المرحلة الرابعة العدد5
باطنية د.فارس5\4\2018
المرحلة الرابعة العدد5
باطنية د.فارس
5\4\2018
تسلسل 71ِ
تسلسل 71ِ
INFECTION AND INFECTIOUS DISEASE
‘Infection’ is defined as the process of foreign organisms invading and multiplying in or on a host. In practice, the term is usually reserved for situations in which this results in harm, rather than an infectious agent simply colonizing the host without ill effect. Infectious diseases remain the main cause of morbidity and mortality in man, particularly in developing areas where they are associated with poverty and overcrowding.
In the developed world increasing prosperity, universal immunization and antibiotics have reduced the prevalence of infectious disease. However, antibiotic-resistant strains of microorganisms and diseases such as human immunodeficiency virus (HIV) infection, variant Creutzfeldt–Jakob disease (vCJD), avian influenza and pandemic H1N1 influenza have emerged. There is increased global mobility ,both enforced (as a result of war, civil unrest and natural disaster) and voluntary (for tourism and economic benefit).This has aided the spread of infectious disease and allowed previously localized pathogens such as dengue and West Nile virus to establish themselves across much wider territories An increase in the movement of livestock and animals has enabled the spread of zoonotic diseases like monkeypox,
while changes in farming and food-processing methods have contributed to an increase in the incidence of food- and water-borne diseases. Deteriorating social conditions in the inner city areas of our major conurbations have facilitated the resurgence of tuberculosis and other infections. Prisons and refugee camps, where large numbers of people are forced to live in close proximity, often in poor conditions, are providing a breeding ground for devastating epidemics of infectious disease. There are new concerns about the deliberate release of infectious agents such as smallpox or anthrax by terrorist groups or national governments.
In the developing world successes such as the eradication of smallpox have been balanced or outweighed by the new plagues. Infectious diseases cause nearly 25% of all human deaths, rising to more than 50% in low income countries. Two billion people – one-third of the world’s population – are infected with tuberculosis (TB), up to 400 million people catch malaria every year and 200 million are infected with schistosomiasis. Some 500 million people are chronically infected with a hepatitis virus (either HBV or HCV) and 34 million people are living with HIV/AIDS, with 2.6 million new HIV infections in 2008 (65% in sub-Saharan Africa). Infections are often multiple and there is synergy both between different infections and between infection and other factors such as malnutrition. Many of the infectious diseases affecting developing countries are preventable or treatable, but continue to thrive owing to lack of money and political will.
Infectious agents
The causative agents of infectious diseases can be divided into four groups:
Prions are the most recently recognized and the simplest infectious agents, consisting of a single protein molecule. They contain no nucleic acid and therefore no genetic information: their ability to propagate within a host relies on inducing the conversion of endogenous prion protein PrPc into an abnormal protease-resistant isoform referred to as PrPSc.
Viruses contain both protein and nucleic acid and so carry the genetic information for their own reproduction. However, they lack the apparatus to replicate autonomously, relying instead on ‘hijacking’ the cellular machinery of the host. They are small (usually less than 250 nanometres (nm) in diameter) and each virus possesses only one species of nucleic acid (either RNA or DNA).
Bacteria are usually, though not always, larger than viruses. Unlike the latter they have both DNA and RNA, with the genome encoded by DNA. They are enclosed by a cell membrane and even bacteria which have adopted an intracellular existence remain enclosed within their own cell wall. Bacteria are capable of fully autonomous reproduction and the majority are not dependent on host cells.
Eukaryotes are the most sophisticated infectious organisms, displaying subcellular compartmentalization. Different cellular functions are restricted to specific organelles, e.g.photosynthesis takes place in the chloroplasts, DNA transcription in the nucleus and respiration in the mitochondria. Eukaryotic pathogens include unicellular protozoa, fungi (which can be unicellular or filamentous) and multicellular parasitic worms.
