
1
Course: Immunology
Lecturer: Dr. Weam Saad
Lecture: Inflammation
Factors affecting Innate Immunity:
1. Species; e.g. Human not affected by plants pathogens.
2. Race; genetic play role in this factor e.g. all members of particular race
are resistance to certain infections like people of African race are
resistant to malaria.
3. Individual Factors include:
Age: increased age causes increase ability to get infections. Also,
new born are more susceptible to infections due to immature
immune system.
Hormones: e.g. Stress causes release of steroid hormones causing
easy to get infections. Also hyperthyroidism can cause immune-
suppression.
Nutrition: vitamins play role in good immunity, also some viruses
do not multiply in people with malnutrition.
4. Geographic location, this factor affects on normal flora composition and
exposure to the epidemic disease.
Inflammation
It is the innate response of living tissues to any injury or damage in the
site of infection. It is a reaction and an ordered process mediated by the
inflammatory mediators produced by injured tissues and immune cells. This
process consists of four major events:
1. Increased blood supply to the region.
2. Increased capillary permeability in the affected area (vasodilation).
3. Increase the degree of temperature (fever).
4. Migration of W.B.Cs from the blood vessels into the tissues.
2
Neutrophils are the first cells reach inflammatory sites followed by
macrophages and lymphocytes in order to generate an immune response.
Inflammatory mediators include; complement system protiens, fibrin, clotting
plasmin, kinin system, prostaglandin, serotonin, histamine, etc. the function of
these mediators is very important to initiate the immune response.
The Importance of inflammation
1. Limitation of the infection and make it localized.
2. Control the infection by stop spreading of infectious organisms to
the surrounding healthy tissues by forming the fibrin clot around.
3. Activation of the immune system to generate the proper immune
response against the pathogen.
Types of inflammations
1. Acute inflammation
The most common type of inflammations characterized by swallow,
pain, redness and heat at the site of inflammation due to Odema (or edema),
increase blood supply and toxic effects of inflammatory products on nerves
in the site of inflammation the most important sign of acute inflammation is
exudate formation.
Exudate defined as the odema inflammatory liquid forms during acute
inflammations contain high levels of protein, many inflammatory cells, low
glucose, pus and sometimes fibrin clot. The importance of exudates is:
A. Killing causative pathogen.
B. Dilution of toxins in the site of inflammation.
C. Media for immune response (Abs reaction with Ag).
D. Localization of infection and stop spreading.
Pus: it is the solid components of inflammatory exudates contain living and
