Dr. Bushra
5th stageDefinition
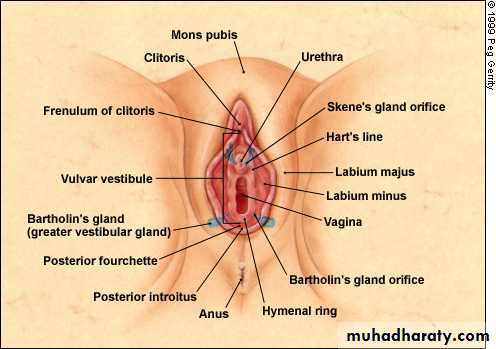
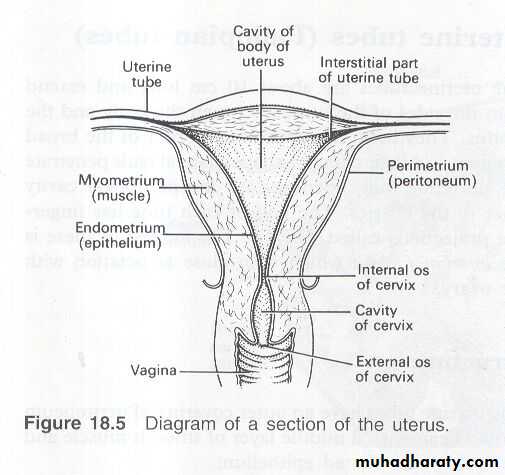
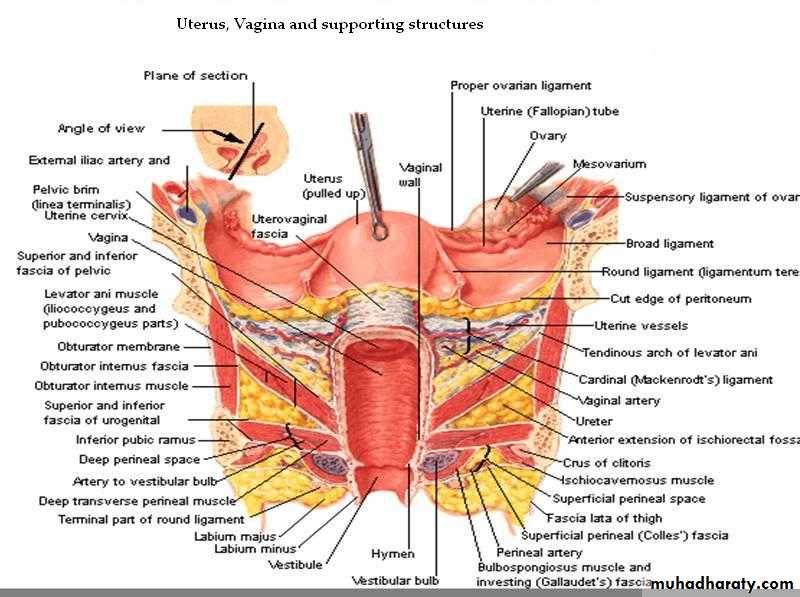
A fibromuscular tube which leads from the vulva to the uterus connecting the external and internal organs of reproduction in the femaleThe lowest part of internal genital tract.
Course
Runs obliquely upwards and backwards at 45 ° angle
Between the bladder and rectum,anus
Size
Anterior wall 7.5 cm ( 3 inches)
Posterior wall 9 cm
Cervix protrudes through the anterior wall
StructureOuter areolar tissue
Middle smooth muscle
Inner stratified squamous epithelium – ridges – rugae
No secretory glands – moisture from cervical secretions
Blood Supply
Arterial plexus – derived from the uterine and vaginal arteries - the branches of the internal iliac arteries
Venous plexus situated in the muscular wall, drains into the internal iliac veins
Lymph drainage
To the deep and superficial iliac glands
Nerve supply
Parasympathetic fibres from the sacral outflow
Sympathetic fibres from the lumbar outflow
Somatic sensory fibres from the pudendal nerves
Normal Vaginal Physiology
Normal vaginal discharge is usually white/transparent/thick/odorlessVaginal PH 4-4.5
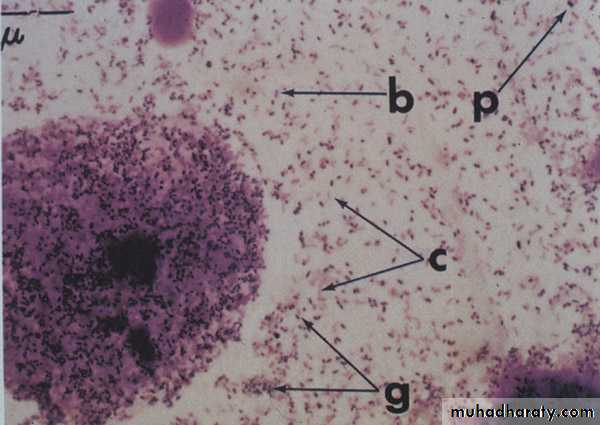
Microscopic examination:
predominantly squamous epithelial cells
rarely PMN’s (polymorphonuclear leukocytes)
Vaginal microbiology
Mainly lactobacillusDiphtheroids
S.epidermidis
Epidemiology
Vulvovaginal symptoms are extremely common,
The etiology of vaginal complaints includes infection of the vagina, cervix, and upper genital tract, and a number of non-infectious causes such as chemicals or irritants (e.g., spermicides or douching), hormone deficiency etc.
