Epilepsy
•
Epilepsy is one of the most common and disabling public health problems,
affecting approximately 50 million people around the world.
Definition
Seizures
are sudden but transient behavioral, somatosensory,
motor, or visual symptom or sign, and caused by
abnormal excessive cortical neuronal activity.
•
Cc
•
In 2014, the International League Against Epilepsy (ILAE) adopted a new practical
definition for epilepsy as a disease with either:
Epilepsy
recurrent unprovoked seizures (ie, two or more unprovoked seizures occurring at least 24
hours apart)
heightened tendency toward recurrent unprovoked seizures (ie, a single seizure,
accompanied by evidence from clinical, electroencephalographic, or neuroimaging
tests that a heightened risk [at least 60%] exists for future seizures over the next 10 years)
Classification
•
According to etiology
•
unprovoked
provoked
Seizures may occur spontaneously without provocation
or may be provoked by certain influences (eg, trauma,
brain tumors, stroke, CNS infection, metabolic
dyscrasias, or drug exposures).
•
According to semiology of the seizure
Partial (focal) seizures
simple partial
These may have motor features,
sensory symptoms or autonomic like
pallor, nausea, fear or anger.
The consciousness is
not impaired
•
Theses are originated from:
•
Consist of 3 distinct events
complex partial
There is transient impairment of the patient ability to maintain normal contact
with external environment.
characterized by motor and speech arrest, during
which the patient appears vacant (the ‘motionless stare’).
Automatisms are defined as involuntary motor actions that occur during or in the
aftermath of epileptic seizures, in a state of impaired awareness. Chewing, lip
smacking, swallowing, picking. Ambulatory as walking or running. Verbal as
words, sentences.
The aura is in effect a simple partial seizure. It is usually short-lived, lasting a few
seconds or so depending on site of origin.
Temporal lobe 60%
Frontal lobe 30%
Other sites 10%
aura
Impaired
consciousness
automatism
Generalized tonic-clonic seizure (grand mal epilepsy)
•
Initially there is loss of consciousness during which the patient can fall to the
ground causing self injury.
•
Followed by brief tonic phase with arms are flexed at elbows and legs are
extended. Tongue bite cry or moan sound can occur during this stage
•
Followed by clonic phase which is rhythmic flexion-extension of arms and legs.
Incontinence can occur during this stage.
•
Finally post-ictal confusion.
generalized seizures
Tonic- clonic
Tonic, atonic
Clonic
Myoclonic
Absence
Absence seizure (petit mal epilepsy)
•
Typical age of onset is 4-10 years
•
Sex girls are 2 to 5 times more likely to have absence seizures.
•
characterized by abrupt onset of impaired consciousness and unresponsiveness
lasting approximately
1-
10 seconds
, occurring up to
hundreds of times per day
.
•
The seizures can be provoked by
hyperventilation
in approximately
90%
of
children.
•
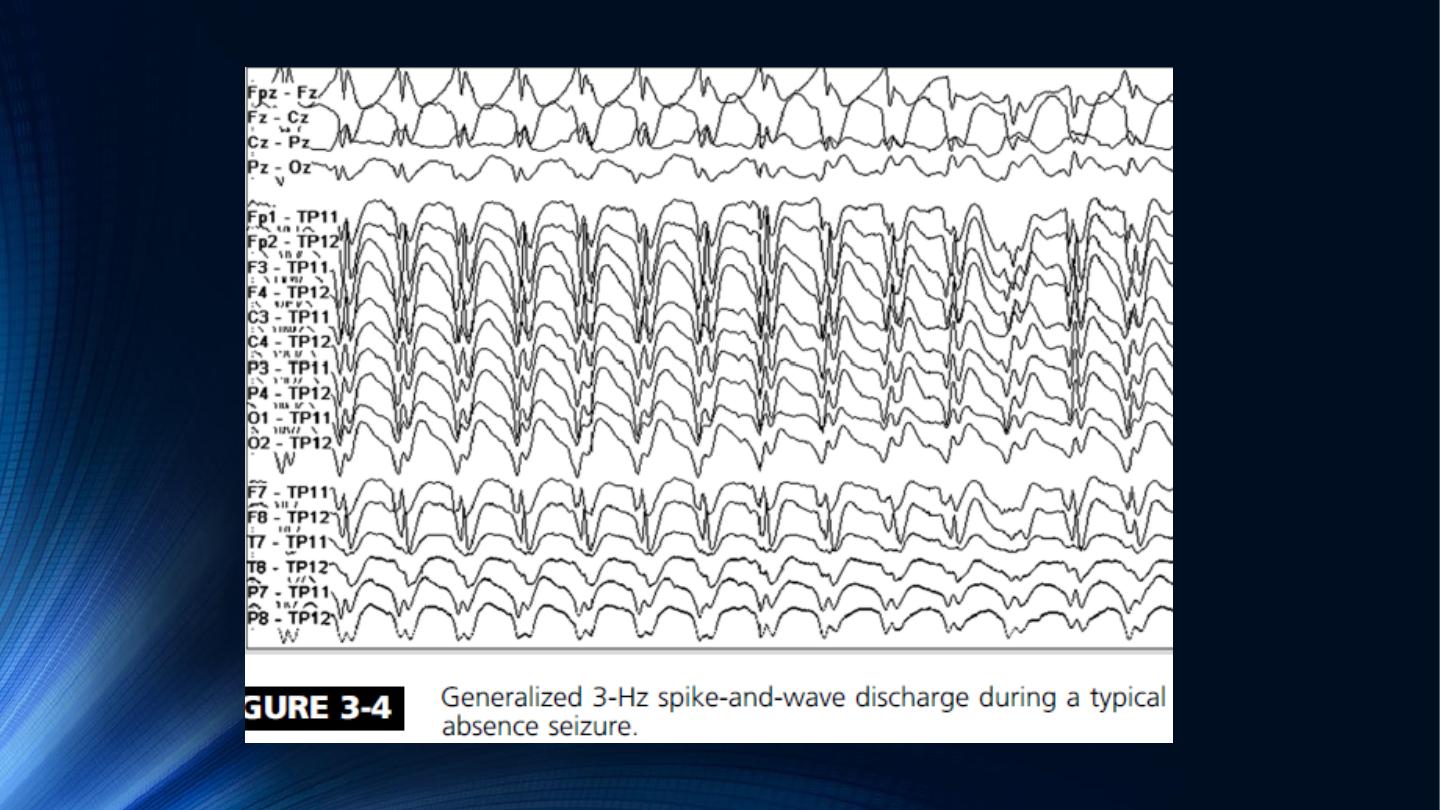
