EMERGENCY COMPLICATIONS
OF CANCER
ZAID THAMER JABER
HIND SALIM AL_kazzaz

Cerebral Oedema and Increased
Intracranial Pressure
Autopsy series show that 25% of patients who die
of cancer have intracranial metastases
The tumor that most commonly metastasizes to
the brain is lung cancer, which is responsible for
30% of brain metastases.
Tumor dissemination to the central nervous
system (CNS) is usually by the hematogenous
route,
Left untreated, metastatic brain tumors cause
progressive neurologic deterioration leading to
coma and death
Clinical presentation:
Metastases can cause focal or global cerebral
dysfunction at presentation. Symptoms usually
develop insidiously and progress over a few
weeks.
Occasionally, the onset is sudden when there is
an acute hemorrhage into a metastatic lesion.
Seizures
Differential diagnosis.

Treatment of Intracranial Hypertension
1-Head position (Head elevation).
2-Hyperventilation: PCO
2
down to (30-34 mmHg).
3-Hypertonic solutions like Mannitol, dose of 1g/kg
4-Steroids (dexamethasone 4mg, 6-hourly).
5-Barbiturates:
6-. Surgery (for single lesion) Radiotherapy or
Chemotherapy..
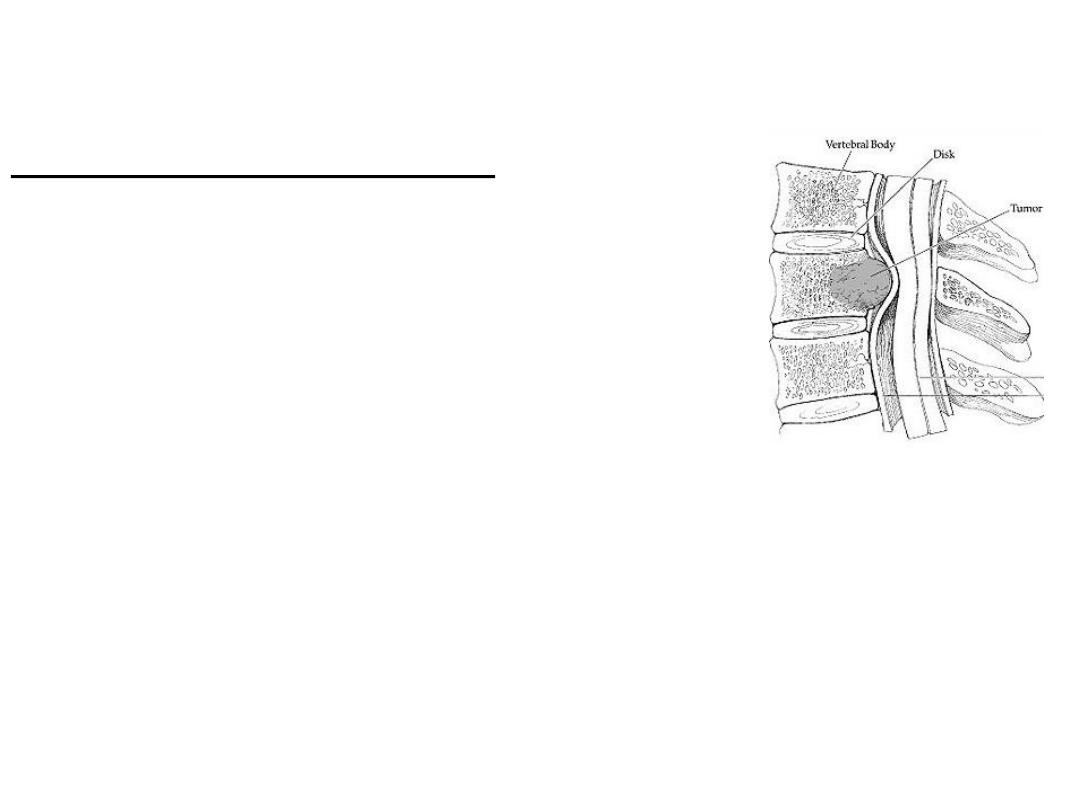
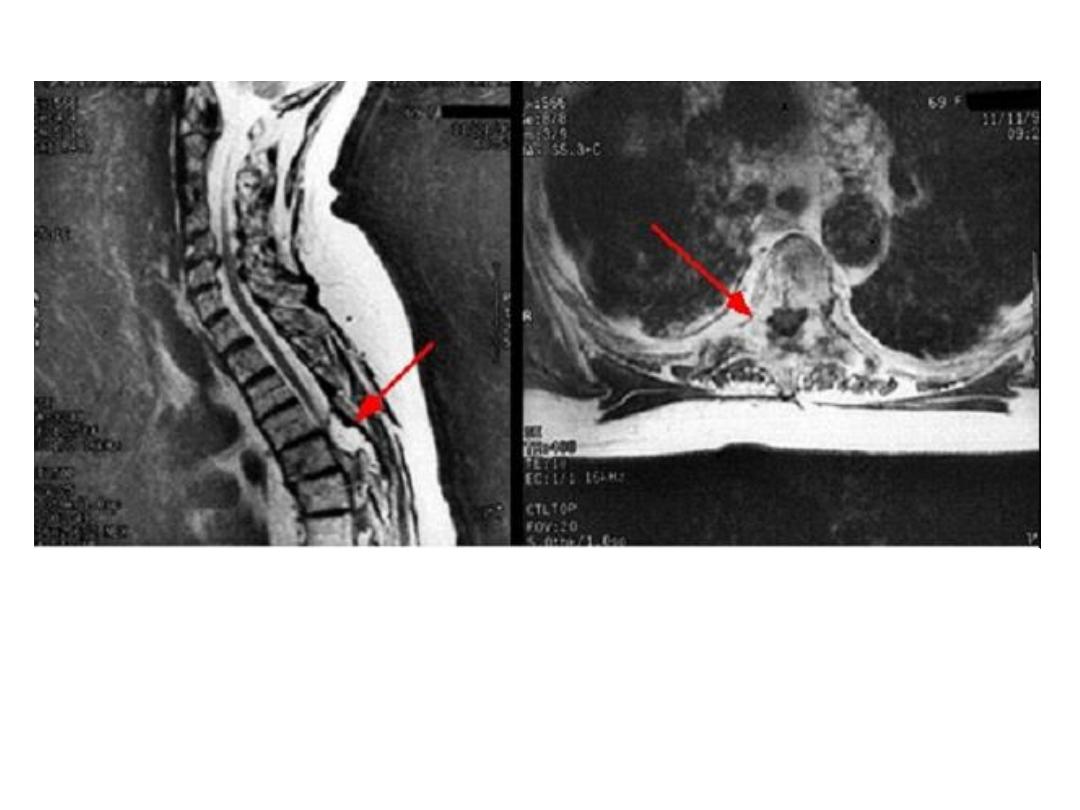
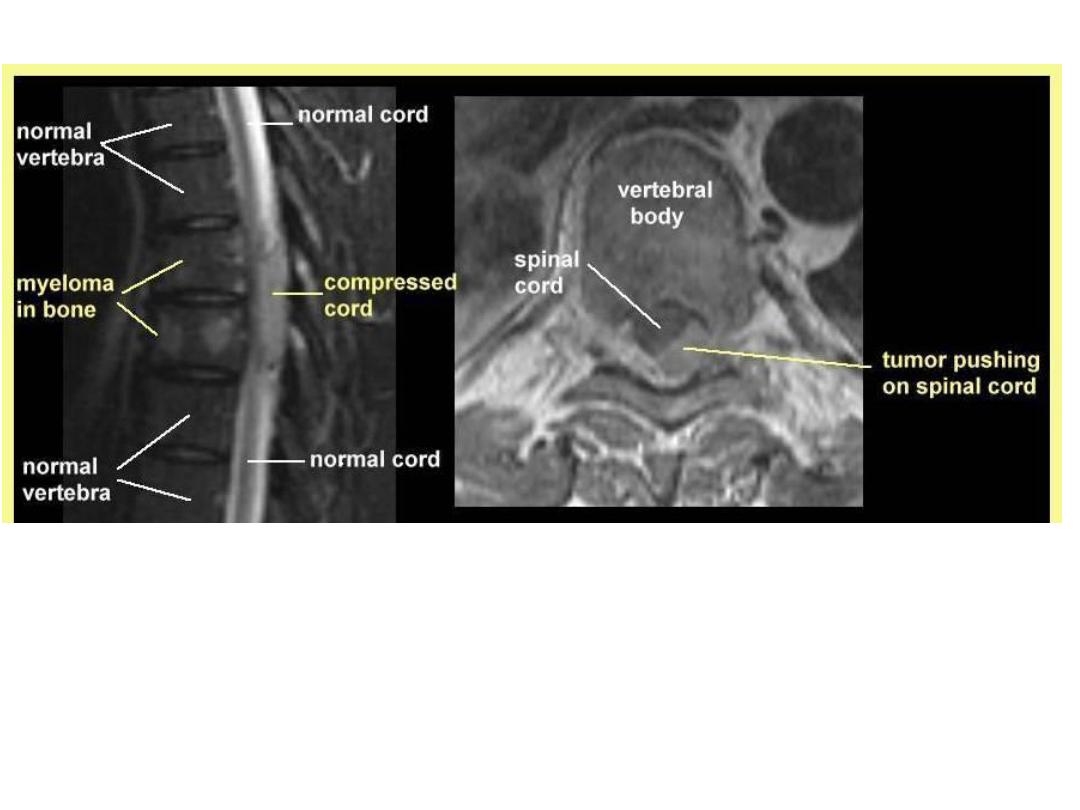
Spinal cord compression
Spinal cord compression: complicates
5% of cancers and is most common in
myeloma, prostate, breast and lung
cancers that involve bone.
Cord compression often
results from posterior extension of a
vertebral body
mass but intrathecal spinal cord
metastases can cause
similar signs and symptoms.