Routes of transmission
Endogenous infection
The body’s own endogenous flora can cause infection if the organism gains access to an inappropriate area of the body. This can happen by simple mechanical transfer, e.g. colonic bacteria entering the female urinary tract. The nonspecific host defences may be breached, for example, by cutting or scratching the skin and allowing surface commensals to gain access to deeper tissues; this is frequently the aetiology of cellulitis. There may be more serious defects in host immunity owing to disease or chemotherapy, allowing normally harmless skin and bowel flora to produce invasive disease.
Air-borne spread
Many respiratory tract pathogens are spread from person to person by aerosol or droplet transmission. Secretions containing the infectious agent are coughed, sneezed or breathed out and are then inhaled by a new victim. Some enteric viral infections may also be spread by aerosols of faeces or vomit. Environmental pathogens such as Legionella pneumophila and zoonoses such as psittacosis, are also acquired by aerosol inhalation, while rabies virus may be inhaled in the dust from bat droppings.
Faeco-oral spread
Transmission of organisms by the faeco-oral route can occur by direct transfer (usually in small children), by contamination of clothing or household items (usually in institutions or conditions of poor hygiene) or most commonly via contaminated food or water. Human and animal faecal pathogens can get into the food supply at any stage. Raw sewage is used as fertilizer in many parts of the world, contaminating growing vegetables and fruit. Poor personal hygiene can result in contamination during production, packaging, preparation, or serving of foodstuffs. In the western world, the centralization of food supply and increased processing of food has allowed
the potential for relatively minor episodes of contamination to cause widely disseminated outbreaks of food-borne infection.
Water-borne faeco-oral spread is usually the result of inadequate access to clean water and safe sewage disposal and is common throughout the developing world. Worldwide, 1.1 billion people have no access to clean water and 2.6 billion do not have basic sanitation.
Vector-borne disease
Many tropical infections, including malaria, are spread from person to person or from animal to person by an arthropod vector. Vector-borne diseases are also found in temperate climates, but are relatively uncommon. In most cases part of the parasite life cycle takes place within the body of the arthropod and each parasite species requires a specific vector. Simple mechanical transfer of infective organisms from one host to another can occur, but is rare.
Direct person-to-person spread
Organisms can be passed on directly in a number of ways. Sexually transmitted infections are examples ,Skin infections such as ringworm, and ectoparasites such as scabies and head lice, can be spread by simple skin-to-skin contact. Other organisms are passed on by blood- (or occasionally other body fluid) to-blood transmission. Blood-to blood transmission can occur during sexual contact, from mother to infant either transplacentally or in the peripartum, between intravenous drug users sharing any part of their injecting equipment, when infected medical or other (e.g. tattoo needles) equipment is reused, if contaminated blood or blood products are transfused, or in any sporting or accidental contact when blood is spilled. Ingestion of infected breast milk is another route of person-to-person spread for some infections (e.g. HIV).
Direct inoculation
Infection can occur when pathogenic organisms breach the normal mechanical defences by direct inoculation. Some of the circumstances in which this can occur are covered under endogenous infection and blood-to-blood transmission above. Some environmental organisms may be inoculated by accident: this is a common mode of transmission of tetanus and certain fungal infections. Rabies virus may be inoculated by the bite of an infected animal.
Consumption of infected material
Although many food-related zoonotic infections are due to contamination of food with animal faeces (and are thus, strictly speaking, faeco-oral), several diseases are transmitted directly in animal products. These include some strains of Salmonella (eggs, chicken meat), brucellosis (unpasteurized milk) E. coli and the prion diseases kuru and vCJD (neural tissue).
VIRAL INFECTIONS
DNA VIRUSES
Adenoviruses
Over 50 adenovirus serotypes have been identified as human pathogens, infecting a number of different cell types and therefore resulting in different clinical syndromes. Adenovirus infection commonly presents as an acute pharyngitis and extension of infection to the larynx and trachea in infants may lead to croup. By school age the majority of children show serological evidence of previous infection. Certain subtypes produce an acute conjunctivitis associated with pharyngitis.In adults, adenovirus causes acute follicular conjunctivitis and rarely pneumonia that is clinically similar to that produced by Mycoplasma pneumoniae , Certain adenoviruses cause gastroenteritis . without respiratory disease and adenovirus infection may be responsible for acute mesenteric lymphadenitis in children and young adults. Mesenteric adenitis due to adenoviruses may lead to intussusception in infants. Infection in an immunocompromised host, e.g. a bone marrow transplant recipient, may result in multisystem failure and fatal disease.