The EEG demonstrates generalized symmetric 3-Hz spike-wave discharges.
•
Prognosis: complete remission of epilepsy
2 to 6 years
after onset.
•
Treatment: drug of choice
Ethosuximide
Juvenile
Myoclonic
Epilepsy
•
12-18 years
100%
will have myoclonic seizures, 96% will have generalized
tonic-clonic seizures, and only 20% will experience absence seizures.
•
JME tend to occur in the morning upon awakening provoked by sleep
deprivation, alcohol consumption, menstruation and photosensivity which is
present in 30-90% of cases.
•
Genetics autosomal dominant linked to ch.6
•
Treatment The traditional treatment for JME is valproic acid, with a response
rate of 85% to 90%.
•
The response to AED medications is typically excellent However, JME is usually a
lifelong disorder with only 10% of patients able to discontinue AED medications.
DIFFERENTIAL DIAGNOSIS OF SEIZURE
•
The most common non-neurologic disorder mimicking epilepsy is
syncope
.
•
Syncope most frequently results from:
•
Cardiogenic causes of syncope result from bradyarrhythmia or tachyarrhythmia,
Orthostatic hypotension results from a fall in blood pressure following a
positional change to standing from a recumbent position and is a frequent cause
of syncope in patients who are elderly or diabetic with autonomic neuropathy.
Non-neurologic Differential Diagnosis
cardiogenic
vasovagal
hypotensive causes
•
Several paroxysmal neurologic disorders can be confused with epilepsy,
including:
Neurologic Differential Diagnosis
Cerebrovascular disease
Delirium
migraine
Movement disorders
including paroxysmal dystonias and dyskinesias and some tremor
disorders, may also resemble epileptic seizures. EEG is invariably
normal during subcortically generated movement disorders.
TIAs typically last from minutes to 1 hour, symptoms, including
negative symptoms such as numbness, weakness, visual loss, or aphasia
while seizure is often manifested as positive symptoms.
Disoriented to time,
person, place
Incomprehensible
speech
agitated
•
C
•
PNES can be distinguished by:
Psychogenic nonepileptic seizures (PNES)
prolonged spell duration
“ often
much longer than 1 minute”
eye closure during the
spell
bizarre voluntary
movements
,
prominent pelvic
thrusting
atypical non anatomic spread of
movements
lack stereotypy across
different events
INVESTIGATION OF THE PATIENT WITH SEIZURES
•
Investigations with
EEG
and
neuroimaging
is essential to consider in the
evaluation of most patients presenting with seizures or spells.
•
These investigation aim to:
1.
Diagnosis of epilepsy and possible underlying cause.
2.
help determine the prognosis for future seizure recurrence.
•
An epileptiform pattern seen on EEG after a first-time seizure often predicts
recurrence range from 30% to 70% in the first year.
•
The clinical applications of EEG include:
1.
diagnosis of epilepsy.
2.
selection of AED therapy.
3.
evaluation of response to treatment.
4.
determination of candidacy for drug
withdrawal.
5.
surgical localization.
