
Hypertension
Presented by:
Leena Mehjin
Yasir Emad
Shahad Mikdad
Rahma Jamal
Supervised by:
Dr. Muhamad Abdulhadi

Definition:
Blood pressure is the force exerted by the blood against
the walls of the blood vessels. The pressure depends on
the work being done by the heart and the resistance of
the blood vessels
.
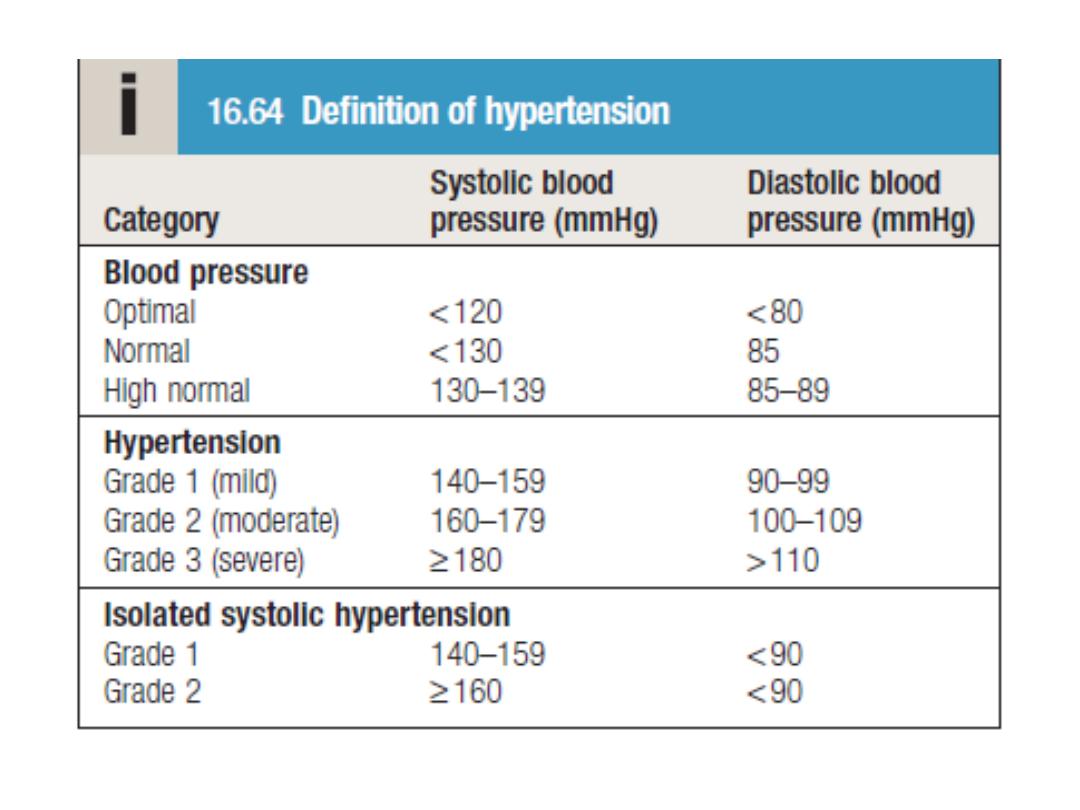
Medical guidelines define hypertension as a blood
pressure higher than 130 over 80 millimeters of
mercury (mmHg), according to guidelines issued by the
American Heart Association (AHA) in November 2017.

Epidemiology:
Hypertension is an epidemic affecting one billion people and is
the commonest risk factor for death throughout the world.
World health statistics 2012 has estimated the prevalence of
hypertension to be 29.2% in males and 24.8% in females.
Approximately 90 percent for men and women who are non
hypertensive at 55 or 65 years will develop hypertension by the
age of 80–85. Hypertension is not limited to rich population and
affects countries across all income groups. Out of total 58.8
million deaths worldwide in year 2004, high blood pressure was
responsible for 12.8% (7.5 million deaths). World over
hypertension is responsible for 51% of cerebrovascular disease
and 45% of ischemic heart disease deaths. Unlike the popular
belief that hypertension is more important for high-income
countries, people in low- and middle-income countries have
more than double the risk of dying of hypertension.

Types of Hypertension
There are two primary types of hypertension. For 95 percent
of people with high blood pressure, the cause of their
hypertension is unknown — this is called essential, or
primary, hypertension. When a cause can be found, the
condition is called secondary hypertension.
Essential hypertension. This type of hypertension is
diagnosed after a doctor notices that your blood pressure is
high on three or more visits and eliminates all other causes of
hypertension. Usually people with essential hypertension
have no symptoms, but you may experience frequent
headaches, tiredness, dizziness, or nose bleeds. Although the
cause is unknown, researchers do know that obesity,
smoking, alcohol, diet, and heredity all play a role in essential
hypertension.

