CHRONIC DIARRHEA
Supervised By: Dr. Ismael Dawood
Presented By: Fadi Adel
Basma Ahmed
Saja Laith
Haneen Laith
Diarrhea
•
Normal bowel movement frequency ranges from three times
daily to once every 3 days.
•
Diarrhoea
is the frequent passage of loose stools.
•
It is also defined as the passage of more than
200 g
of stool
daily
, and measurement of stool volume is helpful in confirming
this.
•
Chronic Diarrhea
lasts more than
four weeks.
•
The
most severe symptom
in many patients is
urgency
of
defecation
, and
faecal incontinence
is a common event in
acute and chronic diarrheal ilness.
•
High-volume diarrhoea
(>1 litre per day) occurs when stool
water content is increased (the principal site of water
absorption being the colon) and may be:
Secretory
(persists when the patient fasts), due to intestinal
inflammation, e.g. infection, or inflammatory bowel disease.
Osmotic
(stops when the patient fasts), due to malabsorption,
adverse drug effects or motility disorders.
•
Steatorrhoea
is diarrhoea associated with fat malabsorption.
The stools are greasy, pale and bulky, and float, making them
difficult to flush away.
•
Low-volume diarrhoea
is associated with the irritable
bowel syndrome
Chronic or Relapsing Diarrhoea
•
The most common cause is
irritable bowel syndrome
.
•
Chronic diarrhoea can be categorised as being due to
disease of the
colon
or
small bowel
, or to
malabsorption.
•
Clinical presentation, examination of the stool, routine
blood tests and imaging reveal a diagnosis in many
cases. A series of negative investigations usually implies
irritable bowel syndrome but some patients clearly have