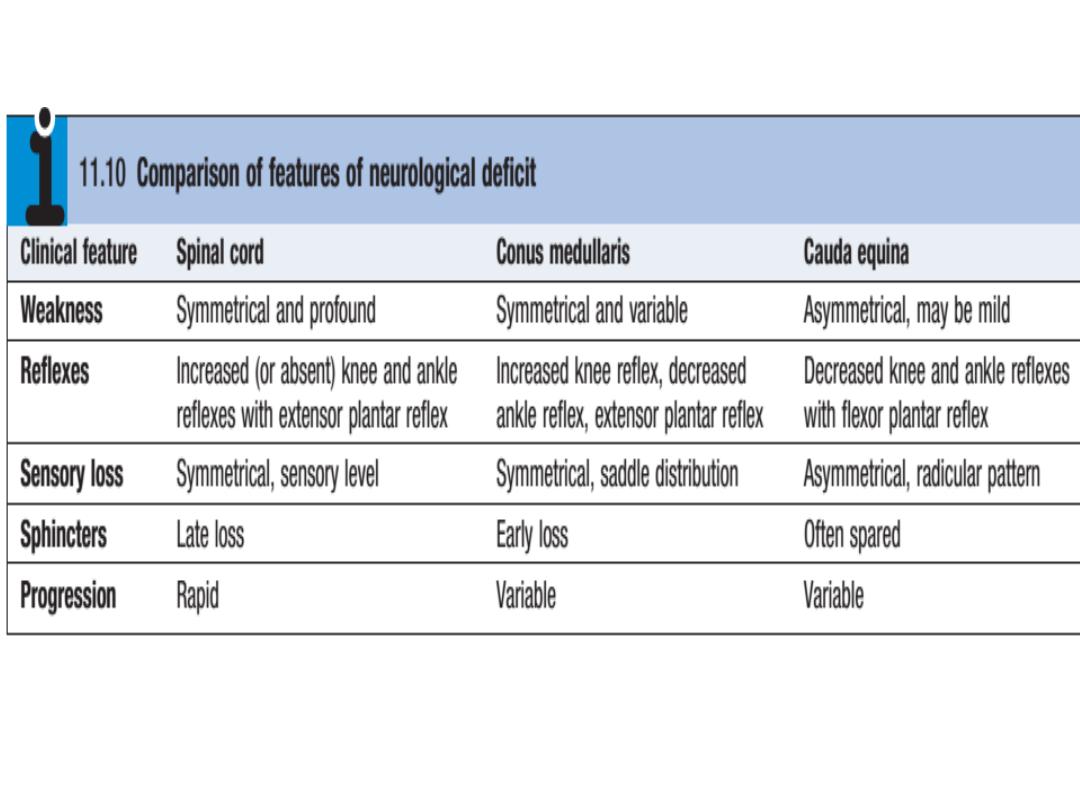
Clinical features
The earliest sign
is back pain
, particularly on
coughing and lying flat. Subsequently,
sensory
changes develop
in dermatomes below the level of
compression and motor weakness distal to the
block occurs. Finally,
sphincter disturbance
, causing
urinary retention and bowel incontinence, is
observed. Involvement of the lumbar spine may
cause
conus medullaris or cauda
equina
compression .
Physical examination:reveals findings consistent
with an upper motor neuron lesion, but lower motor
neuron fidings may predominate early on or in cases
of nerve root compression
.
•
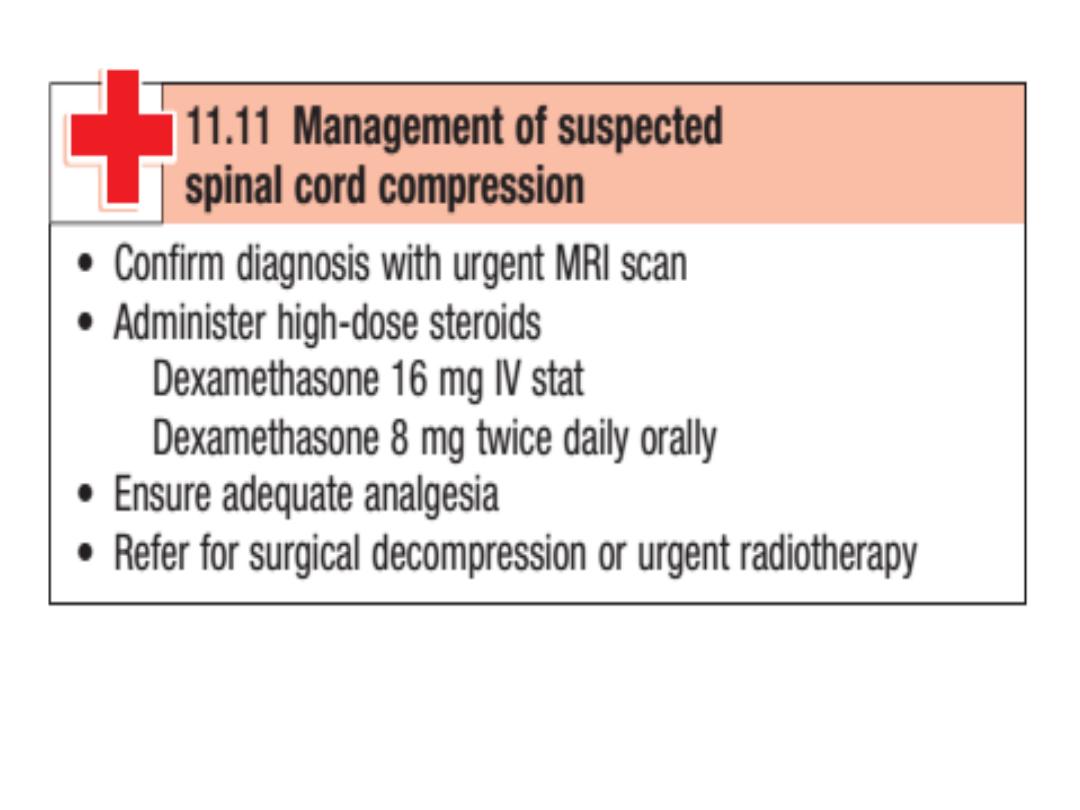
Management
Spinal cord compression is a medical emergency and should
be treated with analgesia and high-dose steroid therapy .