dead neutrophils and the debris of dead cells of necrotic tissues.

3
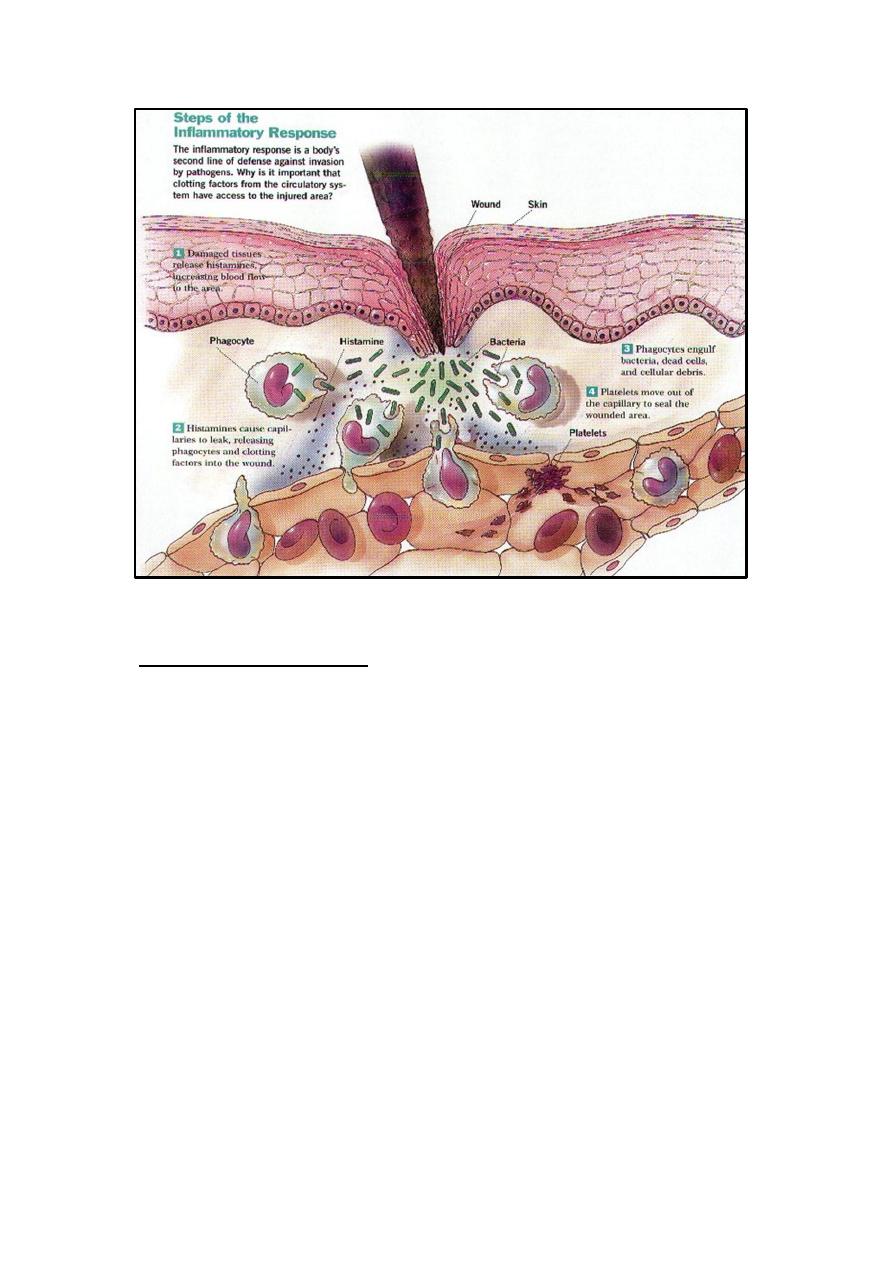
Steps of Acute inflammation
1. After infection, increase permeability of blood vessels in the infected
site.
2. Formation of exudate which contain proteins (e.g. Albumin,
Immunoglobulins, plasmin and fibrin).
3. Aggregation of RBCs due to congestion.
4. Migration of PMNs (polymorph nucleus cells) to the site of
inflammation), followed by monocytes by the effect of chemotaxis.
5. Vesicular changes in the site of inflammation.
6. Repair damage: [re-absorption of liquids, regeneration of damaged cells
of infected tissues by repair blood vessels and fibroblast cells. This
process is called regerntion and that is the end of inflammation.
Factors affect the repair are:
1) Neutrition (vit D and C).
2) Medications and drugs e.g. antibiotics increase repair while cortisone
drugs decrease due to prevent new blood vessels formation.
Types of acute inflammations:
Acute inflammations can be classified according to the type of exudates
formed as following:
1) Serous inflammation (the exudate is serum e.g.: Tuberculosis).
2) Mucoid or catarrhal inflammation (the exudate is mucous e.g. flue or
influenza).
3) Fibrinous inflammation (the exudate is fibrin. e.g.: Diphtheria, caused by
Corynebacteria diptheriae).
4) Purulent or suppulative inflammation (the exudate is pus and called abscess.
5) Combined Inflammation when there is more than one type of inflammation
like muco-purulent or sero-fibrinous usually occur during mixed infections.
4
2.
Chronic inflammation
Occurs when the pathogenic infection last for long time without treatment
or with low immune response or when the pathogen is intracellular parasite
lives inside cells and escape immune system defense mechanisms and has no
Immunogenic antigens, also when the acute inflammation left without
treatment will become chronic inflammation.
Signs of chronic inflammation:
1) Long standing inflammation.
2) Low exudate.
3) Histological changes in tissue (most important sign) e.g.: Hyperplasia,
hypertrophy.
Metaplasia and suppress the physiological function, hence adding
immunosuperssor drugs (like cortisone) to the therapy in order to avoid these
histological changes for example chronic inflammation in middle ear (chronic
otitis media) lead to hearing loss due to ear drum damage.

5
3.
Granulomatous inflammation.
Long standing inflammation transformed from chronic inflammation, occurs
due to internal fungal infections and some intracellular bacterial infections
e.g.: Tuberculosis, laprosy, brucellosis, syphilis, when the pathogenic
microorganism hide and escape from host immune system mechanisms and
hide inside cells.
Granuloma: it is the site of this type of inflammation and composed of nodule
containing a giant cell (merge of macrophage cell) in the center surrounded by
epithelial cells and some lymphocytes with fibrin deposited around these cells.