organic disease and need more extensive investigations.
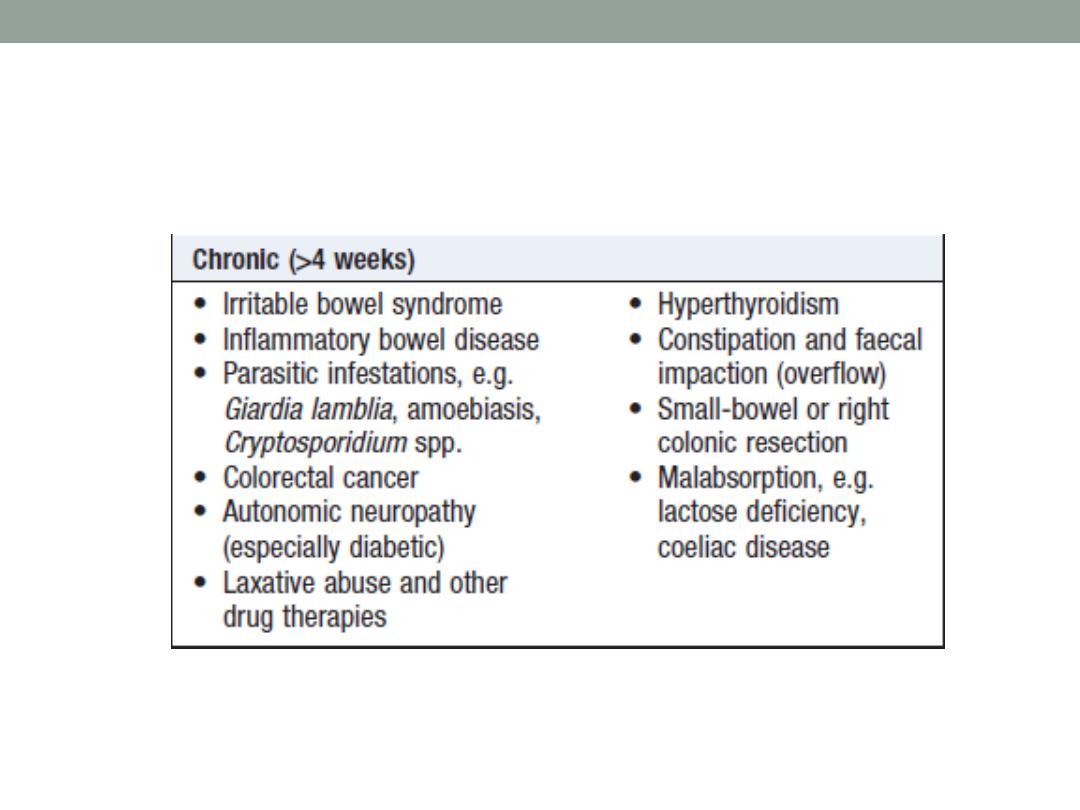
Causes
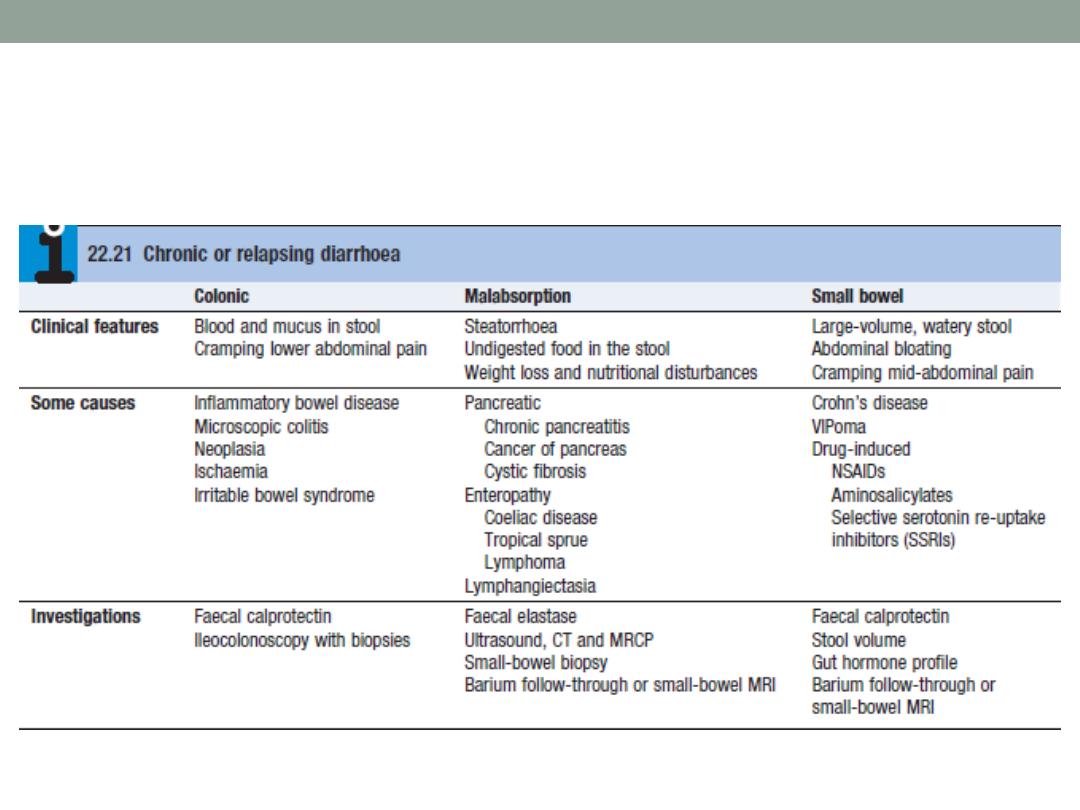
Clinical Features and Investigation
Red Flags - suggestive of organic causes
•
Painless Diarrhea.
•
Recent onset in an older patient .
•
Nocturnal diarrhea (especially if awakes the patient).
•
Weight loss.
•
Blood in stool.
•
Large stool volumes: >400 grams stool per day
•
Anemia.
•
Hypoalbuminemia.
•
increased ESR.
Irritable Bowel Syndrome
•
IBS is the most common cause of gastrointestinal referral
and accounts for frequent absenteeism from work and
impaired quality of life.
•
Young women are affected 2
–3 times more often than
men.
•
Coexisting conditions, such as non-ulcer dyspepsia,
chronic fatigue syndrome, dysmenorrhoea and
fibromyalgia, are common.

Clinical Features
•
The most common presentation
is
recurrent abdominal
discomfort
. this is usually
colicky or cramping
in nature,
felt in the
lower abdomen
and
relieved by defecation
.
Abdominal bloating
worsens throughout the day.
•
The bowel habit is variable
, most patients
alternate
between episodes of diarrhea and constipation.
•
Those with constipation tend to pass infrequent pellety
stools, usually in association with abdominal pain or
proctalgia.
•
Those with diarrhoea have
frequent defecation
but
produce
low-volume stools
and
rarely
have nocturnal
symptoms. Passage of mucus is common but
rectal
bleeding
does
not occur
. Patients do not lose weight and
are constitutionally well.
•
Physical examination
is generally unremarkable, with the
exception of variable tenderness to palpation.