Symptoms : 1- Abnormal vaginal discharge 2- Pruritus 3-Irritation 4-Burning 5-Soreness 6-Odor 7-Dyspareunia 8-Bleeding 9-Dysuria
History of Vaginitis
Is there abdominal pain?.
Has there been exposure to a new sexual partner?
When did the symptoms start in relation to menses?
What medications (prescription and nonprescription) are being used?.
What are the patient's hygienic practices (e.g., daily use of pantyliners, feminine products)?
Abdominal pain is suggestive of PID and suprapubic pain is suggestive of cystitis
A new sexual partner increases the risk of acquiring STD or cervicitis r/t GC/CH
Candida vulvovaginitis often occurs in the premenstrual period, while trichomoniasis often occurs during or immediately after the menstrual period.
Antibiotics and high-estrogen contraceptives may predispose to candida vulvovaginitis; increased physiologic discharge can occur with estrogen-progestin contraceptives
pruritus unresponsive to antifungal agents suggests vulvar dermatitis
Bacterial Vaginitis (G Vaginalis)
Most common cause of vaginitis in women of childbearing age
Caused by decrease in hydrogen peroxide-producing lactobacilli and increase in Gardnerella vaginalisMay c/o Vaginal discharge usually thin white/grayish white & nonirritating , malodorous fishy odor (usually worse after unprotected intercourse.)
Risk Factors
Complications
Prevalence of 5-60% across the globe
Gardenerella is made up of different types of anaerobic gram negative rods
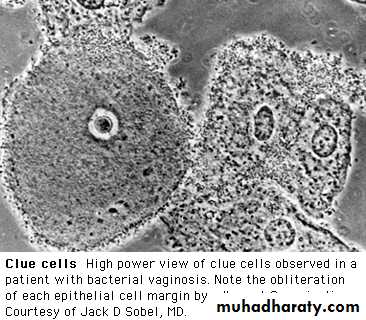
The lactobacilli compete against the other micro-organisms for adherence on the epithelial cell (Clue cells) ultimately changing the morphology of the cell.
BV (Gardenella)not considered STD however women who are not sexually active rarely get BV ODOR becomes worse after washing with soap or after coitus secondary to it the d/c becoming more alkaline
50% asymptomatic
RISK FACTORS:
having frequent sexual intercourse or more than one partner,
antibiotic use,
douching routinely,
fecal contamination into the vagina,
failure to clean sex toys
COMPLICATIONS:
Pregnant women have higher risk of preterm delivery,
post-partum fever,
post hysterectomy vaginal cuff cellulitis,
and post abortion infection
BV more common among women with PID (but studies inconclusive0
BV increases risk of HIV infection transmissionas long as the lactobacilli are there they control the situation, but if the lactobacilli begin to disappear Gardneralla increases, anaerobes increase, as a result of that the Gardnerella produces amino acids which the anaerobes have an enzyme that cleaves into amines. It's the amines that elevates the pH in the vagina, that cause the squamous cells to slough and desquamate and produce the discharge characteristic of the disease. And then what you get yourself into is this vicious cycle in which you've got an elevated pH which kills off more of the lactobacilli which then allows the anaerobes to grow to tremendously high levels
Bacterial vaginosis
Incidence: the most common 40%
Organism : Gardenrella vaginalis ( gram – ve coccobcilli )
Suitable PH : 5 – 5.5
Incubation period: 5 – 10 days
Symptoms : Discharge: thin , moderate in amount , grayish, frothy , characterized by fish odor specially after intercourse
Diagnosis
History and PE2- Amsel criteria
-Clue cells on wet mount
-Vaginal pH >4.5
-Fishy smell on addition 10%KoH
-Grayish-white discharge
Gram stain (3 out of 4 necessary for diagnosis (Amstel Criteria)
3- Whiff amine test (10% KOH added to vaginal D/C has fishy odor)
4-Vaginal culture has no role in the diagnosis of BV