•
Neurosurgical treatment produces superior outcome and
survival compared to radiotherapy alone, and should be
considered fist for all patients.
•
Radiotherapy is used for the remaining patients and selected
tumour types when the cancer is likely to be radiosensitive.
•

The prognosis varies considerably,
depending on tumour type, but the degree
of neurological dysfunction at presentation
is the strongest predictor of outcome
irrespective of the underlying diagnosis.
Ambulation can be preserved in more than
80% of
patients who are ambulatory at
presentation, but neurological function is
seldom regained in patients with
established such as paraplegia
Prognosis

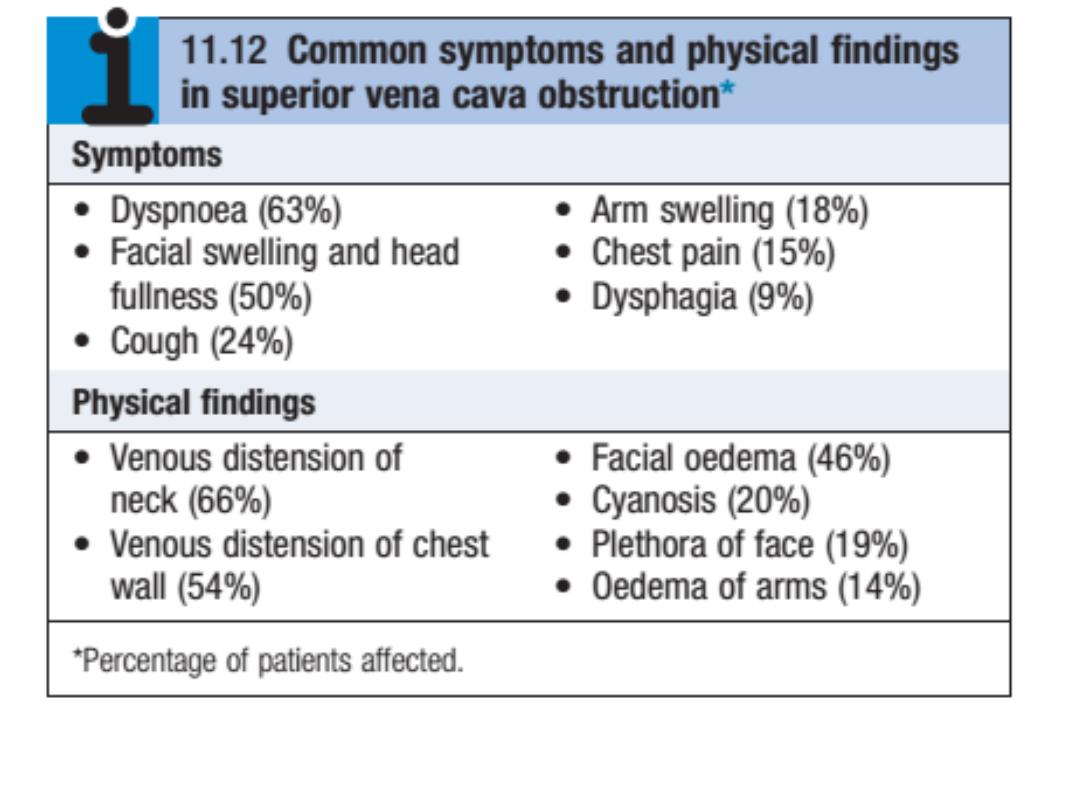
Superior vena cava obstruction
(SVCO) is a common complication of cancer that
can occur through extrinsic compression or
intravascular blockage. The most common
causes of extrinsic compression are lung cancer,
lymphoma and metastatic tumors. Patients with
cancer can also develop SVCO due to
intravascular blockage in association with a
central catheter or thrombophilia secondary to the
tumor.