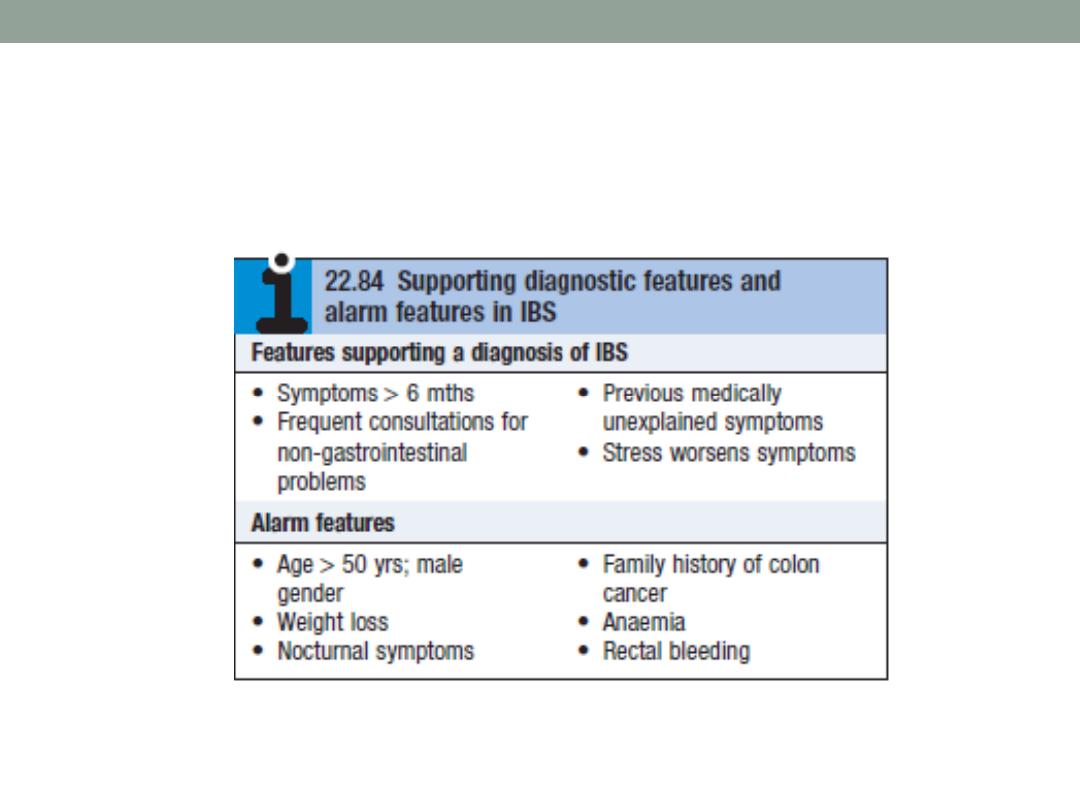
Diagnosis
•
The diagnosis is
clinical
and can be made confidently in
most patients using the Rome criteria combined with the
absence of alarm symptoms, without resorting to
complicated tests.
•
Those
who present atypically
require investigations to
exclude other gastrointestinal diseases.
•
Diarrhea predominant patients
justify investigations to
exclude coeliac disease , microscopic colitis ,lactose
intolerance , bile acid malabsorption, thyrotoxicosis and,
in developing countries parasitic infection.
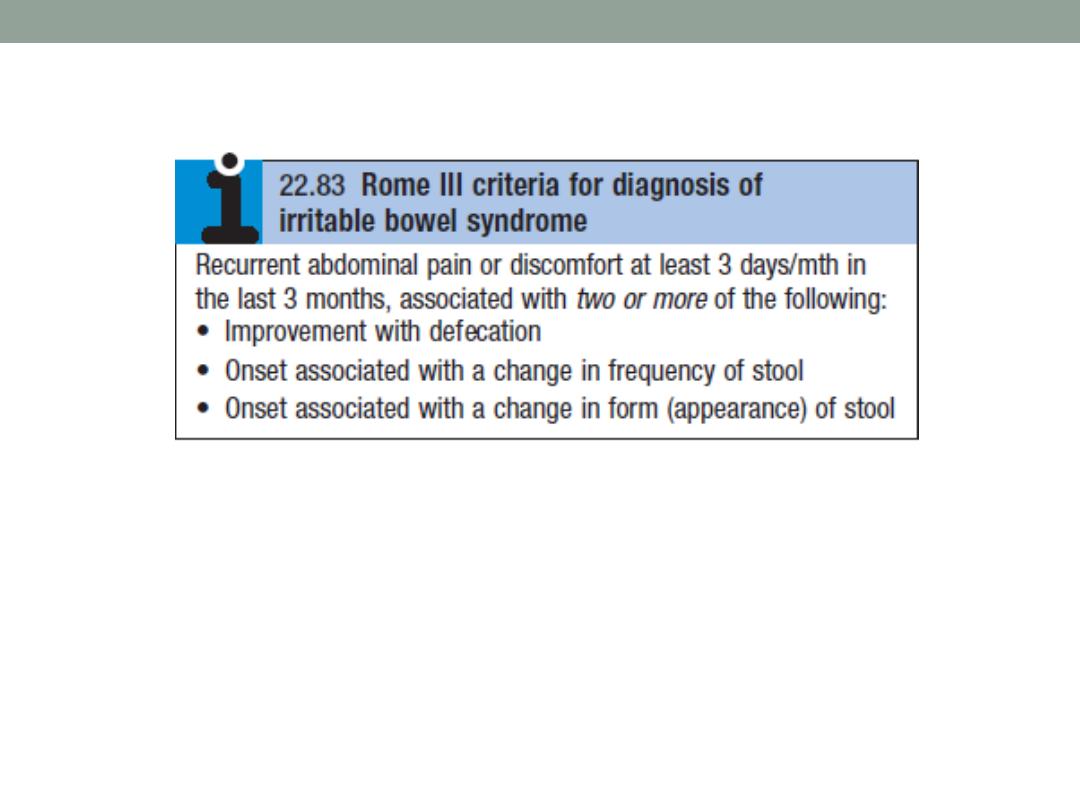
Criterion fulfilled for the last 3 months with symptom onset at
least 6 months prior to diagnosis.