The Complement System
This system includes over than 20 proenzymes (glycoproteins)
components inactive state found in the blood. When the complement
components are activated, serial, rapid cascad events occur. Historically,
the term complement (C) was used to a heat-labile serum component able
to lyse bacteria and its activity is destroyed (or inactivated) by heating
serum at 56 C ᵒ
for 30 min.
1. Synthesis and metabolism of complement components.
Complement glycoproteins are synthesized by liver cells
(hepatocytes) and macrophages and many other cells (e.g. gut
epithelial cells). All normal individuals have complement
components in their blood. The synthetic rates for the complement
glycoproteins increase when complement is activated and
consumed.
2. Activation of the complement system.
This system can be activated by:
a) Antigen-antibody complexes containing IgG or IgM activate
complement by the classical pathway that starts with C1
(complement 1).
b) Membranes and cell walls of microbial organisms (e.g.
Lipopolyccharides layer [LPS] of gram –ve bacteria) and many

6
other substances can activate complement by the alternative
pathway.
c) Proteolytic enzymes released either from microbes or from host
cells during immune defense mechanisms, can also activate the
complement system by breaking down critical components.
3. The complement cascade induction. When the complement
component is activated, it continues activating the next component by:
either cleaves.
or becomes bound to an activated component or complex of
complement components.
4. Function of the complement system:
The complement system has role in both specific and non-specific
immunity. The functions of the complement system are:
1) Binding and neutralizing foreign substances that activate it.
2) Induce the ingestion of complement-coated substances by
phagocytic cells (help in the opsonization process when C3b and
C4b linked with the surface of microorganisms and attach to
Complement
receptor
on
phagocytic
cells
then
induce
phagocytosis).
3) Activation of many cells including PMNs cells and macrophages
.
4) Have roles in regulation of antibody responses.