Clinical features:
The typical presentation is with
oedema
of the arms
and face,
distended neck and arm veins
and
dusky
skin
coloration over the chest, arms and face.
Collaterals
may develop over a period of weeks and
the flow of blood in the collaterals helps to confirm
the diagnosis
. Headache
secondary to cerebral
oedema arising from the backflow
pressure may also occur and tends to be aggravated
by bending forward, stooping or lying down. The
severity of symptoms is related to the rate of
obstruction and the development of a venous
collateral circulation. Accordingly, symptoms may
develop rapidly or gradually.
managemen
Investigations and
CT
of the thorax, it can clinch the diagnosis
and distinguish between extra- and
intravascular causes.
A biopsy
should be obtained when the tumor
type is unknown because tumor type has a
major influence on treatment.
*Treat the cause
Palliative: RT + steroid + multiagent
chemotherapy
Surgical bypass of obstructing lesions


MALIGNANT PLEURAL
EFFUSIONS
Etiology. Malignant tumors causing pleural
effusions are as follows (in order of decreasing
frequency): lung cancer (especially
adenocarcinoma), breast carcinoma,
lymphoma, unknown primary, gastric
carcinoma, ovarian carcinoma, melanoma,
and sarcoma.

MALIGNANT PLEURAL
EFFUSIONS
Types of malignant effusions. Pleural
effusions are usually caused by direct
involvement of the pleura by tumor or by
lymphatic or venous obstruction or both.
Central effusions, particularly those caused by
lymphoma or nerve tissue tumors, may be
chylous and have high-triglyceride and low-
cholesterol concentrations. Atelectasis,
pneumonia, and severe hypoalbuminemia that
complicate malignancy may also cause pleural
effusion.

MALIGNANT PLEURAL
EFFUSIONS
Symptoms and signs. Cough and dyspnea
are the most common symptoms of pleural
effusion. Dullness to percussion, decreased
breath and voice sounds, decreased vocal
fremitus, and egophony are the classic
physical findings. The trachea may be shifted
to the side opposite the effusion. Thickened
pleura from fibrosis or neoplastic involvement
also produces dullness and decreased
vibration.

Management.
1-Respiratory insufficiency caused by malignant
effusion may be relieved by removing up to 1,500 mL
of fluid by needle aspiration. The effusion should be
later tapped dry if possible. Removal of excessive
amounts of pleural fluid can be associated with
reactive pulmonary edema. In a small percentage of
patients, no recurrence of the effusion develops after
a single evacuation. In most cases, the effusion
recurs, and more definitive methods of therapy are
required.
2-Chemotherapy
3. Indwelling pleural catheter
4. Pleurodesis
Hypercalcaemia: is the most common metabolic
disorder
in patients with cancer and has a prevalence of 15
–20
cases per 100 000 persons. The incidence is highest
in
myeloma and breast cancer (approximately 40%),
intermediate in non-small cell lung cancer, and
uncommon
in colon, prostate and small cell lung carcinomas.
• It is most commonly due to over-production of
PTHrP,
which binds to the PTH receptor and elevates
serum
calcium by stimulating osteoclastic bone resorption
and
increasing renal tubular reabsorption of calcium.
• Bone metastasis may also cause hypercalcaemia.
Hypercalcaemia
Clinical features;
The symptoms of hypercalcemia are often
non-specific and may mimic those of the
underlying malignancy.