“Discomfort” means an uncomfortable sensation not
described as pain.
Rome IV Criteria for Diagnosing IBS
•
Recurrent abdominal pain, on average, at least 1
day/week in the last 3 months, associated with two or
more of the following criteria:
•
Related to defecation
•
Associated with a change in frequency of stool
•
Associated with a change in form (appearance) of stool.
•
Criteria fulfilled for the last 3 months with symptom onset
at least 6 months before diagnosis.
Management
•
The most important steps are to
make a positive
diagnosis
and
reassure
the patient.
•
Many patients are concerned that they have developed
cancer, and a cycle of anxiety leading to colonic
symptoms, which further heighten anxiety, can be broken
by
explanation
that symptoms are not due to a serious
underlying disease but instead are the result of
behavioural, psychosocial, physiological and luminal
factors.
Inflammatory Bowel Disease
•
Ulcerative colitis and
Crohn’s disease
are chronic
inflammatory bowel diseases
which have a protracted
relapsing and remitting course
, usually
extending over
years.
•
Both diseases most commonly
start in the second and
third decades of life
, with a second smaller incidence
peak in the
seventh decade
.
•
Life expectancy
in patients with IBD is
similar
to that of the
general population.
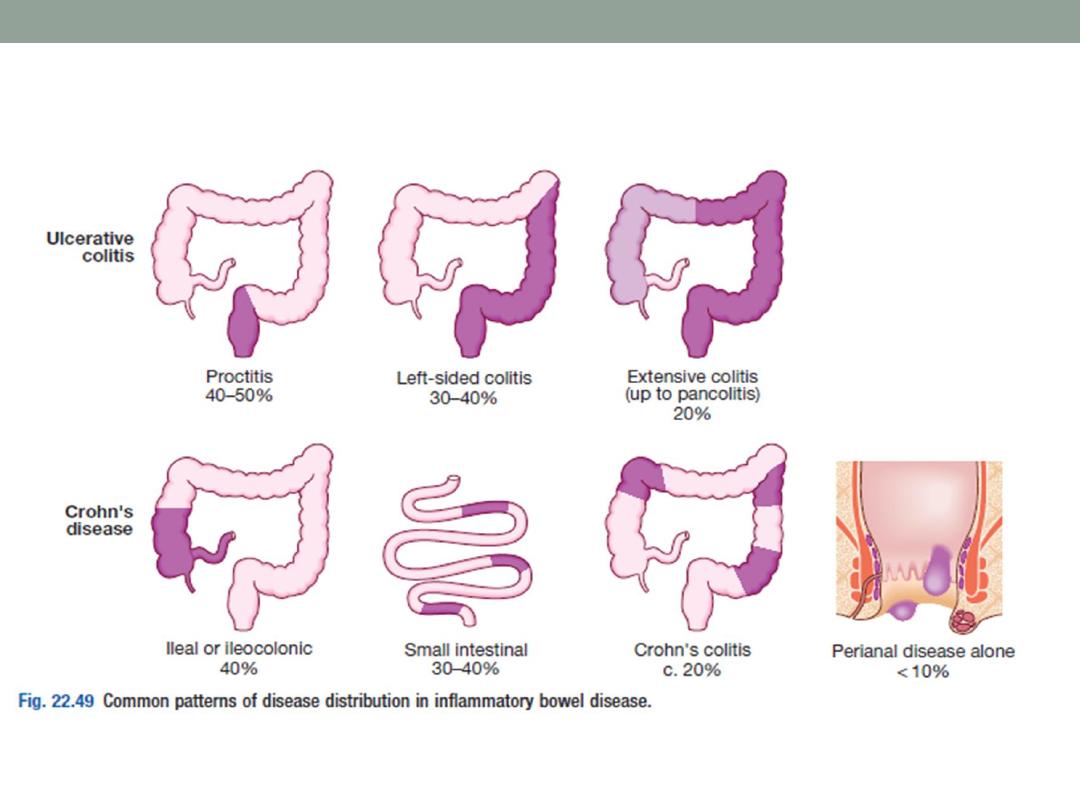
Clinical Features of Ulcerative Colitis
•
The cardinal symptoms are
rectal bleeding with passage
of mucus and bloody diarrhoea
. The presentation varies,
depending on the site and severity of the disease, as well
as the presence of extra-intestinal manifestations.