TreatmentBacterial Vaginosis
Metronidazole 500mg BID X 7days or
Metronidazole 2g single dose
Metro gel .75% 1-application intravaginally qhs or BID X 5days
Clindamycin cream 2% 1-applicator (5g) intravaginally qhsX7d
Oral clindamycin 300mg BID X 7 Days
Cleocin has a new 3 day treatment w/vaginal supp (cleocin vaginal ovules)=clindamycin
Clindamycin cream appears less effective than metro regimens
Metronidazole (flagyl) 10% will experience metallic taste and nausea (2g sl. Less effective
Psuedomembranous colitis has been associated with clindamycin
If asymptomatic it may resolve on its own in a few months (in a study on asymptomatic patients end result no difference in cure rate, but few on metro developed vag. Candida
Relapse: approximately 30% of patients with initial response to therapy have a relapse of Sx w/in 3m (probably d/t failure to eradicate the offending organism / inability to reestablish normal flora (treat 10-14 days)
Vaginal candidiasis
Incidence: 25-50% of vaginal infectionOrganism : 58-90 % candia albicans
15 – 10% candial glabrata and tropicalis
Predisposing factor
Antibiotic.
Oral contraception .
Pregnancy.
Bad personal hygiene.
Partner infection .
Decreased immunity
* Suitable PH : < 4.5
* Mode of infection:
Flourishing due to predisposing factor.
Contamination (hands,towels,clothes)
Bath water
Sexual intercourse
Clinical picture symptoms
Signs
Signs of inflammation
Itching marks
A symptomatic in 50% of cases
Pruritus the most common , increases at night.
Discharge: white scanty thick odorless
( like cottage cheese)
Dysuria and dyspareumia.
Candidiasis (Candida albicans)
C/O intense vulvar pruritis & burning, white curd-like D/C, irritation, dyspareunia, vulvar erythema & edema may occur, as well as dysuria
Accounts for 1/3 of vaginitis cases
The infection is part of the host inflammatory response to the invasion of yeast
Multiple Causes/Risk Factors
1/3 of vaginitis cases – as many as ½ may be misdx because microscopy not always performed
75% of premenopausal women have reported having at least one episode
Rare before menarche, post-menopausal women less likely unless on HRT
Candidiasis:
may be seen in Pregnancy, DM, HIV, obesity Medications:OCP (higher the estrogen the greater the risk, corticosteroids, antibiotics (inhibition of normal bacterial flora by broad spectrum antibiotics favor yeast growth.
It is not considered sexually active, but sexual activity can also be a cause and seen more w/orogenital sex
Treatment of BV frequently causes Candidiasis.
1/3 of all vaginitis is caused by candida (since med OTC difficult to obtain true epidemiology)
At least 75% of women will have had this in there life time. And rare before menarche
DiagnosisPhysical Exam
pH 4-4.5
Wet mount with 10% KOH displays yeast buds and hyphae
Culture should be performed in persistent or recurrent symptoms
Treatment Options
Candidiasis
Azoles-vaginal preps(creams/suppostories/tablets) available in different strengths and length of use will vary
Fluconazole 150mg X1 orally
Ketoconzole 200mg orally BID X5days
Many available treatment options OTC. 1-7day treatments. Many women harbor yeast, so only treat if symptomatic.
Acidophilis/yogurt not proven to be effective
Oral Azoles are contraindicated in pregnancy, but topical treatments usually considered safe.
Recurrent candidiasis is considered =/>4 infections per year which occurs in8% of health women. Most prone are immunocompromized/diabetics (most a reinfected d/t relapse)
Treatment Good personal hygiene and usage of suitable vaginal wash.
