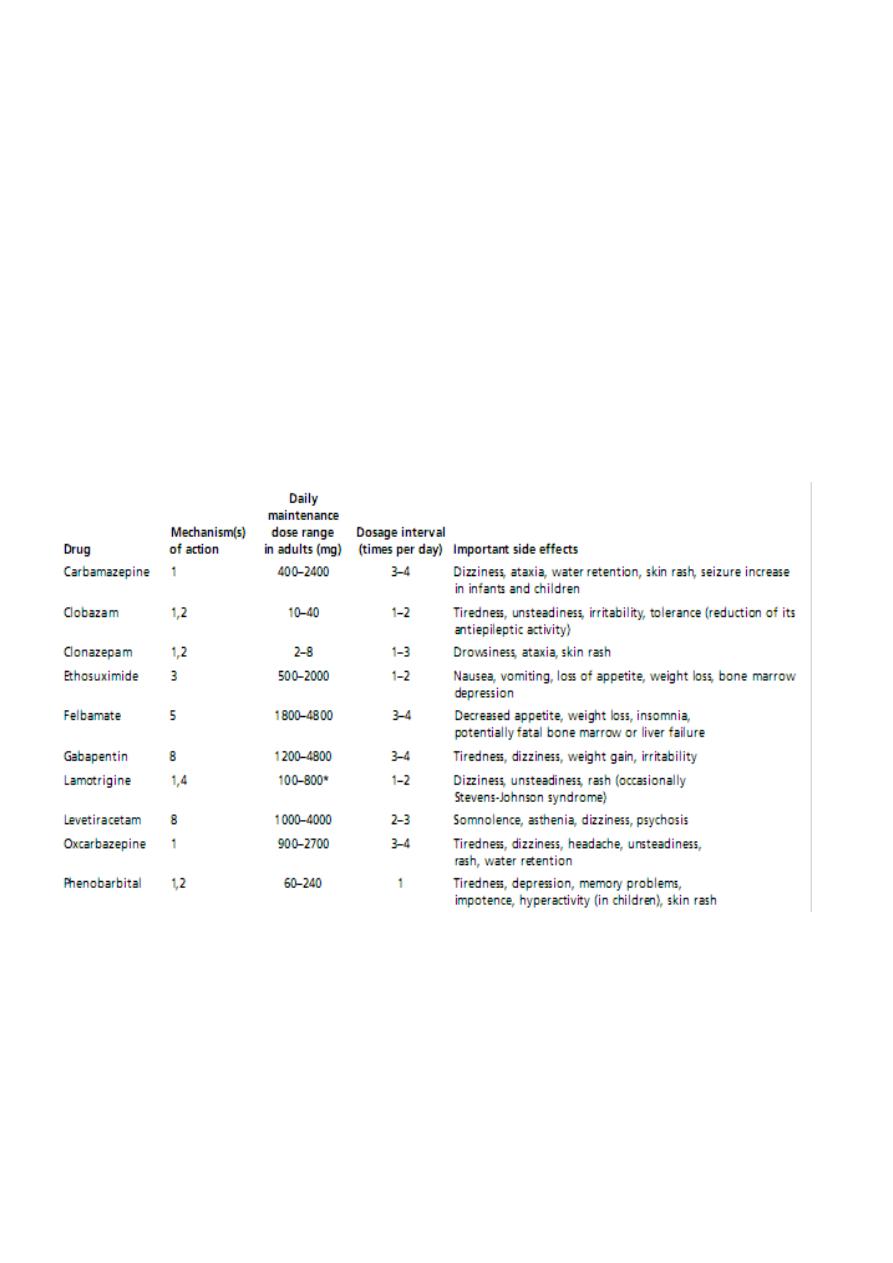
Anticonvulsant therapy
Drug treatment should certainly be considered after more than one seizure has occurred
and the patient agrees that seizure control is worthwhile; a wide range of anti-epilepsy
drugs is available.
The mode of action of these drugs is either to increase inhibitory neurotransmission in the
brain or to alter neuronal sodium channels in a way to prevent abnormally rapid
transmission of impulses.
In 80 % of patients whose epilepsy is controlled, only a single drug is necessary. The
combination of more than 2 drugs is seldom required. Dose regimens should be kept as
simple as possible to promote compliance.
11
With few exceptions, there is no hard evidence indicating that one drug is superior to
another.
The first choice should be one of the first line drug with the more recently introduced drugs
as second choice.
Phenytoin and carbamazepine are not ideal for a young woman wishing to use oral
contraceptives (inducer drugs).