•
The first attack
is usually the most severe and is followed
by
relapses and remissions
.
•
Emotional stress, intercurrent infection, gastroenteritis,
antibiotics or NSAID therapy may all provoke a relapse.
•
Proctitis
causes rectal bleeding and mucus discharge,
accompanied by
tenesmus
. Some patients pass frequent,
small volume fluid stools, while others pass pellety stools.
Constitutional symptoms
do
not
occur.
•
Left-sided and extensive colitis
causes bloody diarrhoea
with mucus, often with abdominal cramps.
In severe
cases
, anorexia, malaise, weight loss and abdominal pain
occur, and the patient is
toxic
, with fever, tachycardia and
signs of peritoneal inflammation.
Clinical Features of
Crohn’s Disease
•
The major symptoms
are abdominal pain, diarrhoea and
weight loss. Ileal
Crohn’s disease may cause subacute or
even acute intestinal obstruction.
•
The pain is often associated with
diarrhoea
, which is
usually watery and does not contain blood or mucus.
•
Almost all patients lose weight
because they avoid food,
since eating provokes pain. Weight loss may also be due
to malabsorption.
•
Crohn’s colitis
presents in an identical manner to
ulcerative colitis, but
rectal sparing
and the presence of
perianal disease
are features which
favour a diagnosis of
Crohn’s disease.
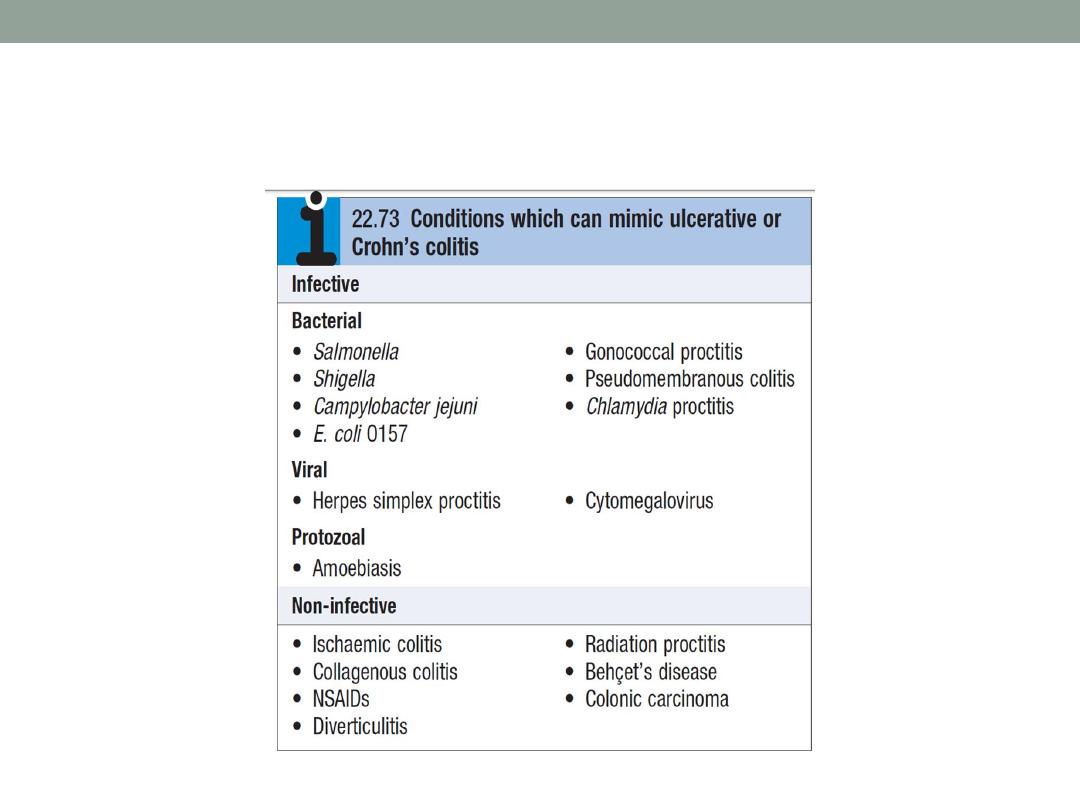