They include
drowsiness, confusion, nausea and
vomiting, constipation, polyuria, polydipsia and
dehydration
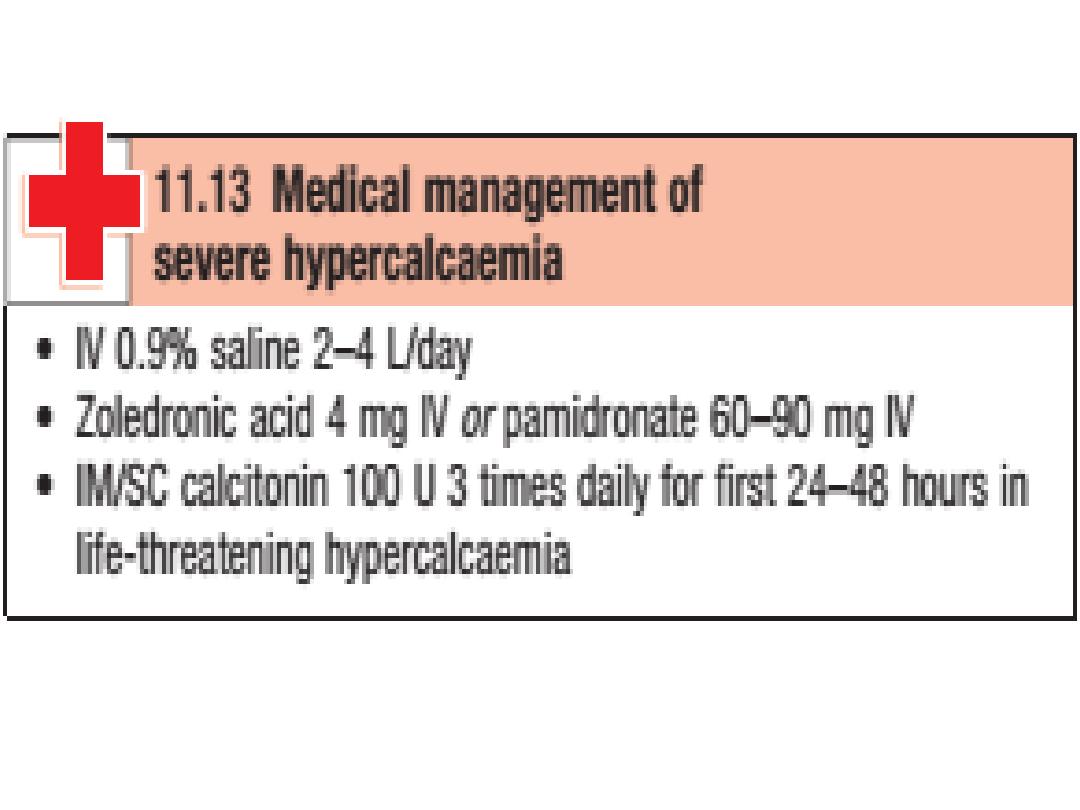
Hypercalcaemia
Investigations and management;
The diagnosis is made by
measuring serum total
calcium
and adjusting for
albumin
. It is especially
important to correct for albumin in cancer
because hypoalbuminemia is common and total
calcium values underestimate the level of ionized
calcium.

TUMOR LYSIS SYNDROME
Effective chemotherapy of several
malignancies may result in the massive
release into the blood of potassium,
phosphate, uric acid, and other breakdown
products of dying tumor cells. Hypocalcemia
may occur with severe hyperphosphatemia.
Tumor lysis syndrome develops within hours to
a few days of treatment for the underlying