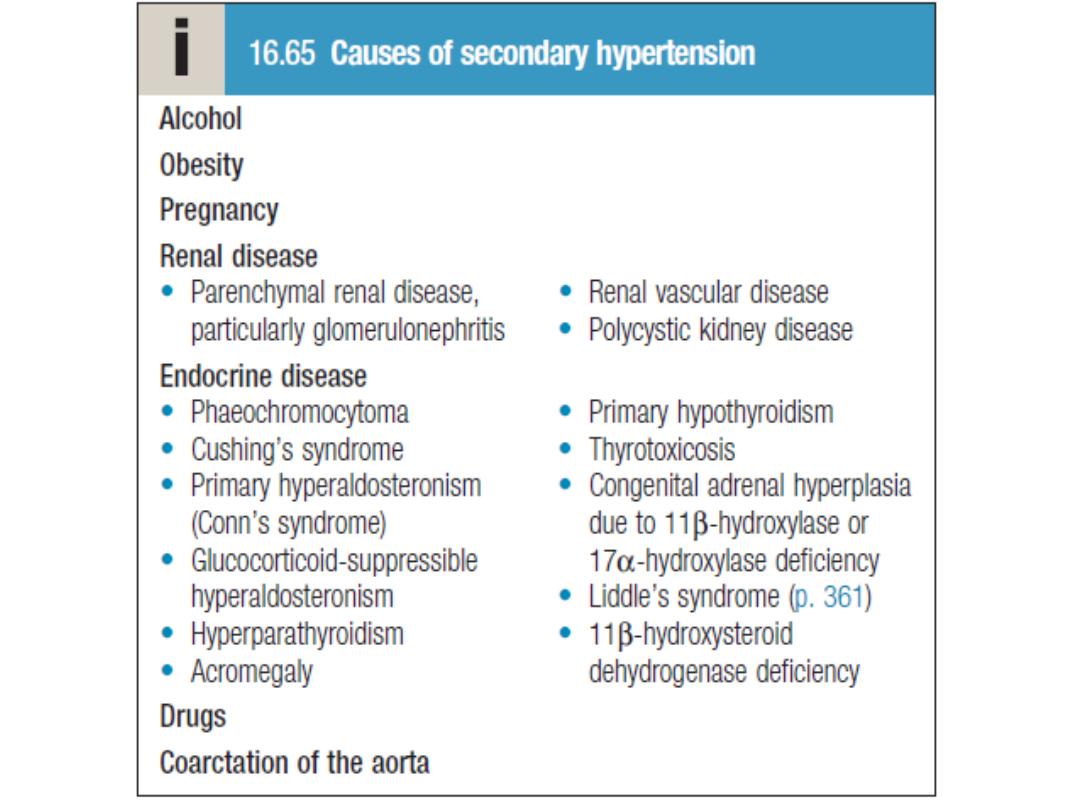
Secondary hypertension.
The most common cause of secondary hypertension is
an abnormality in the arteries supplying blood to the
kidneys airway obstruction during sleep
diseases and tumors of the adrenal glands,
hormone abnormalities
thyroid disease
too much salt or alcohol in the diet
Drugs can cause secondary hypertension, including
over-the-counter medications such as ibuprofen
(Motrin, Advil, and others) and pseudoephedrine
(Afrin, Sudafed, and others)
if the cause is found, hypertension can often be
controlled

Additional Types of Hypertension
Isolated systolic hypertension, malignant hypertension,
and resistant hypertension are all recognized
hypertension types with specific diagnostic criteria.
Isolated systolic hypertension Normal blood pressure
is considered under 120/80. With isolated systolic
hypertension, the systolic pressure rises above 140,
while the lower number stays near the normal range,
below 90. This type of hypertension is most common in
people over the age of 65 and is caused by the loss of
elasticity in the arteries. The systolic pressure is much
more important than the diastolic pressure when it
comes to the risk of cardiovascular disease for an older
person.

Malignant hypertension. This hypertension type
occurs in only about 1 percent of people with
hypertension. It is more common in younger
adults, African-American men, and women who
have pregnancy toxemia. Malignant
hypertension occurs when your blood pressure
rises extremely quickly. If your diastolic pressure
goes over 130, you may have malignant
hypertension. This is a medical emergency and
should be treated in a hospital. Symptoms
include numbness in the arms and legs, blurred
vision, confusion, chest pain, and headache.
It is characterised by accelerated microvascular
damage with necrosis in the walls of small
arteries and arterioles (fibrinoid necrosis) and by
intravascular thrombosis.
The diagnosis is based on evidence of high BP
and rapidly progressive end-organ damage, such
as retinopathy (grade 3 or 4), renal dysfunction
(especially proteinuria) and/or hypertensive
encephalopathy. Left ventricular failure may
occur and, if this is untreated, death occurs
within months
.

Resistant hypertension. If your doctor has prescribed three
different types of antihypertensive medications and your blood
pressure is still too high, you have resistant hypertension.
Resistant hypertension may occur in 20 to 30 percent of high
blood pressure cases. Resistant hypertension may have a genetic
component and is more common in people who are old, obese,
female, African American
Although this may be due to genuine resistance to therapy in
some cases, a more common cause of treatment failure is non-
adherence to drug therapy.
Resistant hypertension can also be caused by
failure to recognise an underlying cause, such as renal artery
stenosis or phaeochromocytoma

Pathogenesis
Many factors may contribute to the regulation of BP and the development of
hypertension, including:
renal dysfunction
peripheral resistance
vessel tone
endothelial dysfunction,
autonomic tone
insulin resistance
neurohumoral factors
Hypertension is more common in some
ethnic groups, particularly African Americans and Japanese, and
approximately 40–60% is explained by genetic factors. Age is a
strong risk factor in all ethnic groups. Important environmental
factors include a high salt intake, heavy consumption of alcohol,
obesity and lack of exercise. Impaired intrauterine growth and low
birth weight are associated with an increased risk of hypertension
later in life.
Clinical features
Hypertension is usually asymptomatic until the
diagnosis is made
at a routine physical examination or when a
complication arises.
Reflecting this fact, a BP check is advisable every 5
years in adults
over 40 years of age to pick up occult hypertension.
Sometimes
clinical features may be observed that can give a
clue to the
underlying cause of hypertension.