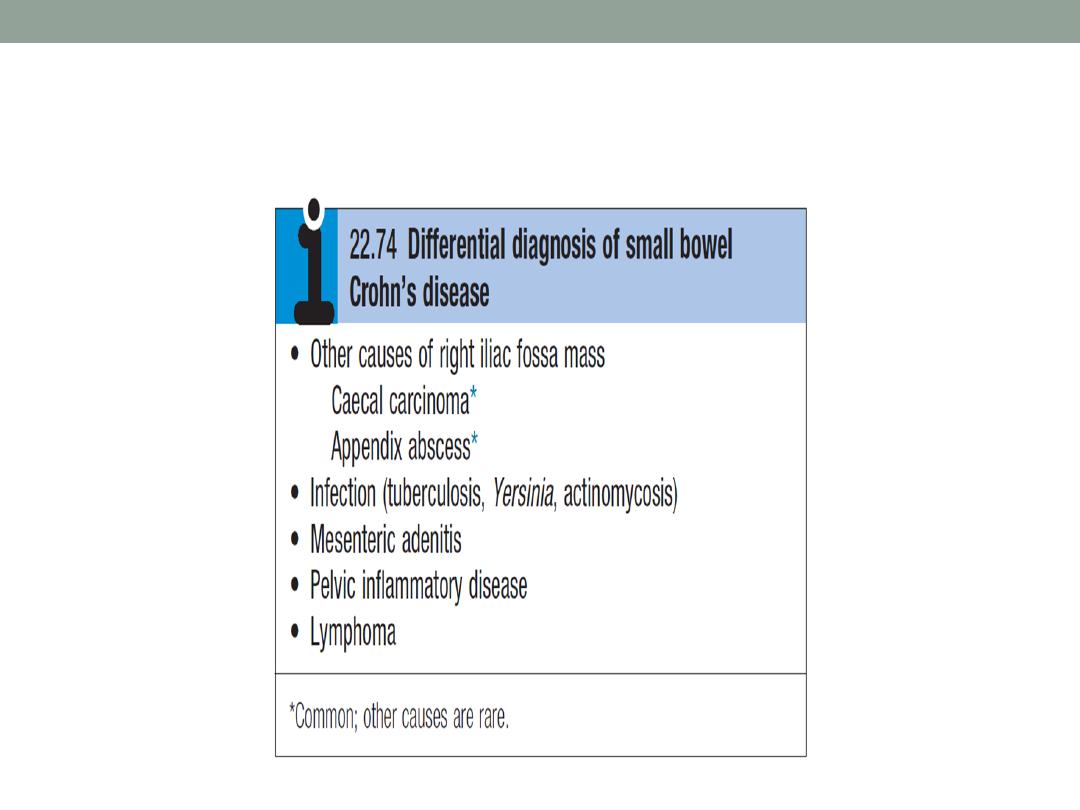
Differential Diagnosis
Investigations
•
Investigations are necessary to confirm the diagnosis, define
disease distribution and activity, and identify complications.
•
Full blood count
may show anaemia resulting from bleeding or
malabsorption of iron, folic acid or vitamin B12.
•
Serum albumin concentration
falls as a consequence of
protein-losing enteropathy, inflammatory disease or poor
nutrition.
•
The ESR and CRP
are elevated in exacerbations and in
response to abscess formation.

•
Faecal calproctectin
has a high sensitivity for detecting
gastrointestinal inflammation and may be elevated, even
when the CRP is normal. It is particularly useful in
distinguishing inflammatory bowel disease from irritable
bowel syndrome at diagnosis, and for subsequent
monitoring of disease activity.
•
Bacteriology:
stool microscopy, culture and examination
for Clostridium difficile toxin or for ova and cysts, blood
cultures and serological tests should be performed.

Endoscopy
•
Patients who present with diarrhoea plus raised inflammatory
markers or alarm features, such as weight loss, rectal bleeding
and anaemia, should undergo
ileocolonoscopy
.
•
Flexible sigmoidoscopy
is occasionally performed to make a
diagnosis, especially during acute severe presentations when
ileocolonoscopy may confer an unacceptable risk.