Carbamazepine, lamotrigene and sodium valproate are preferable to phenytoin because of
the side effect profile of the latter and its complicated pharmacokinetics.
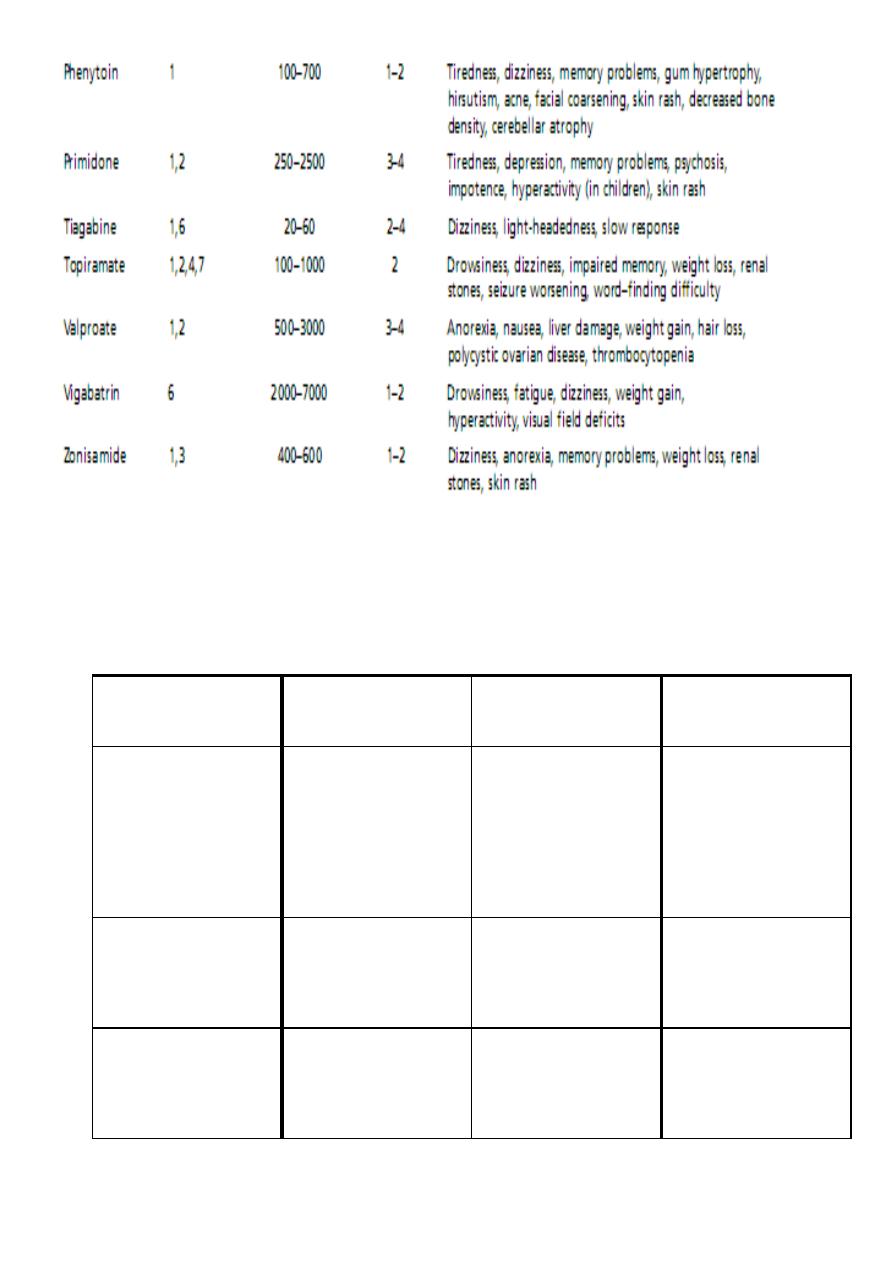
Important Pharmaco-Kinetic features of first and second line of AED
12
Guidelines for choice of AEDs
Third line
Second line
First-line drug
Epilepsy type
Lamotrigine
Sodium valproate
Levetiracetam
topiramate
carbamazepine
Partial
and/or
secondary GTCS
Lamotrigine
topiramate
Sodium valproate
Primary GTCS
Sodium valproate
ethosuximide
absence

13
clonazepam
Sodium valproate
myoclonic
Guidelines for anticonvulsant therapy
Start with one first-line drug.
Start at a low dose, increase, dose until effective control of seizures is achieved or
side effects develop (drug level may be helpful).
Optimize compliance (use minimum number of doses per day).