•
These include radio-femoral
•
delay in patients with coarctation of the aorta (see Fig. 16.93,
•
p. 534), enlarged kidneys in patients with polycystic kidney
•
disease (p. 405), abdominal bruits that may suggest renal
artery
•
stenosis (p. 406), and the characteristic facies and habitus of
•
Cushing’s syndrome (Box 16.65). Examination may also reveal
•
evidence of risk factors for hypertension, such as central
obesity
•
and hyperlipidaemia. Other signs may be observed that are
due
•
to the complications of hypertension. These include signs of
left
•
ventricular hypertrophy, accentuation of the aortic component
•
of the second heart sound, and a fourth heart sound. AF is
•
common and may be due to diastolic dysfunction caused by
•
left ventricular hypertrophy or the effects of CAD.

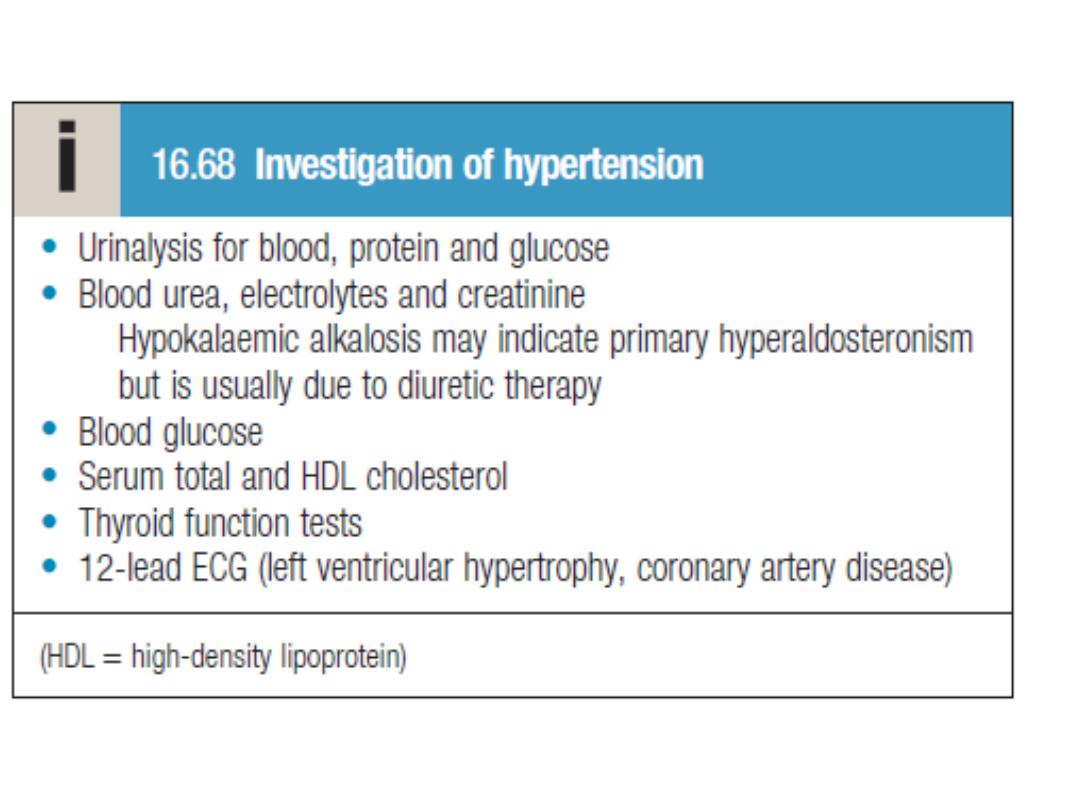
Investigations
•
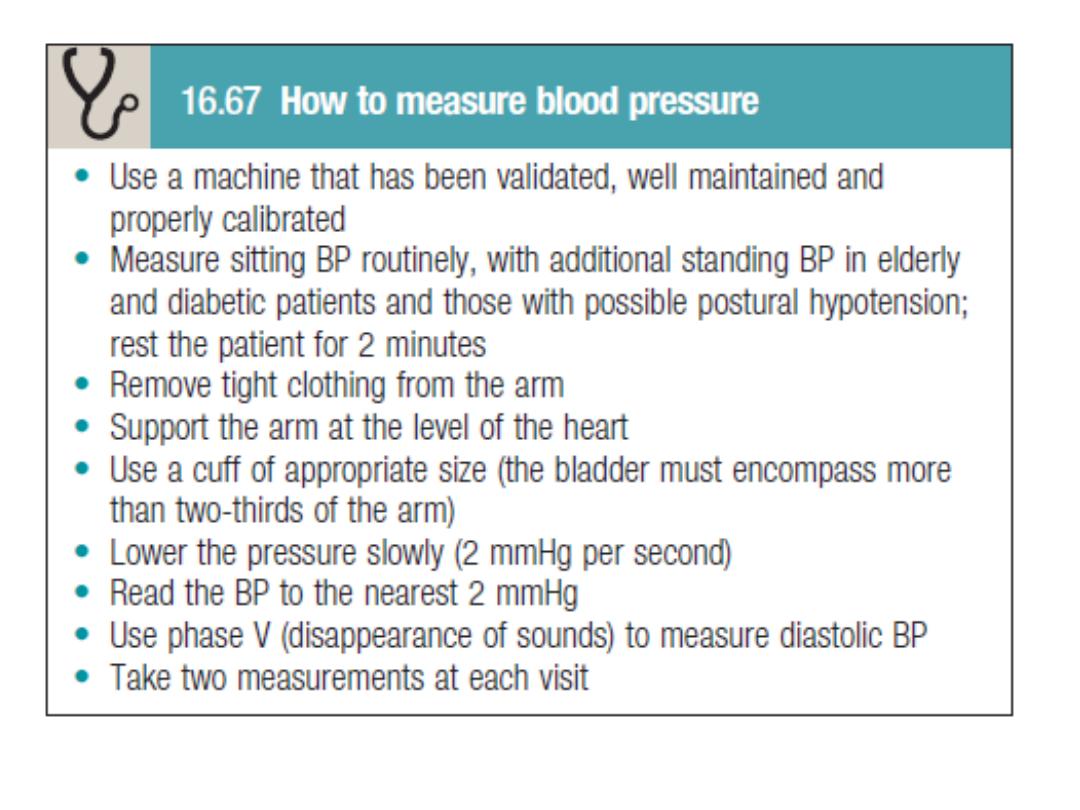
A decision to embark on antihypertensive therapy effectively
•
commits the patient to life-long treatment, so readings must
be
•
as accurate as possible. The objectives are to:
•
• confirm the diagnosis by obtaining accurate, representative
•
BP measurements
•
• identify contributory factors and any underlying causes
•
• assess other risk factors and quantify cardiovascular risk
•
• detect any complications that are already present
•
• identify comorbidity that may influence the choice of
•
antihypertensive therapy.