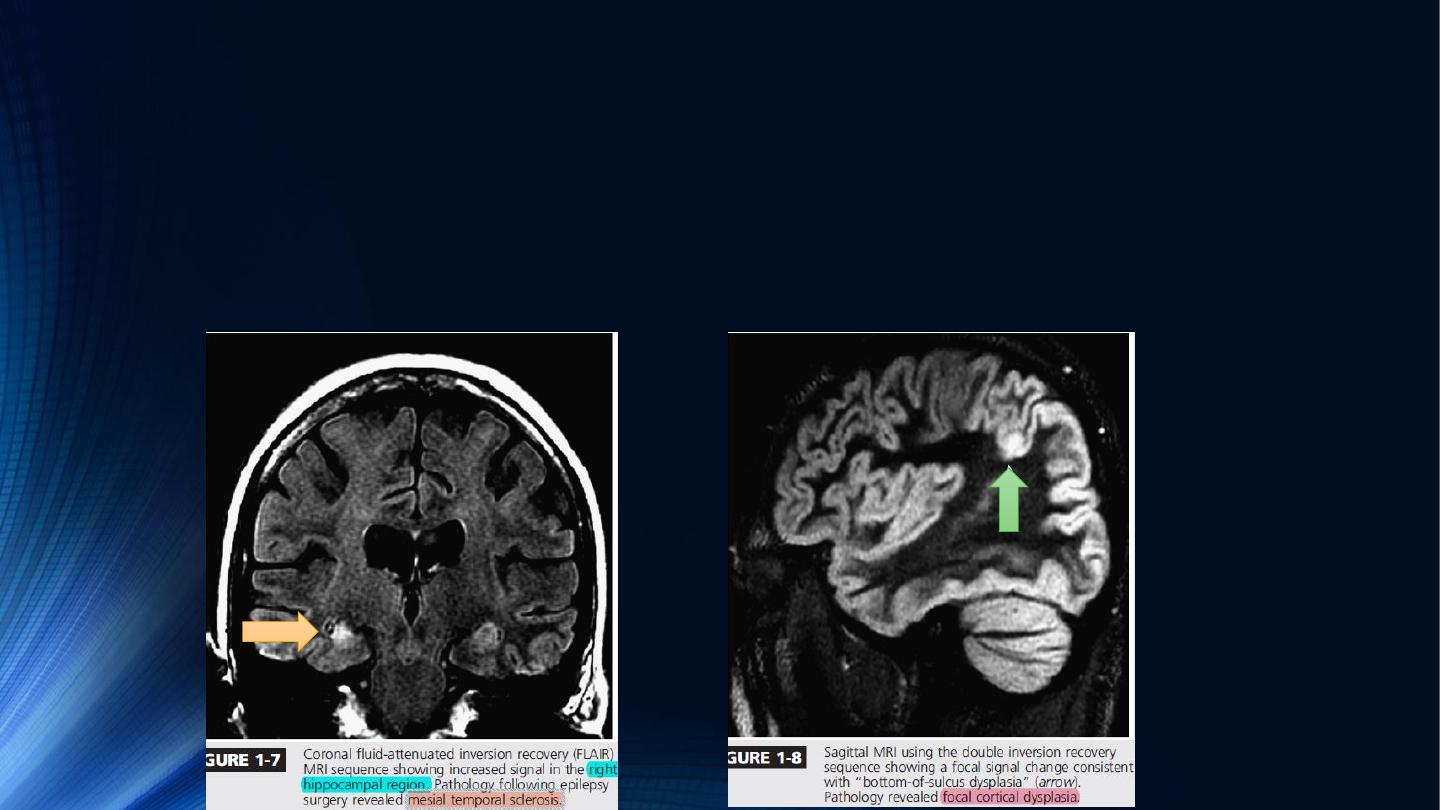
Magnetic Resonance Imaging
•
MRI is used for identification of the pathologic findings associated with focal or
generalized seizures, localization of the epileptogenic zone, and determination
of surgical localization in drug-resistant focal epilepsy.

MANAGEMENT OF EPILEPTIC SEIZURE
After first seizure we have to ask ourselves the following questions:
•
Is it seizure or not?
•
Is it partial or generalized?
•
Seizure type?
•
Is there any metabolic disturbances?
•
What are the recommended investigations?
• Blood test (CBC ,electrolytes,
sugar, RFT, LFT).
• Urine and blood screen for drugs
• EEG
• MRI/CT
• LP if there is suspicion of CNS
infection
•
Start AEDs or not?
•
Decisions about weather to treat or not a patient after a first unprovoked seizure
depend on:
1.
Abnormal neurological examination.
2.
Abnormal EEG.
3.
Abnormal neuroimaging.
4.
Nocturnal seizure.
5.
Strong positive family history of epilepsy.
the chance of having a second seizure

Why the occurrence of second seizure is important?
•
after a first unprovoked seizure, the overall risk for a
second seizure
was only
33%
. After a second seizure, however, the risk of a
third unprovoked seizure
rose to
76%.
•
Criteria of AEDs treatments
1.
Choose appropriate drug for seizure type.
2.
Start with only single drug.
3.
Start with the lowest effective dose and increase gradually.
4.
When to add a second AED make sure that no drug interaction exist.
5.
Coast.