•
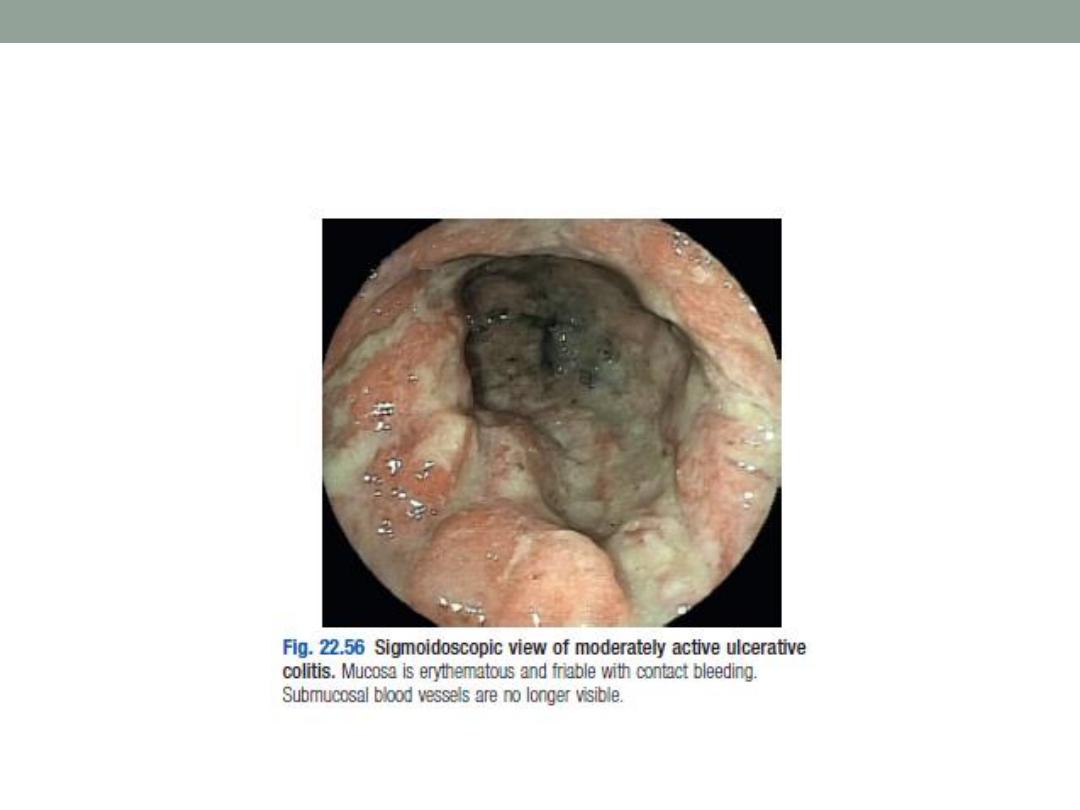
In ulcerative colitis
, there is loss of vascular pattern, granularity,
friability and contact bleeding, with or without ulceration.
•
In
Crohn’s disease
, patchy inflammation, with discrete, deep
ulcers, strictures and perianal disease (fissures, fistulae and
skin tags), is typically observed, often with rectal sparing.
Radiology
•
Barium enema is a less sensitive investigation than
colonoscopy in patients with colitis and, where
colonoscopy is incomplete, a CT colonogram is preferred.
•
Small bowel imaging is essential to complete staging of
Crohn’s disease. Traditional contrast imaging by barium
follow-through demonstrates affected areas of the bowel
as narrowed and ulcerated, often with multiple strictures.
•
A plain abdominal X-ray is essential in the management of
patients who present with severe active disease.
Dilatation of the colon , mucosal edema (thumb-printing)
or evidence of perforation may be found.
Clostridium Difficile Colitis
•
C. difficile is the most commonly diagnosed cause of
antibiotic-associated diarrhoea and is an occasional
constituent of the normal intestinal flora.
•
C. difficile is capable of producing two toxins (A and B).
•
C. difficile infection (CDI) usually follows antimicrobial
•
therapy, which alters the composition of the
gastrointestinal flora and may result in colonisation with C.
difficile.

Clinical Features
•
Disease manifestations range from diarrhoea to
lifethreatening pseudomembranous colitis.
•
Around 80% of cases occur in people over 65 years of
age, many of whom are frail with comorbid diseases.
•
Symptoms usually begin in the first week of antibiotic
therapy but can occur at any time up to 6 weeks after
treatment has finished.

•
The onset is often insidious, with lower abdominal pain
and diarrhoea which may become profuse and watery.
•
The presentation may resemble acute ulcerative colitis
with bloody diarrhoea, fever and even toxic dilatation and
perforation.
•
Ileus is also seen in pseudomembranous colitis.
Investigation
•
The diagnosis of CDI rests on detection of toxins A or B in the
stool.
•
screen stool from patients with a compatible clinical syndrome
by detection either of glutamate dehydrogenase (GDH), an
enzyme produced by C. difficile, or of C. difficile nucleic acid
(e.g. by PCR);
•
if screening is positive, a C. difficile toxin ELISA or a tissue
culture cytotoxicity assay is performed.