Target organ damage
The adverse effects of hypertension on the organs .
Blood vessels
In larger arteries (> 1 mm in diameter), the internal
elastic lamina is thickened, smooth muscle is hypertrophied and fibrous
tissue is deposited. The vessels dilate and become tortuous, and their
walls become less compliant In smaller arteries (< 1 mm), hyaline
arteriosclerosis
occurs in the wall, the lumen narrows and aneurysms may
develop. Widespread atheroma develops
and may lead to coronary and cerebrovascular disease,
particularly if other risk factors (e.g. smoking,
hyperlipidaemia, diabetes) are present.
These structural changes in the vasculature often
perpetuate and aggravate hypertension by increasing
peripheral
vascular resistance and reducing renal blood flow, thereby activating the
renin–angiotensin–aldosterone axis. Hypertension is a major risk factor
in the pathogenesis of aortic aneurysm and aortic dissection.

Central nervous system
Stroke is a common complication of
hypertension and may be due to cerebral haemorrhage or
infarction. Carotid atheroma and TIAs are more common
in hypertensive patients. Subarachnoid haemorrhage is
also associated with hypertension.
Hypertensive encephalopathy is a rare
condition characterised by high BP and neurological
symptoms, including transient disturbances of speech or
vision, paraesthesiae, disorientation, fits and loss of
consciousness. Papilloedema is common. A CT scan of the
brain often shows haemorrhage in and around the basal
ganglia; however, the neurological deficit is usually
reversible if the hypertension is properly controlled.