5) Clearance of immune complexes and apoptotic cells.
6) Have roles in inflammation and tissue damage.
7) Some components (C3a, C4a and C5a), have role in Anaphylaxis (a
dangerous case of type I hypersensitivity), hence they are called
anaphylotoxins.
8) Some complement components acts as chemotactic factors e.g.
C5a.
7
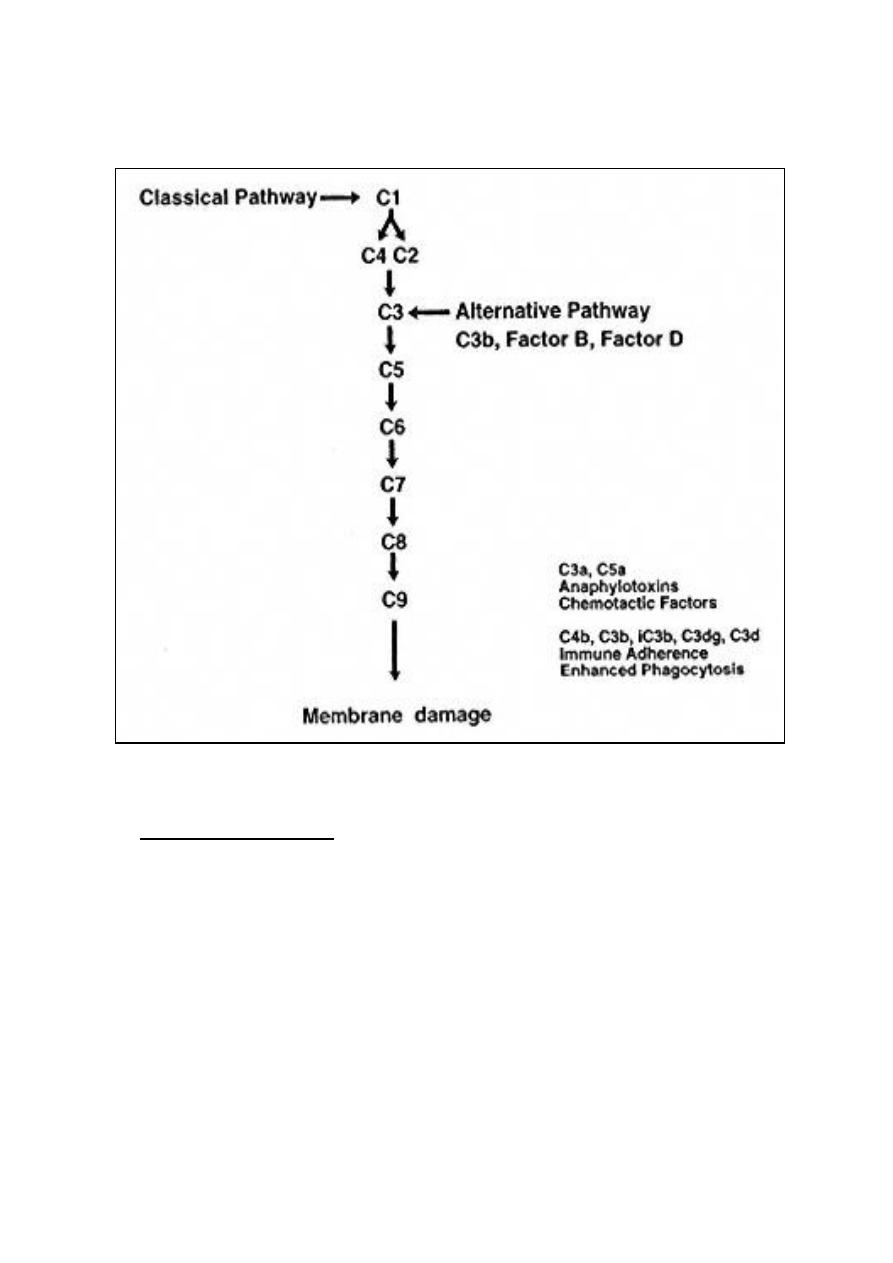
5. Complement Pathways.
(The sequence of complement components activation)
A. Classical Pathway:
1) C1activation
C1, a multi-subunit protein containing three different proteins (C1q,
C1r and C1s), binds to the Fc region of IgG and IgM antibody
molecules that have interacted with antigen (it does not bind to free
Ab) , binding requires calcium and magnesium ions. The binding of
C1q results in the activation of C1r which in turn activates
C1s. The result is the formation of an activated “C1qrs”, which is
an enzyme that cleaves C4 into two fragments C4a and C4b.
8
2) C4 and C2 activation (generation of C3 convertase).
The C4b fragment will stay (usually binds to the binds to the
membrane of bacteria) and the C4a fragment is released. Activated
“C1qrs” also cleaves C2 into C2a and C2b. C2a binds to the
membrane in association with C4b, and C2b is released. The
resulting C4bC2a complex is a C3 convertase (acts as enzyme),
which cleaves C3 into C3a and C3b.
3) C3 activation (generation of C5 convertase):
C3b binds to the membrane in association with C4b and C2a, and
C3a is released (which acts as anaphylaxis protein and a
chemotactic factor). The resulting C4bC2aC3b is a C5
convertase. The generation of C5 convertase is the end of the
classical pathway. Many products of the classical pathway have
biological activities that support the host defenses:
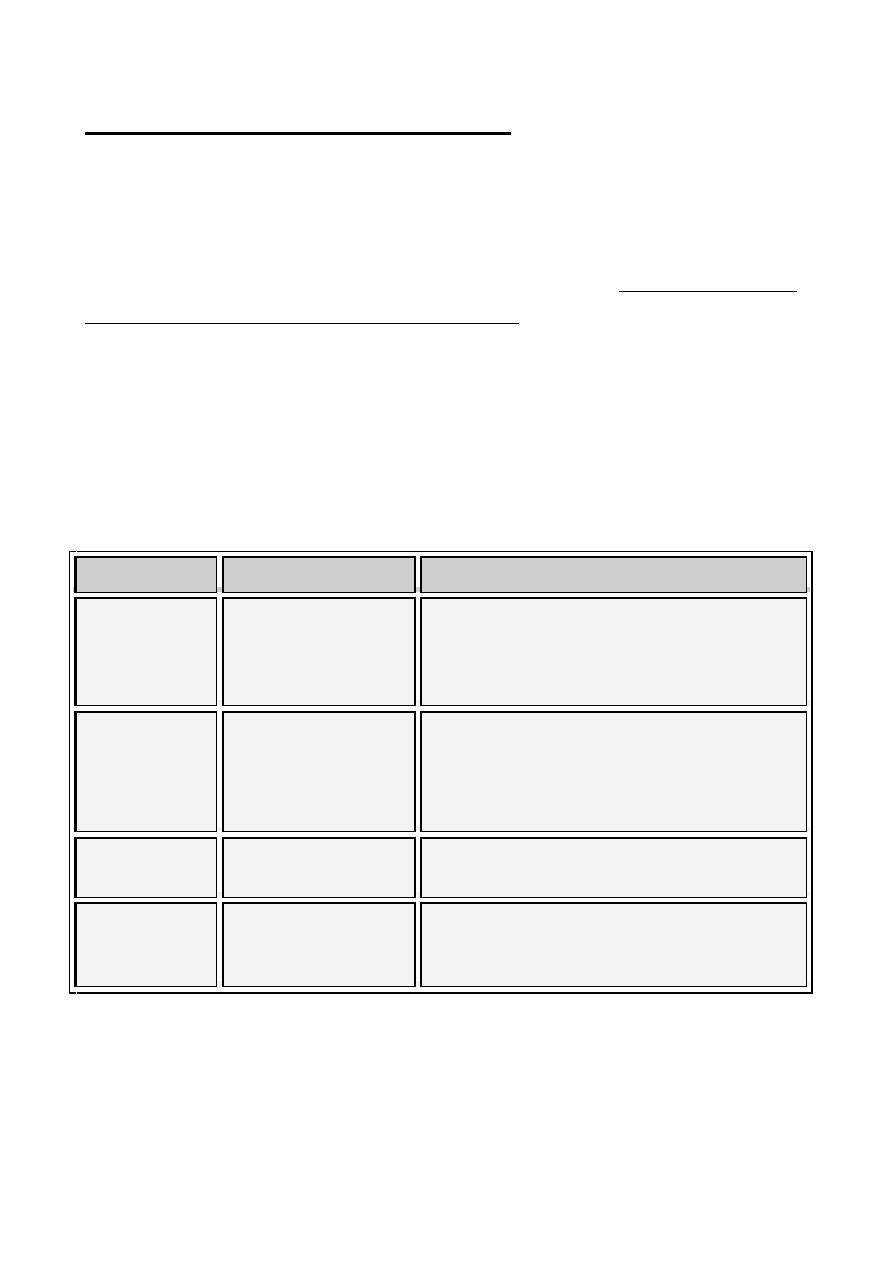
Biological Activity of classical pathway products
Component
Biological Activity
C2b
Prokinin; have role in kinin system, causes edema
C3a
Anaphylotoxin; can activate basophils and mast cells to
degranulate resulting in increased vascular permeability and
contraction of smooth muscle cells, which may lead to
anaphylaxis
C3b
Opsonin; induces phagocytosis by binding to complement