Herpesviruses
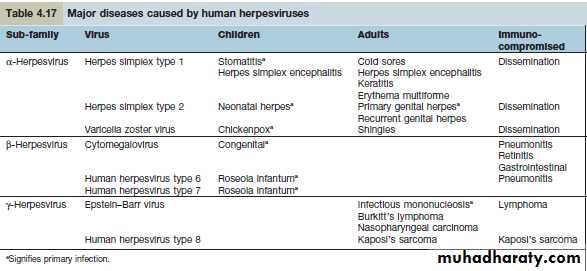
Members of the Herpesviridae family are causes of a wide range of human diseases. Details are summarized in Table 4.17. The hallmark of all herpesvirus infections is the abilityof the viruses to establish latent (or silent) infections that then persist for the life of the individual.
Herpes simplex virus (HSV) infection
Two types of HSV have been identified: HSV-1 is the major cause of herpetic stomatitis, herpes labialis (‘cold sore’), keratoconjunctivitis and encephalitis, whereas HSV-2 causes genital herpes and may also be responsible for systemic infection in the immunocompromised host. These divisions, however, are not rigid, for HSV-1 can give rise to genital herpes and HSV-2 can cause infections in the mouth.HSV-1
The portal of entry of HSV-1 infection is usually via the mouth or occasionally the skin. The primary infection may go unnoticed or may produce a severe inflammatory reaction with vesicle formation leading to painful ulcers (gingivostomatitis). The virus then remains latent, most commonly in the trigeminal ganglia, but may be reactivated by stress, trauma, febrile illnesses and ultraviolet radiation, producing the recurrent form of the disease known as herpes labialis (‘cold sore’). Approximately 70% of the population is infected with HSV-1 and recurrent infections occur in one-third of individuals. Reactivation often produces localized paraesthesiae in the lip before the appearance of a cold sore. Complications of HSV-1 infection include transfer to the eye (dendritic ulceration, keratitis), acute encephalitis , skin infections such as herpetic whitlow and erythema multiforme .
HSV-2
The virus remains latent in the sacral ganglia and during recurrence, can produce a radiculomyelopathy, with pain in the groin, buttocks and upper thighs. Primary anorectal herpes infection is common in men having sex with men. The clinical picture, diagnosis and treatment of genital herpes .
Neonates may develop primary HSV infection following vaginal delivery in the presence of active genital HSV infection in the mother, particularly if the maternal disease is a primary, rather than a recurrent infection. The disease in the baby varies from localized skin lesions (about 10–15%) to widespread visceral disease often with encephalitis, with a poor prognosis. Caesarean section should therefore be performed if active genital HSV infection is present during labour.
Immunocompromised patients such as those receiving intensive cancer chemotherapy or those with the acquired immunodeficiency syndrome (AIDS) may develop disseminated HSV infection involving many of the viscera. In severe cases, death may result from hepatitis and encephalitis. Eczema herpeticum is a serious complication in individuals with eczema, where the non-intact skin allows spread of lesions across large areas and bloodstream access which may lead to herpetic involvement of internal organs. Humoral antibody develops following primary infection, but mononuclear cell responses probably prevent dissemination of disease.
Varicella zoster virus (VZV) infection
VZV produces two distinct diseases, varicella (chickenpox) and herpes zoster (shingles). The primary infection is chickenpox. It usually occurs in childhood, the virus entering through the mucosa of the upper respiratory tract. In some countries (e.g. the Indian subcontinent), a different epidemiological pattern exists with most infections occurring in adulthood. Chickenpox rarely occurs twice in the same individual. Infectious virus is spread from the throat and from fresh skin lesions by air-borne transmission or direct contact. The period of infectivity in chickenpox extends from 2 days before the appearance of the rash until the skin lesions are all at the crusting stage. Following recovery from chickenpox, the virus remains latent in dorsal root and cranial nerve ganglia. Reactivation of infection then results in shingles.