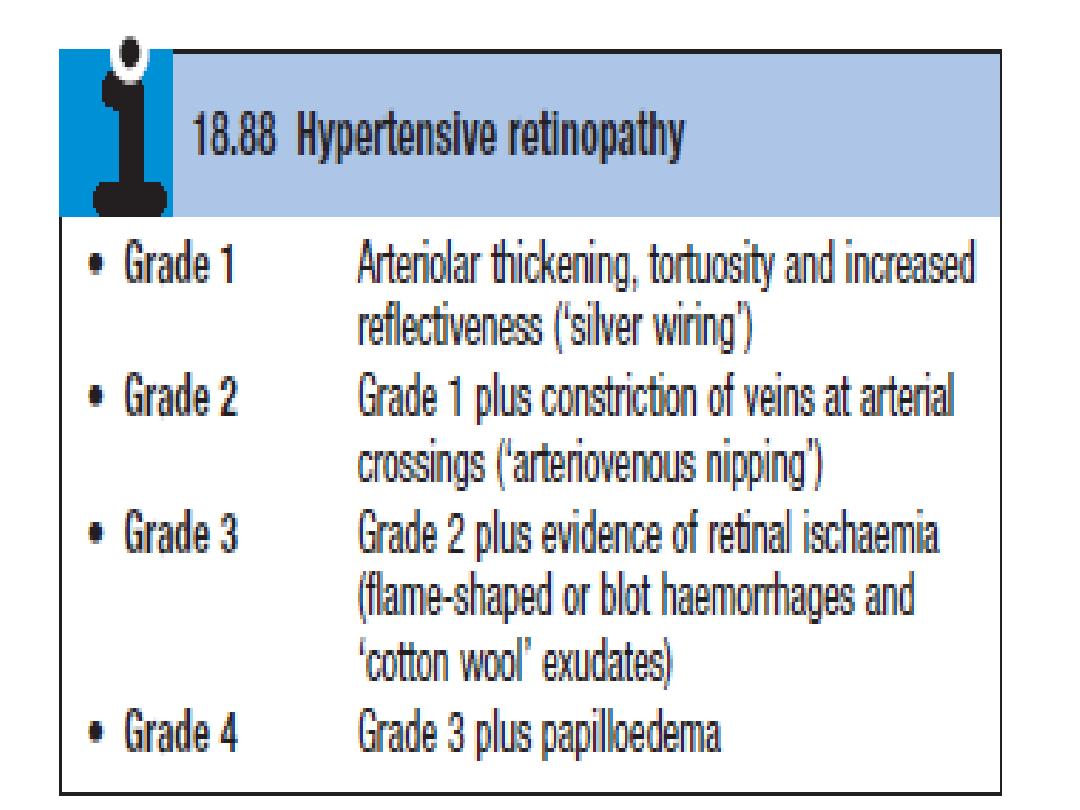
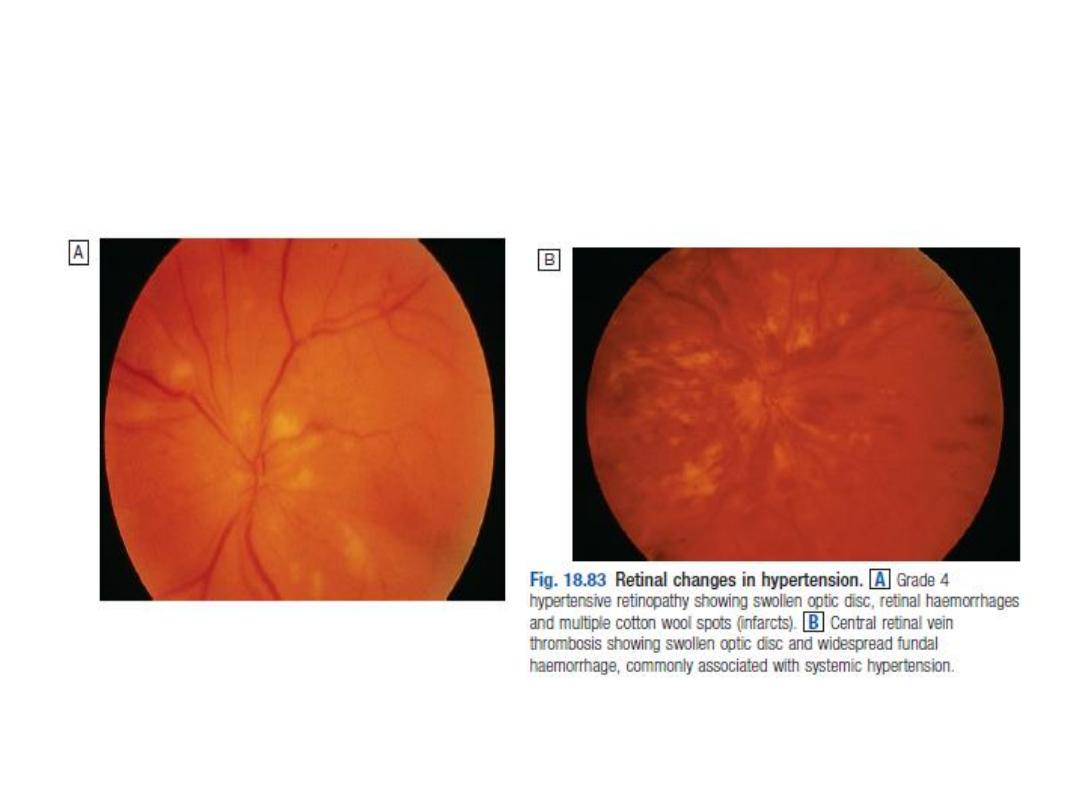
Retina
The optic fundi reveal a gradation of
changes linked to the severity of hypertension;
fundoscopy can, therefore, provide an indication of the
arteriolar damage occurring
Elsewhere.
‘Cotton wool’ exudates are associated with
retinal
ischaemia or infarction, and fade in a few weeks.
‘Hard’ exudates (small, white, dense
deposits of lipid) and microaneurysms (‘dot’
haemorrhages) are more characteristic of diabetic
retinopathy.
Hypertension is also associated with
central retinal vein thrombosis.

Heart
The excess cardiac mortality and morbidity
associated with hypertension are largely due to a higher incidence
of coronary artery disease. High BP places a pressure load on the
heart and may lead to left ventricular hypertrophy with a forceful
apex beat and fourth heart sound.
ECG or echocardiographic evidence of left
ventricular hypertrophy is highly predictive of cardiovascular
complications and therefore particularly useful in risk assessment.
Atrial fibrillation is common and may be due to
diastolic dysfunction caused by left ventricular hypertrophy or the
effects of coronary artery disease.
Severe hypertension can cause left ventricular
failure in the absence of coronary artery disease, particularly
when renal function, and therefore sodium excretion, are
impaired.
Kidneys
Long-standing hypertension
may cause proteinuria and progressive
renal failure by damaging the renal
vasculature.

Management
The objective of
antihypertensive
therapy is to reduce the incidence of adverse
cardiovascular events, particularly CAD,
stroke and heart failure.

Randomised controlled trials have
demonstrated that antihypertensive therapy can
reduce the incidence of stroke and, to a lesser
extent, CAD. The relative benefits (approximately
30% reduction in risk of stroke and 20% reduction
in risk of CAD) are similar in all patient groups, so
the absolute benefit of treatment (total number of
events prevented) is greatest in those at highest
risk.