If first drug fails, start second first-line drug while gradually withdrawing first.
If second drug fails, start second-line drug in combination of preferred first-line drug
at maximum tolerated dose (beware of interaction)
If this combination fails replace second-line drug with alternative second-line drug.
If this combination fails, check compliance and reconsider diagnosis (is there an
occult structural or metabolic lesion or are seizures truly epileptic?).
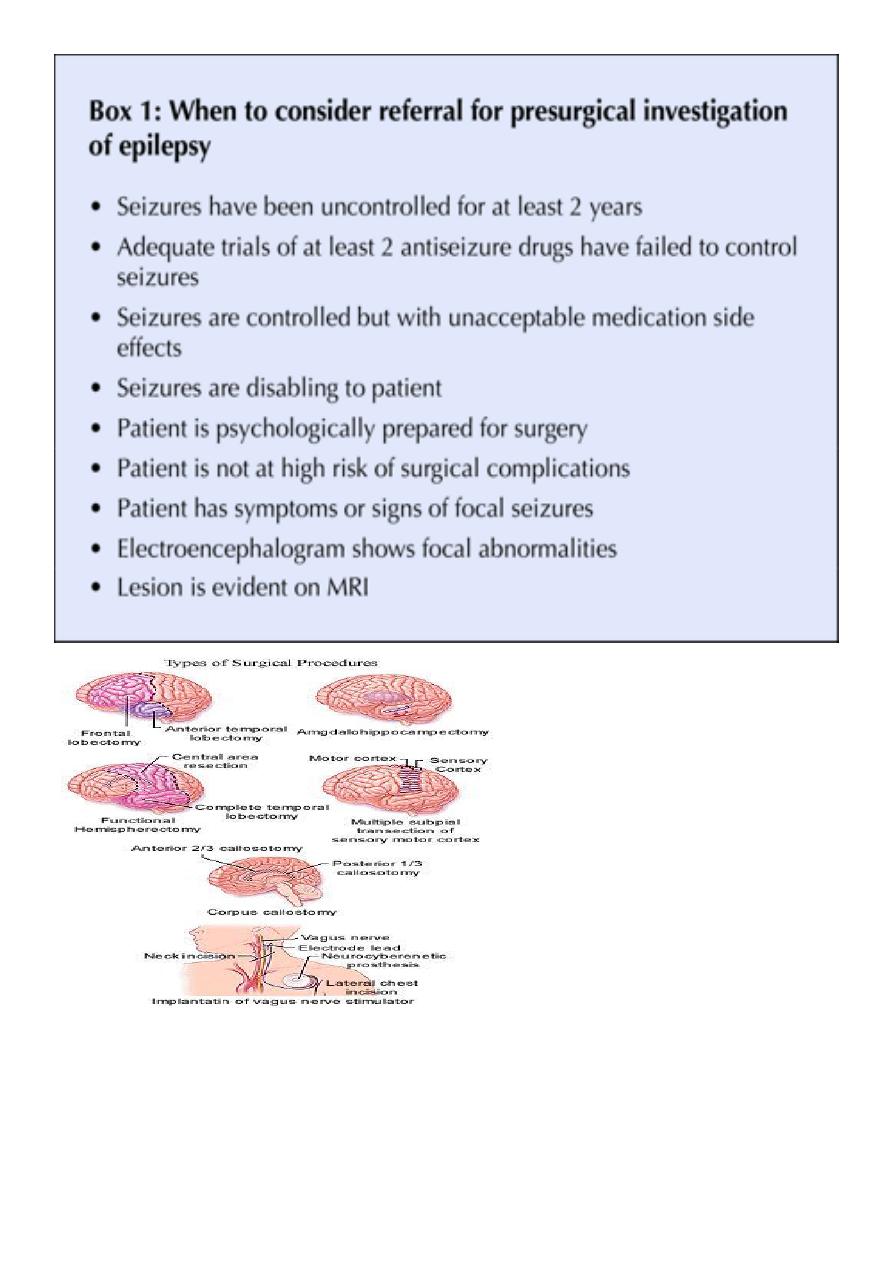
If this combination fails consider alternative non-pharmacological treatment (surgery
or VNS).
Do not use more than 2 drugs in combination at any one time.
Monitoring therapy
With some drugs such as phenytoin and carbamazepine, occasional measurement of the
blood level can be a guide whether the patient is on an appropriate dose and is complying
with the medication, but blood levels need to be interpreted carefully.
The dose of AED in an individual patient should primarily be governed by the efficacy of
seizure control and the development of side effects rather than blood levels alone.