Ketoconazol (Nizoral)
Fluconozol (diflucan)
Local povidone iodin – sunsola120
Adjuvant treatment (1% hydrocortisone)
Mycostatin (nystatin)
Topical imidazol
Tioconozol (gynotrosyd)
Clotrimozol (canestin – candistan)
Miconozol (gynodalctarin – gynozol)
Trichomonas (Trichomonas vaginalis)
Epidemiology
The organism is the flagellated protozoan trichomonas vaginalis found in the vagina, urethra, and paraurethral organs
Self limiting in men
Spermicidal agents may reduce the rate of transmission
Virtually always sexually transmitted
Epidemiology-180 million women worldwide and 2-3 million American women annually making it the 3rd most common cause of vaginitis. It accounts for 4-35% of vaginitis diagnosed in symptomatic women presenting in the primary care clinic
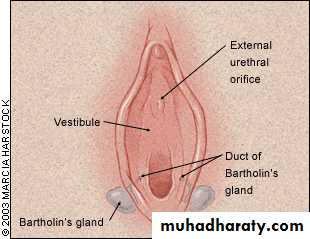
Trich infects the lower urinary tract in men and women. Infecting the vagina, urethra, parauethral organs as well cervix, Bartholins and Skene's glands.
Self limiting in men,however high rate of sexual transmission
Vaginal petichiae are the “strawberry spots
Incidence : 25% of vaginal infection
Causative organisms : Flagellated motile protozoon called trichomonas
Suitable PH : - 5.5 – 6.5.
* Mode of infection:
Sexual contact.
Contamination ( towel – Bath – clothes – instruments ).
Auto infection from GIT .
Clinical Manifestations
May be asymtomatic carrier to severe acute inflammatory dz.
Symptoms usually consistent with purulent, malodorous, thin discharge.
Usually c/o burning, pruritus, dysuria, frequency, and dysparenunia
Generalized inflammation may be present
Vaginal / cervical petechiae may occur
complications
Symptoms usually worse after menses/ during pregnancy
Pruritus may be severe or absent
10-30% may c/o yellow-green frothy d/c
Complications: Important in pregnancy women since associated with premature rupture of membranes, post-hysterectomy cellulitis, tubal infertility, increase in cervical neoplasm, also facilitates the transmission of HIV infection
Clinical Picture
Incubation period : 4 – 28 day
Symptoms :
Discharge : profuse , watery , yellowish , frothy , malodor
Soreness and dyspareunia .
Urinary symptoms.Pruritus
Diagnosis
History and focused physical examWet mount with NS reveals motile flagellates/ trichomonads
Increase Polymorphonuclear leukocytes on microscopy (PMN’s)
pH >4.5
Culture is the GOLD STANDARD
Fineberg-Whittington
Motile flagellates occurs 50-70% of the time (confirmed by culture confirmed cases)
Culture on Diamond’s medium has the highest sensitivity and specificity
Routine pap-smear will also pick up trich (60-70% of the time) w/up to 30% chance of false positive
Also available are rapid diagnostic kits using DNA probes (w/>90% S&S)
Complications **important in pregnancy. Increase the risk of premature rupture of membranes and premature birth, also associated with increased risk of post hysterectomy cellulitis, tubal infertility, and cervical neoplasm. Also facilitates the transmission of HIV infection
Unlike yeast infection H&P alone is not sufficient enough for treatment
Flagella in 50-70% and culture 95% sensitive
Treatment
Metronidazole * 2g single dose *500mg BID X7 days*2g cure rate 85-90%*500mg BID cure rate >90%
Precautions: Pregnancy-avoid treatment in the first trimester d/t teratogenicity (some providers still give it) and the CDC no longer discourages it in the first trimester
AVOID ETOH d/t (antabuse effect)
Bartholin’s Cyst and Abscess
An obstruction of the Bartholin’s gland resulting in retention of secretions and cystic dilatation
Gland is located deep in the posterior 3rd of both labia majora
Infection is often an important cause of obstruction. Clogged mucous or congenital narrowing of the duct may also be the cause.
In post menopausal patients enlargement of the gland must raise suspicion of CA and biopsy indicated
2% of women develop a bartholin cyst of abscess
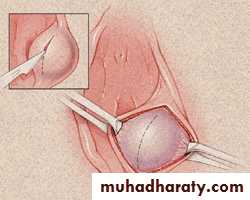
Marsupializationof Bartholin duct cyst. A vertical incision is made over the center of the cyst to dissect it free of mucosa. The cyst wall is everted and approximated to the edge of the vestibular mucosa with interrupted sutures
Bartholin glans: Tow in no. lie posteriolaterally to the vaginal orifice one each side ,normally not seen not felt, if enlarged could be painless cyst or painful abscess
Bartholin Duct Cyst
Most common Vulval cyst .
usually unilateral, on the posterio-lateral side of the introitus.
usually about 2 cm & contains sterile mucus.Usually asymptomatic.
secondary infections → Bartholin's abscess.