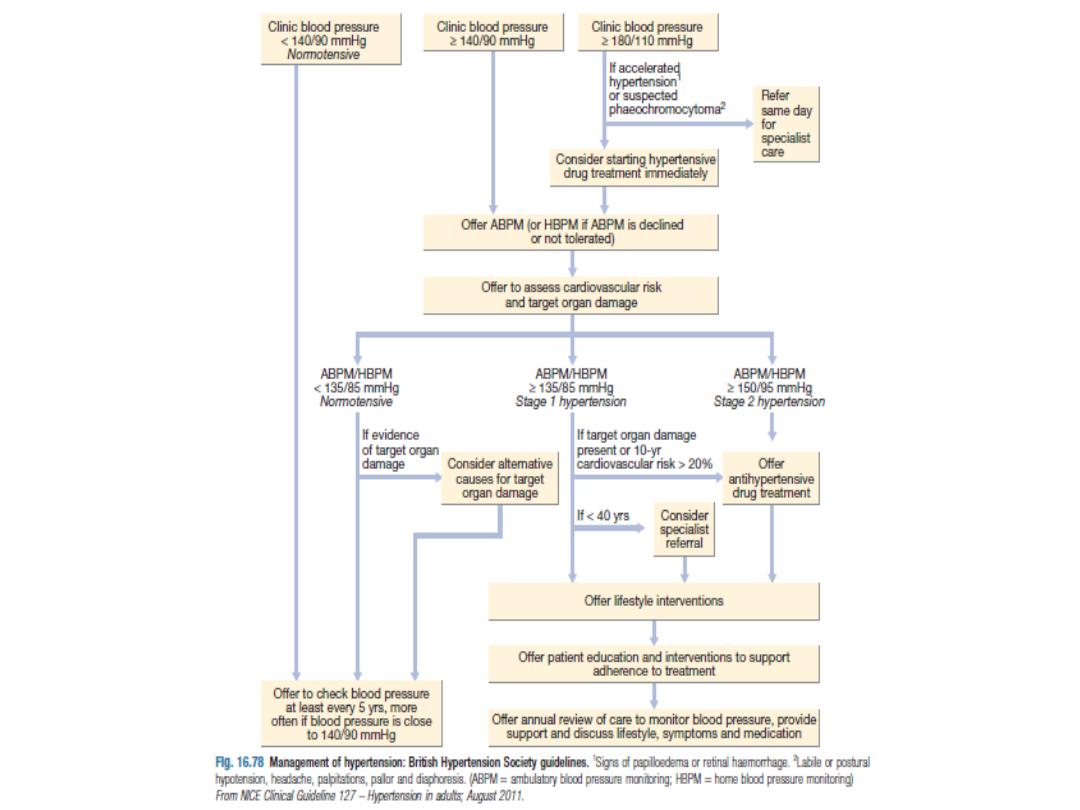
Intervention thresholds
Systolic BP and diastolic BP are both
powerful predictors of cardiovascular risk. The British
Hypertension Society management guidelines therefore
utilise both readings, and treatment should be initiated if
they exceed the given threshold.
Patients with diabetes or cardiovascular
disease are at particularly high risk and the threshold for
initiating antihypertensive therapy is therefore lower (≥
140/90 mmHg) in these patient groups. The thresholds
for treatment in the elderly are the same as for younger
patients.
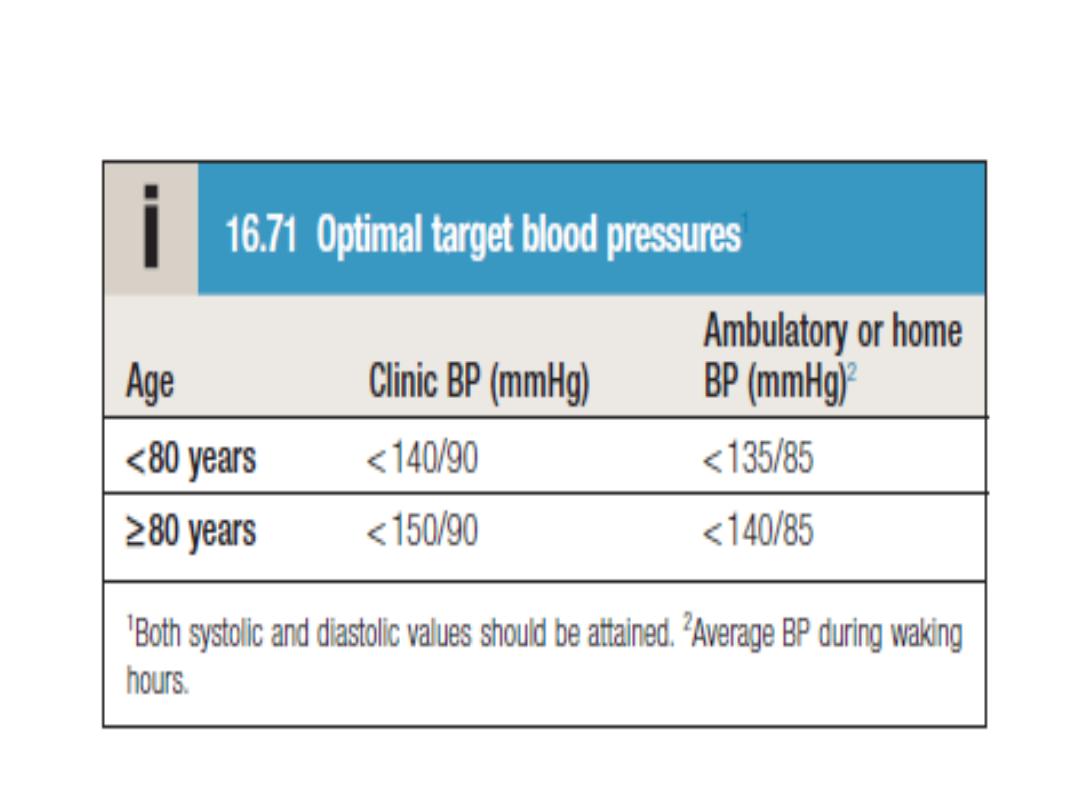
Treatment targets

Non-drug therapy
Appropriate Lifestyle Measures
Correcting Obesity
Restricting Salt Intake
Taking Regular Physical Exercise And Increasing
Consumption Of Fruit And Vegetables can All
Lower BP

Drug therapy
Thiazides The mechanism of action of
these drugs is incompletely understood and it may
take up to a month for the maximum effect to be
observed. An appropriate daily dose is 2.5 mg
bendroflumethiazide or 0.5 mg cyclopenthiazide.
More potent loop diuretics, such as
furosemide (40 mg daily) or bumetanide (1 mg daily),
have few advantages over thiazides in the treatment
of hypertension, unless there is substantial renal
impairment or they are used in conjunction with an
ACE inhibitor.