receptors. Activation of phagocytic cells
C4a
Anaphylotoxin (weaker than C3a)
C4b
Opsonin; induces phagocytosis by binding to complement
receptors
9
B. Lectin Pathway
The lectin pathway is very similar to the classical pathway. It starts with
the binding of mannose-binding lectin (MBL) to bacterial surfaces. Many
serial events happens resulting C4bC2aC3b formation, which is the C5
convertase. The generation of C5 convertase is the end of the lectin
pathway.
C.Alternative Pathway
Activation of this pathway starts spontaneously and C3 will be cleaved
by the help of Factor B, Factor D, properdin and Mg
+2
ions. Cleavage of
C3will release C3a (which acts as anaphylaxis protein) and C3b. when
C3b is formed, Factor B will bind to it and will be cleaved by Factor D.
The resulting C3bBb complex is a C5 convertase and this is the end of the
alternative pathway. Generation of C3b is essential for the activation of
the alternative pathway.
The component C3b can be formed due to:
a. During normal C3 turnover in blood
b. In the presence of bacterial proteases
c. During classical pathway activation (for this reason activation of the
classical pathway is always associated with activation of the
alternative pathway which generating more activated C3).
The alternative pathway of complement activation is important
especially during the early phase of an infection, when the concentrations
of specific antibody are very low and classical pathway activation is
limited and in the presence of large numbers of bacteria. The alternative
pathway provides the non-specific resistance against infection without the
need to antibodies and hence provides a first line of defense against a
number of infectious agents.
10
D. Membrane attack complex Formation:
Lytic pathway is the end of all the complement system pathways, C5
convertase from all pathways (classical, lectin or alternative) cleaves C5
into C5a and C5b. Then C5b rapidly binds with C6, C7, C8 and C9
molecules. Pores will be formed in the membrane and lysis occurs due to
physical damage to the membrane. The complex of C5bC6C7C8C9 is
called the membrane attack complex (MAC).