neoplasm.

TUMOR LYSIS SYNDROME
Life-threatening complications include
renal failure from precipitation of uric acid
or calcium phosphate crystals in the
kidney, seizures from hypocalcemia, and
cardiac arrhythmias from hyperkalemia or
hypocalcemia.

Diagnosis OF TUMOR LYSIS SYNDROME
Clinical presentation - variable
GI: nausea, vomiting
Fluid imbalances: overload, edema, low
urine
Cardiac: CHF, arrhythmias
MSK: lethargy, cramps, tetany
Neuro: syncope, seizures, and sudden
death.
GU: hematuria, flank or back pain

Diagnosis OF TUMOR LYSIS SYNDROME
Physical examination. Oliguria may call
attention to the metabolic disorders.
Tetany may be a presenting feature.
Cardiac arrhythmias or cardiopulmonary
arrest develop if the process is not
controlled.

Diagnosis OF TUMOR LYSIS SYNDROME
Laboratory studies. Patients treated for acute
leukemia or Burkitt lymphoma should have
measurements of serum levels of potassium,
calcium, phosphate, uric acid, and creatinine
performed daily for 1 week and every few
hours if the syndrome develops.

Management.
Vigorous IV hydration with half-normal saline is
initiated. Severe metabolic problems are treated
as follows:
1. Hypocalcemia,
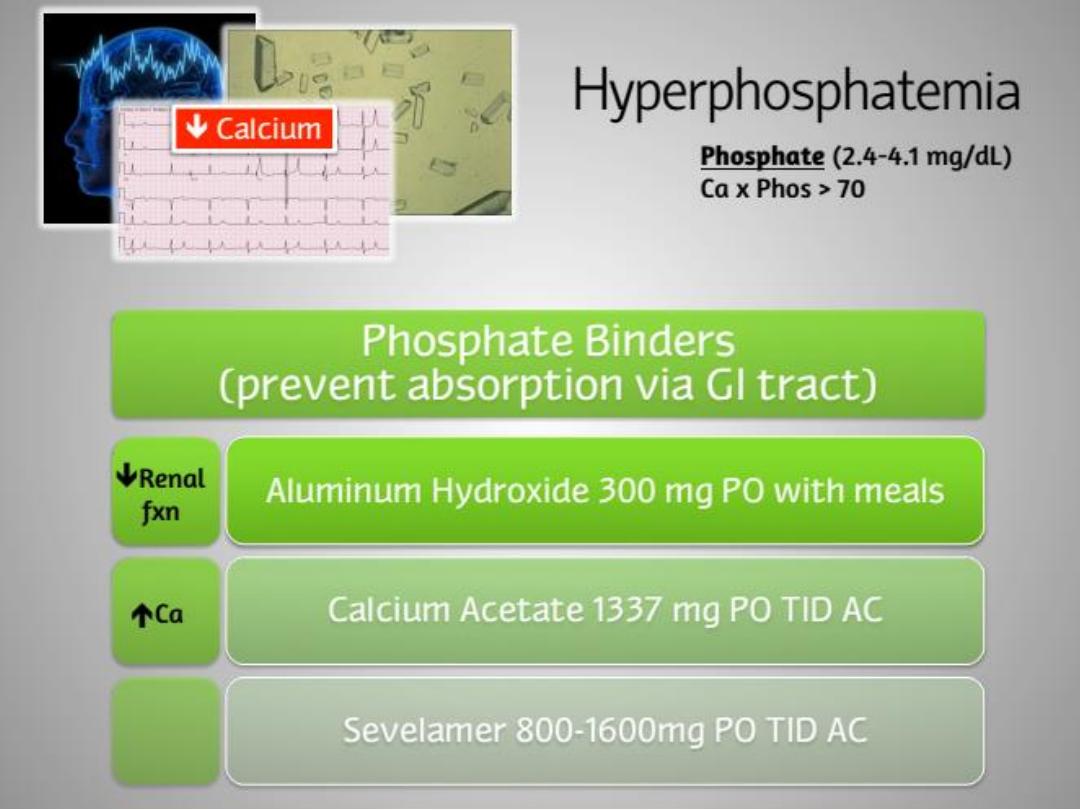
2. Hyperphosphatemia,
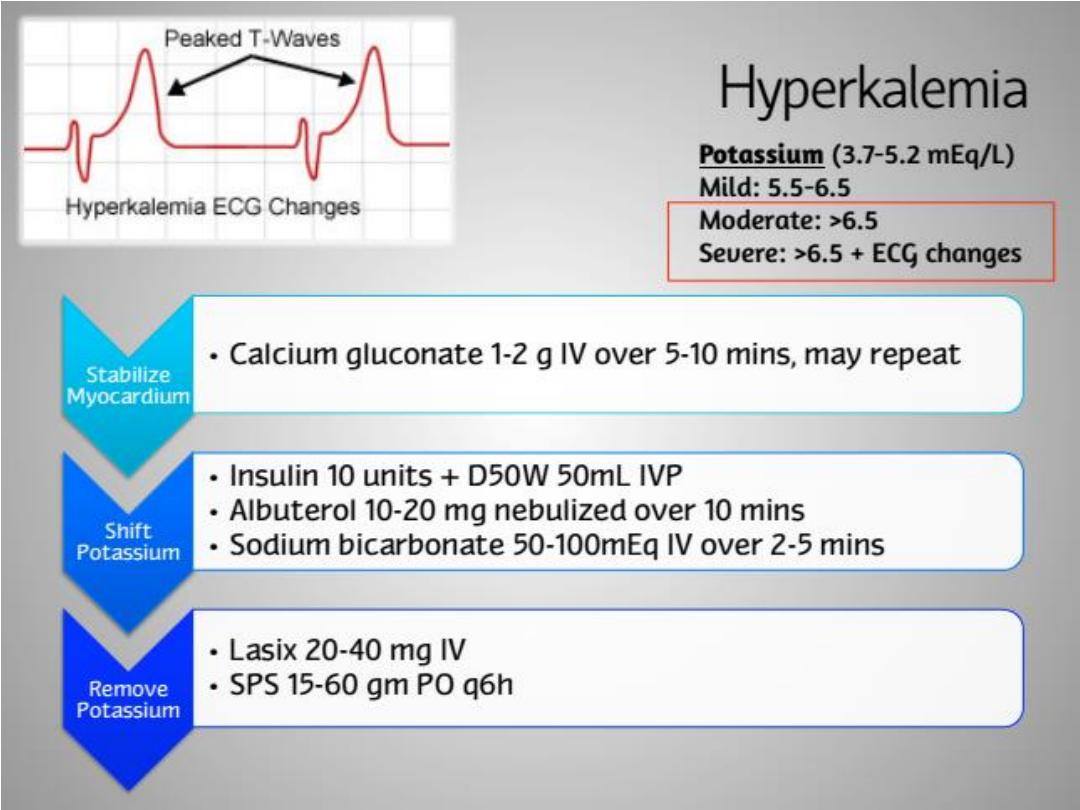
3. Hyperkalemia,
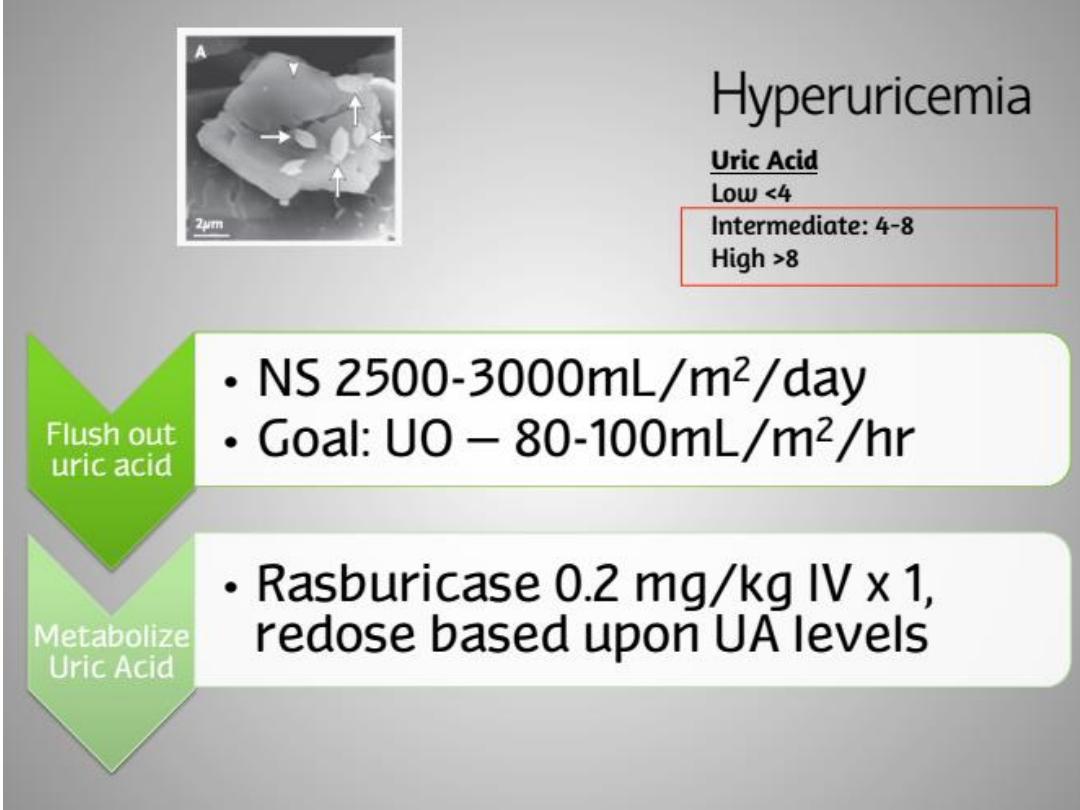
4. Hyperuricemia,
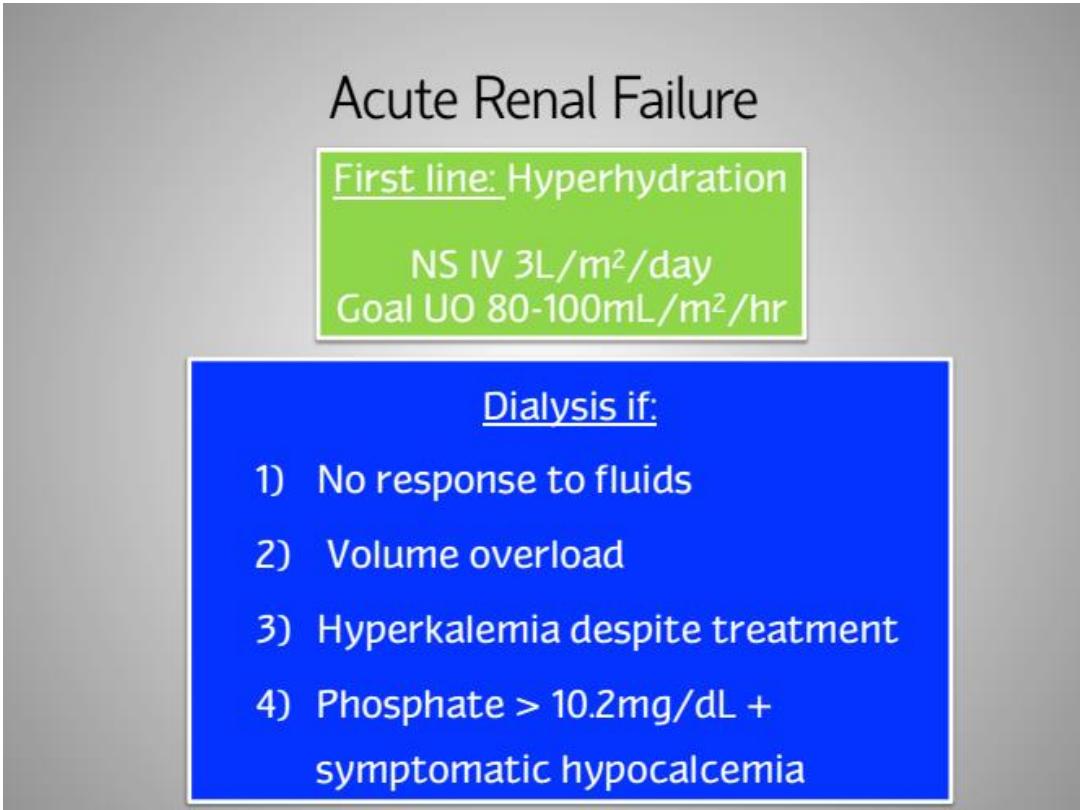
5. Hemodialysis may be necessary on an
emergency basis for patients who do not respond
to treatment or who develop renal insufficiency.