ACE inhibitors (enalapril 20 mg daily,
ramipril 5–10 mg daily or lisinopril 10–40 mg daily) are
effective and usually well tolerated. They should be
used with care in patients with impaired renal function
or renal artery stenosis because they can reduce
glomerular filtration rate and precipitate renal failure.
Electrolytes and creatinine should be
checked before and 1–2 weeks after commencing
therapy. Side-effects include first-dose hypotension,
cough, rash, hyperkalaemia and renal dysfunction.

Angiotensin receptor blockers ARBs
(irbesartan 150–300 mg daily, valsartan 40–160 mg
daily) have similar efficacy to ACE inhibitors but
they do not cause cough and are better tolerated.

Calcium channel antagonists
Amlodipine (5–10 mg daily) and
nifedipine
(30–90 mg daily) are effective and usually well-
tolerated antihypertensive drugs that are
particularly useful in older people.
Side-effects include flushing,
palpitations and fluid retention. The rate-limiting
calcium channel antagonists (diltiazem 200–300
mg daily, verapamil 240 mg daily) can be useful
when hypertension coexists with angina but may
cause bradycardia. The main side-effect of
verapamil is constipation.

Beta-blockers These are no longer used
as first-line antihypertensive therapy, except in
patients with another indication for the drug such as
angina.
Metoprolol (100–200 mg daily), atenolol
(50–100 mg daily) and bisoprolol (5–10 mg daily),
which preferentially block cardiac β1-adrenoceptors,
should be used rather than non-selective agents that
also block β2- drenoceptors, which mediate
vasodilatation and bronchodilatation.

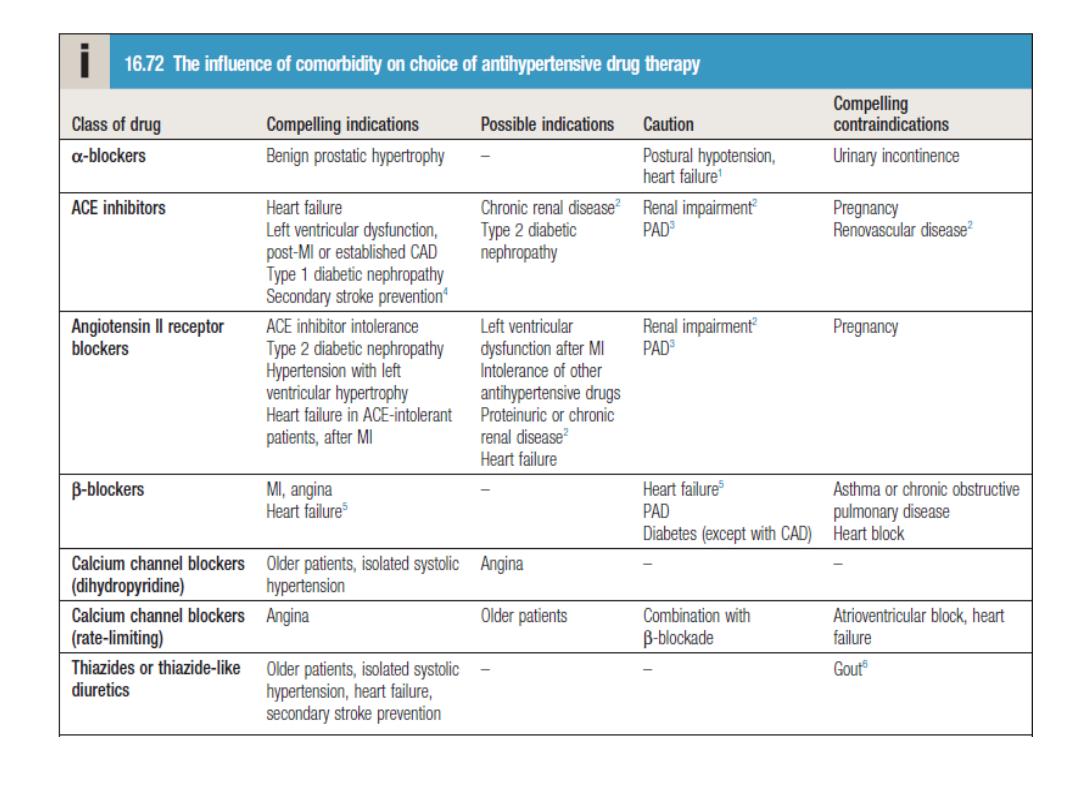
Choice of antihypertensive drug
The choice of antihypertensive therapy is
initially dictated by the patient’s age and ethnic
background, although cost and convenience will
influence the exact drug and preparation used.
Response to initial therapy and side-effects guide
subsequent treatment.
Comorbid conditions also have an
influence on initial drug selection (Box 16.72); for
example, a β-blocker might be the most appropriate
treatment for a patient with angina. Thiazide diuretics
and dihydropyridine calcium channel antagonists are
the most suitable drugs for treatment in older people.