C5a formed in the lytic pathway is the most active anaphylotoxin. It is
a chemotactic factor for neutrophils and stimulates the respiratory burst in
them and it stimulates inflammatory cytokine production by
macrophages.
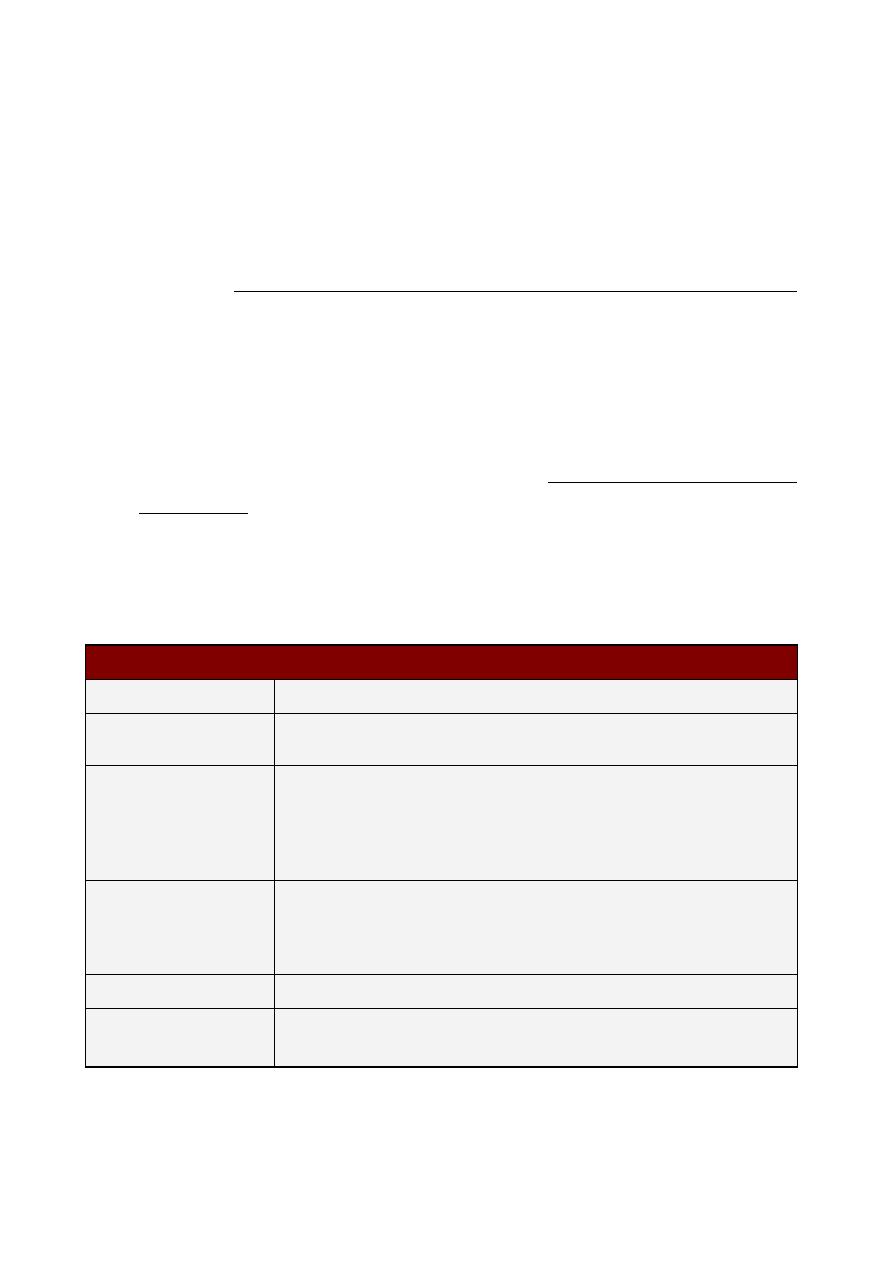
Complement deficiencies and diseases
Component
Disease
Mechanism
C1, C2, C4
SLE
Opsonization of immune complexes help
keep them soluble, deficiency results in
increased precipitation in tissues and
inflammation
Factors B or D
Susceptibility to
pyogenic (pus-
forming) bacterial
infections
Not enough opsonization of bacteria
C3
Susceptibility to
bacterial infections
Lack of opsonization and inability to utilize
the membrane attack pathway
C5, C6, C7
C8, and C9
Susceptibility to
Gram-negative
infections
Inability to attack the outer membrane of
Gram-negative bacteria