•
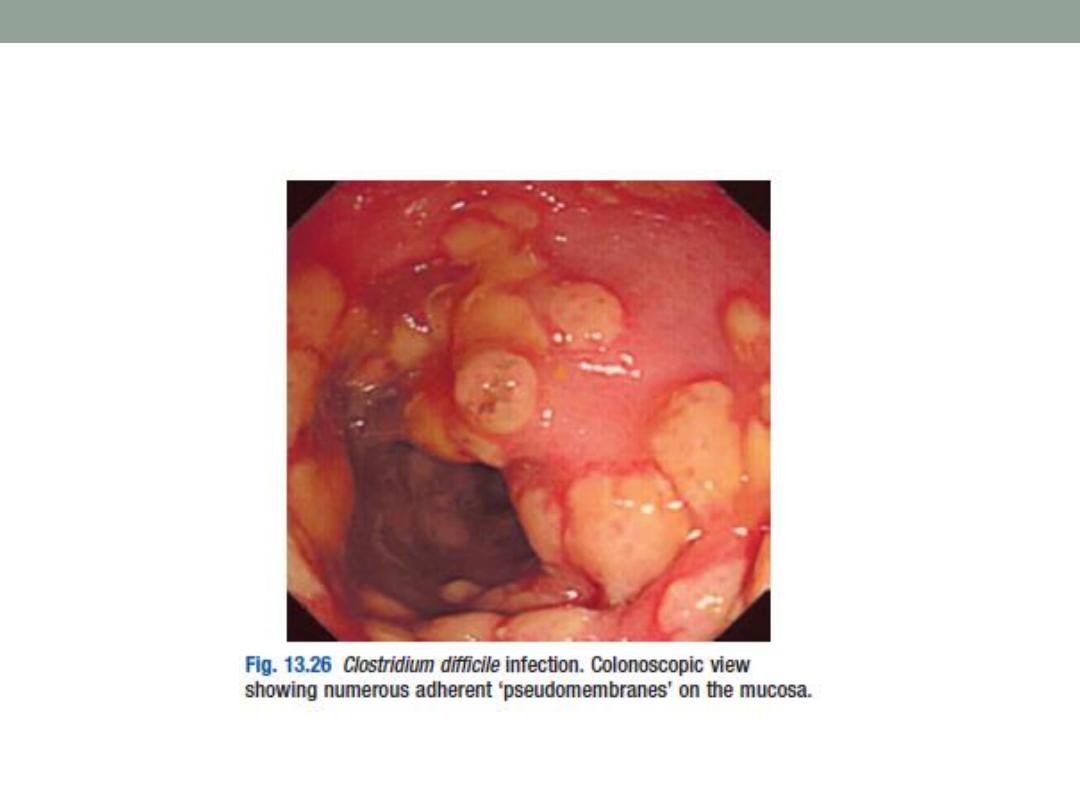
The rectal appearances at sigmoidoscopy may be
characteristic, with erythema, white plaques or an adherent
pseudomembrane.

Ischemic Colitis
•
The spectrum of injury of acute colonic ischemia ranges
from reversible colopathy to transient colitis, colonic
stricture, gangrene and fulminant pancolitis.
•
Arterial thromboembolism is usually responsible but
colonic ischaemia can also follow severe hypotension,
colonic volvulus, strangulated hernia, systemic vasculitis
or hypercoagulable states.
•
Ischaemia of the descending and sigmoid colon is also a
complication of abdominal aortic aneurysm surgery
(where the inferior mesenteric artery is ligated).
Presentation
•
patient is usually elderly and presents with sudden onset
of cramping, left-sided, lower abdominal pain and rectal
bleeding.
•
Symptoms usually resolve spontaneously over 24
–48
hours and healing occurs in 2 weeks.
•
Some may develop a fibrous stricture or segment of
colitis.
•
A minority develop gangrene and peritonitis.
Diagnosis and Management
•
The diagnosis is established by colonoscopy within 48
hours of presentation; otherwise, mucosal ulceration may
have resolved.
•
Except in the most severe cases, ischemic colitis is
treated with supportive care. IV fluids are given to treat
dehydration, and the patient is placed on bowel rest
(meaning nothing to eat or drink) until the symptoms
resolve.
•
Antibiotics are sometimes given in moderate to severe
cases;
•
About 20% of patients with acute ischemic colitis may
develop a long-term complication known as
chronic
ischemic colitis
.
•
Symptoms can include
recurrent infections, bloody
diarrhea, weight loss, and chronic abdominal pain.
Chronic ischemic colitis is often treated with surgical
removal of the chronically diseased portion of the bowel.