With sodium valproate, there is a poor relationship between blood level and anticonvulsant
efficacy and so levels are only useful to assess compliance.
Repeated measurement of blood levels is not generally useful and monitoring is of most
value in dealing with suspected toxicity, the pharmacokinetic effect of pregnancy or in
suspected non-compliance.
Withdrawing AEDs
After complete control of seizures for 2 – 4 years, withdrawal of medication may be
considered.
Childhood – onset epilepsy particularly classical absence seizures carries the best prognosis.
14
Juvenile myoclonic epilepsy have a marked liability to recur after drug withdrawal.
Seizures that begin in adult life particularly those with partial features are likely to recur
especially if there is a structural lesion.
Overall, the overall recurrence rate is about 40 %.
The EEG is generally a poor predictor of recurrence but if the record is still very abnormal,
drug withdrawal is unwise.
Withdrawal should be undertaken slowly, reducing the drug dose gradually over 6-12
months.
VNS Therapy (Vagus Nerve Stimulation)
VNS Therapy consists of electrical signals that are applied to the vagus nerve in the neck for
transmission to the brain.
The vagus nerve has proven to be a good way to communicate with the brain because:
1- There are few if any pain fibers in the vagus nerve.
2- Over 80% of the electrical signals applied to the vagus nerve in the neck are sent
upwards to the brain.
3- The surgical procedure to attach the lead to the vagus nerve does not involve the
brain. It is not brain surgery.
The Ketogenic Diet
Very high in fat and low in carbohydrates and protein.
4 grams of fat for each gram of protein and carbohydrate consumed.
Caloric intake is usually 75% of the recommended calorie intake
A minimum of 1 gram of protein per kilogram of body weight per day is provided.
Restricting fluid to 65 mL per kilogram of body weight per day
15
Contraception
Many AEDs, including carbamazepine, phenytoin, barbiturate, induce hepatic enzymes,
accelerate metabolism of estrogen and cause breakthrough bleeding and contraceptive
failure.
Lamotrigine and oxcarbazepine have little interaction.

16
Sodium valproate has no interaction with oral contraceptives.
The safest policy is to use an alternative contraceptive method, but it is sometimes possible
to overcome the problem by giving higher dose of estrogen.
Pregnancy
With the exception of gabapentine, all AEDs is associated with fetal abnormalities such as
cleft lip, spina bifida and cardiac defects.
The risk is greatest when treatment is given in the 1
st
trimester, rising from a background
risk of 2-4% to about 4-8% with one drug and to 15 % with two drugs or more.
Folic acid (5 mg daily) taken 2 months before conception may reduce the risk of some fetal
abnormalities
Seizures often become more frequent during pregnancy, especially during the 3
rd
trimester
when plasma anticonvulsant level tend to fall.
Monitoring of blood levels of anticonvulsants can be helpful with adjustment of drug doses.
Occasionally in a well-controlled patient, AEDs can be withdrawn before conception, but if
major seizures have occurred in the preceding year, this is unwise, since uncontrolled
maternal seizures represent a significant risk to the fetus.
Prognosis
Overall, generalized seizures are more readily controlled than partial seizures.
The presence of structural lesion makes complete control of the epilepsy less likely.
There is a 40 fold increased risk of sudden unexplained death in epilepsy (SUDEP) and
patients may need to be made aware of this in order to help them rearrange their
lifestyle and comply with treatment.
Epilepsy outcome after 20 years
50 % are seizure free, without drugs, for last 5 years.
20 % are seizure free for last 5 years but continue to take medication.
30 %continue to have seizures in spite of AEDs.
Status epilepticus
Defined a seizure or a series of seizures lasting 30 minutes without the patient regaining
awareness between attacks. Most commonly, this refers to recurrent tonic clonic seizures
(major status) and is a life-threatening medical emergency. Partial motor status is obvious
clinically, but complex partial status and absence status may be difficult to diagnose
because the patient may merely present in a dazed, confused state. Status is never the

17
presenting feature of idiopathic epilepsy but may be precipitated by abrupt withdrawal of
anticonvulsant drugs, the presence of a major structural lesion or acute metabolic
disturbance, and tends to be more common with frontal epileptic foci .It should be
remembered that psychogenic or non-epileptic attacks commonly masquerade as 'status
epilepticus', so electrophysiological confirmation of the seizures should be obtained as early
as possible
Management of status epilepticus
Initial:
Ensure airway is patent, give oxygen to prevent cerebral hypoxia and secure intravenous
access. Draw blood for glucose, urea and electrolytes (including Ca and Mg), and liver
function and store a sample for future analysis (e.g. drug misuse). Give diazepam 10 mg i.v.
or rectally or lorazepam 4 mg i.v. –repeat once only after 15 minutes.