Combination therapy
Although some patients can be treated
with a single antihypertensive drug, a combination of
drugs is often required to achieve optimal control.
Combination therapy may be desirable for
other reasons; for example, low-dose therapy with two
drugs may produce fewer unwanted effects than
treatment with the maximum dose of a single drug.
Some drug combinations have
complementary or synergistic actions; for example,
thiazides increase activity of the renin–angiotensin
system, while ACE inhibitors block it.
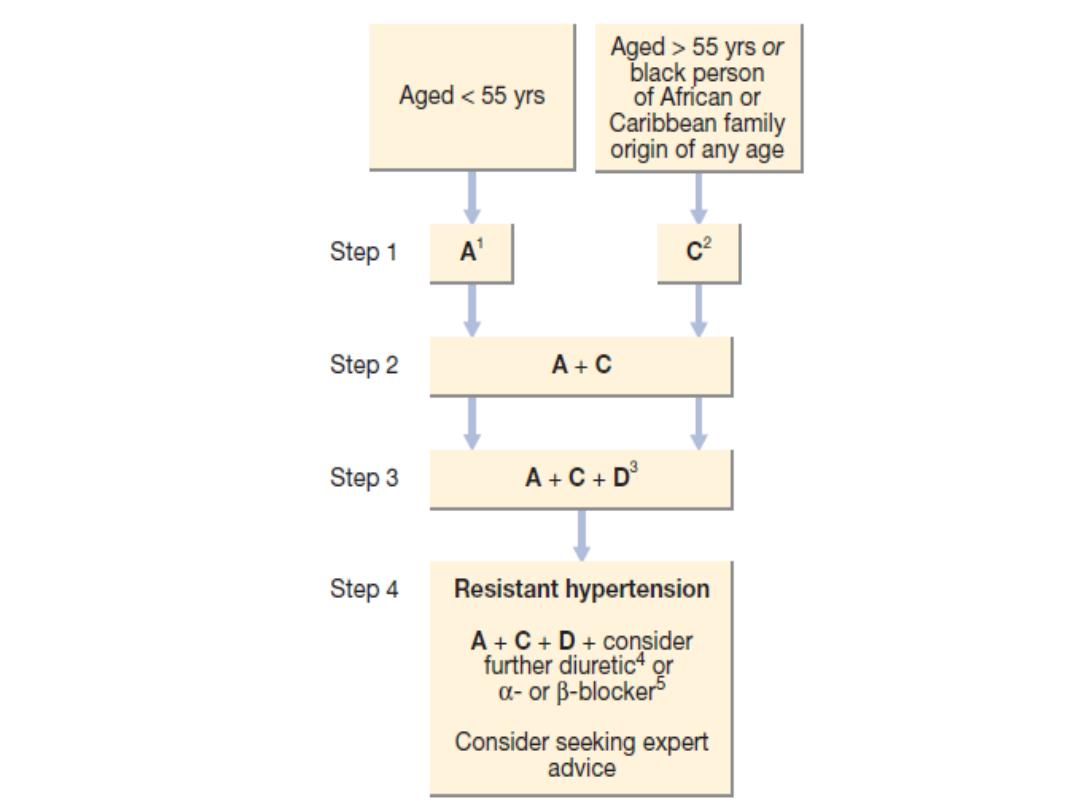

Refractory hypertension
Refractory hypertension refers to the
situation where multiple drug treatments do not give
adequate control of BP. Although this may be due to
genuine resistance to therapy in some cases, a more
common cause of treatment failure is non-adherence to
drug therapy.
Resistant hypertension can also be caused by
failure to recognise an underlying cause, such as renal
artery stenosis or phaeochromocytoma.
There is no easy solution to problems with
adherence but simple treatment regimens, attempts to
improve rapport with the patient and careful supervision
can all help. Spironolactone is a particularly useful addition
in patients with treatment-resistant hypertension.

Accelerated hypertension
Accelerated or malignant hypertension is
a rare condition that can complicate hypertension of
any aetiology. It is characterised by accelerated
microvascular damage with necrosis in the walls of
small arteries and arterioles (fibrinoid necrosis) and by
intravascular thrombosis.
The diagnosis is based on evidence of
high BP and rapidly progressive end-organ damage,
such as retinopathy (grade 3 or 4), renal dysfunction
(especially proteinuria) and/or hypertensive
encephalopathy. Left ventricular failure may occur
and, if this is untreated, death occurs within months>

Management
In accelerated phase hypertension, lowering BP too
quickly may compromise tissue perfusion due to altered
autoregulation and can cause cerebral damage, including occipital
blindness, and precipitate coronary or renal insufficiency. Even in
the presence of cardiac failure or hypertensive encephalopathy, a
controlled reduction to a level of about 150/90 mmHg over a
period of 24–48 hours is ideal.
In most patients, it is possible to avoid parenteral
therapy and bring BP under control with bed rest and oral drug
therapy.
Intravenous or intramuscular labetalol (2 mg/min
to a maximum
of 200 mg), intravenous GTN (0.6–1.2 mg/hr), intramuscular
hydralazine (5 or 10 mg aliquots repeated at half-hourly intervals)
and intravenous sodium nitroprusside (0.3–1.0 μg/kg body
weight/ min) are all effective but require careful supervision,
preferably in a high-dependency unit.