Rx: excision or Marsupializations
Bartholin's Abscess
Rx: drainage & Marsupialization
Atrophic Vaginitis
Definition and Incidence
Atrophic vaginitis, sometimes called vaginal atrophy, is a chronic progressive condition occurs mainly in postmenopausal women and is characterized by pale, thin, shining, shrunken and atrophic vaginal epithelium. In addition to vagina, the atrophic changes also affects the urinary tract because of their common embryologic origin.The condition develops slowly and it takes 5-10 years after menopause to manifest. Atrophic vaginitis affects 50-60% of postmenopausal women; of them only 25% seek medical advice. It may occur in women at childbearing period after delivery or with breastfeeding.
Etiology
1-Menpopause: due to lack of estrogen. Dramatic decline in the circulating estrogen levels occurs at menopause from 120 pg/ml to 18 pg/ml
2-Pelvic irradiation or chemotherapy
3-Oophorectomy
4-Anti-estrogns: e.g. Tamoxifen, Danazol, Medroxyprogesterone, GnRh agonists
5-Immediately after delivery or breast feeding
6-Anorexic women & women who have recently lost a significant body weight
6-idiopathic
Diagnosis
A combined approach is mandatory to reach a correct diagnosis of atrophic vaginitis. This approach consists of; 1) proper history taking with special emphasis on any contact irritant such as local perfumes or deodorants or lubricants, 2) physical examination and 3) laboratory testings.
Be careful to avoid the routine diagnosis of atrophic vaginitis in postmenopausal women with urogenital complaints.
Exclude other causes of vaginal infection such as bacterial vaginosis, candidiasis or trichomoniasis.
Diagnosis (Cont.)
I-History: of
-Frequency of urine, dysuria, nocturia, hematuria and incontinence.
-Malodorous thick yellowish discharge.
-Dyspareunia which may be followed by bleeding after intercourse.
-Vaginal soreness and itching
Diagnosis (Cont.)
II-Physical examination:
Vaginal examination should be performed using a small lubricated speculum to 1) avoid injury or bleeding from the atrophic vaginal tissues 2) minimize discomfort to the patient.
Examination reveals:
1- Stenotic introitus: width is less then 2 fingers
2- Decreased vaginal depth.
3- Pale dry vagina with friable epithelium which lacks normal mucosal rugae
4- Diminished or absent elasticity of vagina.
5-Minimal vaginal lubrication due to decreased vaginal blood flow.
6-Petechiae may be present on the vaginal lining.
7 -Vulvar tissue may appear diminished, obliterated, or even fused.
8 -Clitoral shrinkage
Diagnosis (Cont.)
III- Laboratory testing:
1-PH: Vaginal pH in atrophic vaginitis is more than 5 measured with pH indicator strip inserted into the proximal one-third of the vagina
2-Low level of circulating estrogen <25 pg/mL
3-Microscopy (wet mount): to rule out vaginitis due to bacterial vaginosis, candidiasis, and trichomoniasis
4-Cytology:
In a postmenopausal woman, due to lack of estrogen, a vaginal smear shows lack of maturation of vaginal cells (superficial cells < 30%) with predominance of intermediate, parabasal and metaplastic cells. These cells are characterized by the high nuclear cytoplasmic ratio, round nucleus, and basophilic cytoplasm. They are uniform in size and shape. Parabasal cells also may contain cytoplasmic vacuoles and are known as foam cells.
In premenopausal & younger woman, vaginal cells are mature. i.e superficial. The superficial cells are large cells with either a small round pyknotic nucleus or lack a nucleus if they are cornified. Cytoplasm is abundant and keratinized. Cell margins are angular with folded edges. They are a rich source of glycogen for the lactobacilli.
Complications
Bacterial or fungal vaginal infections
Cracks in the vaginal wall.
Dyspareunia and bleeding after intercourse
Treatment (Cont.)
1-Nonhormonal:
First-line therapy for women with vaginal atrophy includes non-hormonal water soluble vaginal lubricants and moisturizers. Women should also be encouraged to continue sexual activity.
2-Hormonal:
Bio-identical vaginal preparations are more effective than oral or transdermal preparations in releifing manifestations of atrophic vaginitis.
Bio-identical vaginal estrogen require lower doses than systemic therapy; and it is the treatment of choice for such women
Bio-identical vaginal estrogen therapy is available in many forms (creams, tablets, suppositories or rings). The best selection is the form that best suits an individual patient.