Transfer to intensive care area, monitor neurological condition, blood pressure, and
respiration and blood gases. Intubating and ventilating patient if appropriate.
If seizure continue after 30 minutes
Intravenous infusion (with cardiac monitoring) with one of:
1- Phenytoin: i.v. infusion of 15 mg/kg at 50 mg/min
2- Fosphenytoin: i.v. infusion of 15 mg/kg at 100 mg/min
3- Phenobarbital: i.v. infusion of 10 mg/kg at 100 mg/min
If seizures still continue after 30-60 mins
Start treatment for refractory status with intubation and ventilation, and general
anesthesia using propofol or thiopental
Once status controlled
Commence longer-term anticonvulsant medication with one of :
1- Sodium valproate 10 mg/kg i.v. over 3-5 mins, then 800-2000 mg/day
2- Phenytoin: give loading dose (if not already used as above) of 15 mg/kg, infuse at <
50 mg/min, then 300 mg/day
3- Carbamazepine 400 mg by nasogastric tube, then 400-1200 mg/day.
Investigate cause.
Non-epileptic attack disorder ('psychogenic attacks', 'pseudo-seizures’)
Patients may present with attacks that superficially resemble epileptic seizures but which
are caused by psychological phenomena and not associated with abnormal epileptic
discharges in the brain. Such patients may present in apparent status epilepticus. People
with epilepsy may have non-epileptic attacks as well, and this diagnosis should be
considered if a patient fails to respond to anti-epileptic therapy, especially in the absence of
18
a structural abnormality. Non-epileptic attacks may be quite difficult to distinguish from
truly epileptic attacks. Clues pointing towards non-epileptic attacks include elaborate
arching of the back in an attack, pelvic thrusting and/or wild flailing of limbs. Cyanosis and
severe biting of the tongue are rare in non-epileptic attacks, but urinary incontinence can
occur. The distinction between epileptic attacks originating in the frontal lobes and non-
epileptic attacks may be especially difficult, and may require video telemetry with
prolonged EEG recordings. Non-epileptic attacks are three times more common in women
than in men and have been associated with a history of sexual abuse in childhood. They are
not necessarily associated with formal psychiatric illness. Treatment is often difficult and
usually requires psychotherapy and/or counselling rather than drug therapy.
Differential Diagnosis of Seizures
Features That Distinguish Generalized Tonic-Clonic Seizure from Syncope
Syncope
Seizure
Features
Emotional stress, Valsalva,
orthostatic
hypotension,
Usually none
Immediate
precipitating
factors
• Syncope
• Vasovagal syncope
• Cardiac arrhythmia
• Valvular heart disease
• Cardiac failure
• Orthostatic hypotension
• Psychological disorders
• Psychogenic seizure
• Hyperventilation
• Panic attack
• Metabolic disturbances
• Alcoholic blackouts
• Delirium tremens
• Hypoglycemia
• Hypoxia
• Psychoactive drugs (e.g.,
• hallucinogens)
• Migraine
• Confusional migraine
• Basilar migraine
• Transient ischemic attack (TIA)
• Basilar artery TIA
• Sleep disorders
• Narcolepsy/cataplexy
• Benign sleep myoclonus
• Movement disorders
• Tics
• Nonepileptic myoclonus
• Paroxysmal choreoathetosis
• Special considerations in children
• Breath-holding spells
• Migraine with recurrent
• abdominal pain and cyclic
• vomiting
• Benign paroxysmal vertigo
• Apnea
• Night terrors
• Sleepwalking
19
cardiac etiologies
Tiredness,
nausea,
diaphoresis, tunneling of
vision
None or aura (e.g., odd
odor)
Premonitorysy mptoms
Usually erect
Variable
Posture at onset
Gradual over seconds
Often immediate
Transition
to
unconsciousness
Seconds
Minutes
Duration
of
unconsciousness
Never more than 15 s
30–60 s
Duration of tonic or clonic
movements
Syncope
Seizure
Features
Pallor
Cyanosis, frothing at mouth
Facial appearance during
event
5 min
Many minutes to hours
Disorientation
and
sleepiness after event
Sometimes
Often
Aching of muscles after
event
Rarely
Sometimes
Biting of tongue
Sometimes
Sometimes
Incontinence
Rarely
Sometimes
Headache