Clinical features of chickenpox
Some 14–21 days after exposure to VZV, a brief prodromal illness of fever, headache and malaise heralds the eruption of chickenpox, characterized by the rapid progression of macules to papules to vesicles to pustules in a matter of hours . In young children, the prodromal illness may be very mild or absent. The illness tends to be more severein older children and can be debilitating in adults. The lesions occur on the face, scalp and trunk and to a lesser extent, on the extremities. It is characteristic to see skin lesions at all stages of development on the same area of skin. Fever subsides as soon as new lesions cease to appear. Eventually the pustules crust and heal without scarring.Complications of chickenpox include pneumonia, which generally begins 1–6 days after the skin eruption, and bacterial superinfection of skin lesions. Pneumonia is more common in adults than in children and cigarette smokers are at particular risk. Pulmonary symptoms are usually more striking than the physical findings, although a chest radiograph usually shows diffuse changes throughout both lung fields.
CNS involvement occurs in about 1 per 1000 cases and most commonly presents as an acute truncal cerebellar ataxia. The immunocompromised are susceptible to disseminated infection with multiorgan involvement. Women in pregnancy are prone to severe chickenpox and, in addition, there is a risk of intrauterine infection with structural damage to the fetus (if maternal infection is within the first 20 weeks of pregnancy, the risk of varicella embryopathy is 1–2%).
Clinical features of shingles
Shingles arises from the reactivation of virus latent within the dorsal root or cranial nerve ganglia. It may occur at all ages but is most common in the elderly, producing skin lesions similar to chickenpox, although classically they are unilateral and restricted to a sensory nerve (i.e. dermatomal) distribution . The onset of the rash of shingles is usually preceded by severe dermatomal pain, indicating the involvement of sensory nerves in its pathogenesis. Virus is disseminated from freshly formed vesicles and
may cause chickenpox in susceptible contacts. The commonest complication of shingles is post-herpetic neuralgia (PHN) .
Diagnosis
The diseases are usually recognized clinically but can be confirmed by detection of VZV DNA within vesicular fluid using PCR, electron microscopy, immunofluorescence or culture of vesicular fluid and by serology.
Prophylaxis and treatment
Chickenpox usually requires no treatment in healthy children and infection results in lifelong immunity. Aciclovir and derivatives are, however, licensed for this indication in the USA, where the argument for treatment is one of health economics,viz. the sooner the child recovers, the sooner the carer can return to work. However, the disease may be fatal in the immunocompromised, who should therefore be offered protection, after exposure to the virus, with zoster-immune globulin (ZIG) and high-dose aciclovir at the first sign of development of the disease.
Anyone with chickenpox who is over the age of 16 years should be given antiviral therapy with aciclovir or a similar drug, if they present within 72 h of onset. Prophylactic ZIG is recommended for susceptible pregnant women exposed to varicella zoster virus and, if chickenpox develops, acyclovir treatment should be given (NB: aciclovir has not been licensed for use in pregnant women). If a woman has chickenpox at term, her baby should be protected by ZIG if delivery occurs within 7 days of the onset of the mother’s rash. An effective live attenuated varicella vaccine is licensed as a routine vaccination of childhood in the USA; it is available on a named-patient basis in the UK and also for susceptible healthcare workers.
Shingles involving motor nerves, e.g. 7th cranial nerve leading to facial palsy, is also treated with aciclovir (or derivatives thereof) as the duration of lesion formation and time to healing can be reduced by early treatment. Aciclovir, valaciclovir and famciclovir have all been shown to reduce the burden of post-herpetic neuralgia when treatment is given in the acute phase. Shingles involving the ophthalmic division of the trigeminal nerve has an associated 50% incidence of acute and chronic ophthalmic complications. Early treatment with aciclovir reduces this to 20% or less. As for chickenpox,
all immunocompromised individuals should be given acyclovir at the onset of shingles, no matter how mild the attack appears when it first presents. Vaccination of all adults over the age of 60, with a dose higher than that used for chickenpox prophylaxis in childhood, reduces shingles-related morbidity and post-herpetic neuralgia and is recommended for all people in the USA.