Treatment (Cont.)
Examples of bio-identical local vaginal estrogens::
1- Estriol vaginal cream: One gram is applied to the vagina nightly for 7-10 nights then the dosage is reduced to 2–3 times per week for long-term maintenance.
2 - Vagifem vaginal inserts: One insert is used in the vagina each night for 7–14 nights, and then reduced to one insert two nights per week for maintenance.
3- Estrace vaginal cream: 1 gram is applied to the vagina nightly for 7 -10 nights, then reduced to 1-3 times per week for long-term maintenance
4- Estring 90-day vaginal ring: 1 ring is inserted into the vagina and remains there for 90 days when it is removed & replaced with new ring.
Premarin Vaginal Cream which is commonly prescribed by many gynecologists is not a bio-identical estrogen. Biodentical local estrogen are either equal or superior to, premarine.
local bio-identical estrogens are always preferred to systemic estrogenic preparations. They improve atrophic vaginitis with minimal systemic absorption.
Systemic estrogen administration in standard doses does not necessarily improves symptoms of atrophic vaginitis; however, higher doses improves manifestations of atrophic vaginitis in a large proportion of women (close to 85%). In addition, it has the advantage of decreasing postmenopausal bone loss and control of vasomotor dysfunction.
Vaginal preparations improves symptoms and signs in 80% of women within 3 weeks of commencing therapy.
Long term treatment with vaginal estrogenic may improve bone density and lower total cholesterol level, low density lipoprotein and apolipoprotein. Such preparations are unlikely to have adverse effects on long term use.
Treatment should be continued till improvement occurs. Either continuous regimen or intermittent approach can be employed
Follow-up visits should include assessment of symptoms, vaginal morphology, and pH.
Patients at high risk for endometrial cancer, & those using a higher E dose or having vaginal spotting or breakthrough bleeding may require closer surveillance.
Women with hormone-dependent cancer are not ideal candidates for treatment with local E, but such women with severe symptoms not improved with conservative measures may be considered for E therapy
Side effects of local estrogen therapy
1-Breast discomfort
2-Vaginal bleeding
Both 1 and 2 are the commonest side effects
3-Endometrial proliferation
4-A slight increase in the risk of an estrogen-dependent neoplasm.
Contraindications of local estrogen
Unexplained vaginal bleeding
Pregnancy
Estrogen-sensitive tumors,
End-stage liver failure and
Past history of estrogen-related thromboembolization
Vaginal Intraepithelial Neoplasia (VaINExtremely uncommon (150 times < CIN).
70% associated with CIN (extension of the transformation zone into the vaginal fornices).
Predisposing factors: similar to those of CIN (HPV), but the age of VaIN is higher than CIN, diethylstilboesterol in utero (metaplastic transformation into the vagina), previous history of CIN), radiotherapy of CA cervix.
VaIN is graded 1-3 but is less invasive than CIN:
- VaIN1: mild dysplasia.
- VaIN2: moderate dysplasia.
- VaIN3: severe dysplasia.
Dx: V. smear, colposcopy, biopsy (even after hysterectomy).
Rx: low grade: observation. high grade: excision, 5-fluoroyracil, diathermy. Alternatively, Radiotherapy. )
Vaginal Carcinoma
Incidence: 1-2% of all gyn. Cancer.
Classification:1. primary: squamous (common, 85%), adenocarcinoma, clear cell adenocarcinoma (DES).
2. secondary: metastasis from the cervix, endometrium,…..others.
50% in the upper 3rd, 30% in lower 3rd & 19% in middle 3rd.
Posterior V. lesions more common than anterior & the anterior are more common than lateral lesions.
Spread: direct & lymphatic.
Vaginal Carcinoma Clinical Staging (F.I.G.O.):
Stage I: tumour confined to vagina.
Stage II : tumour invades paravaginal tissue but not to pelvic sidewall.
Stage III : tumour extends to pelvic sidewall.
Stage IV :
a) tumour invades mucosa of bladder or rectum and/or beyond the true pelvis.
b) Distant metastasis.
TREATMENT
Stage 1:
1. Tumour < 0.5 cm deep:
a. surgery: local excision or total vaginectomy with reconstruction.
b. radiotherapy.
2. Tumour > 0.5 cm deep: (a) wide vaginectomy, pelvic lymphadenectomy + reconstruction of vagina. (b) radiotherapy
stage 2: (a) radical vaginectomy, lymphadenectomy (b) radiotherapy
Stage 3: radiotherapy.