The Temporomandibular joint disorders
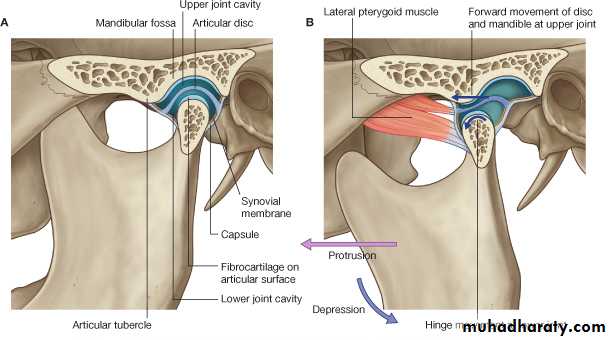
• The TMJ is a synovial bilateral joint that permits the mandible to move as a unit with 2 functional patterns ( hinge and translatory (gliding) movements).Normal anatomy
The basic components of the TMJ include:
• The mandibular component, i.e. the head of the condyle
• The disc
• The temporal component, i.e. the glenoid fossa and articular eminence
• The capsule surrounding the joint.
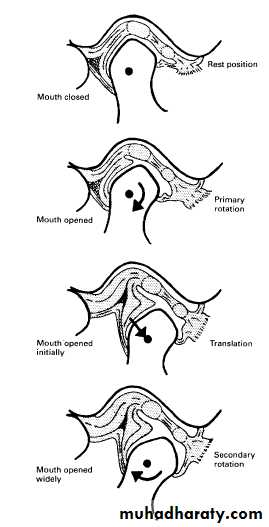
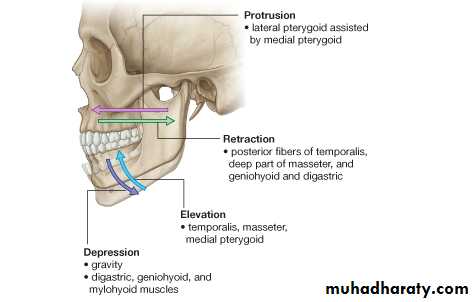
The normal movements include:
• Hinge or rotation of the condyle within the fossa.
• Translation movement of the condyle down the articular eminence. The disc being attached to the condyle also moves
forwards.
These two movements together result in the downward and forward movement of the condyles when patients open their mouths.
Diagrams showing the rotary and translatory movements of the condyle during normal mouth opening.
• Mouth closed
Mouth openA
B
C
D
Sagittal Reformat CBCT Image. A to C, Closed position. A, Lateral image slice.B, Central image slice. C, Medial image slice of the same joint. Notice that the condyle appears retruded in the lateral slice, centered in the central slice, and anteriorly positioned in the medial slice. D, Open view showing the degree of condyle translation during mandibular opening.
• Disorders of the TMJ
• TMJ myofascial pain dysfunction syndrome (MPDS)• Internal derangements
• Osteoarthritis (osteoarthrosis)
• Rheumatoid arthritis
• Juvenile rheumatoid arthritis (Still's disease)
• Ankylosis
• Tumours
• Fractures and trauma
• Developmental anomalies:
1- Condylar Hyperplasia
2- Condylar Hypoplasia
3- Juvenile Arthrosis
4- Coronoid Hyperplasia
5- Bifid Condyle
TMJ myofascial pain dysfunction syndrome (MPDS):
• This is the most common clinical diagnosis applied to patients with:
• Pain in the muscles of mastication, often worst in the early morning and evening , with occasional clicking and stiffness.
The etiology : anxiety or depression, malocclusion, or muscle spasm.
Main radiographic features:
• Normal condylar head shape and articular surface.• Normal glenoid fossa shape.
• Possible increase or reduction in the overall size of the joint space ( an increase in the size of the joint space is only indicative of
Inflammation).
• Possible displacement of the condylar head anteriorly or posteriorly in the glenoid fossa when the mouth is closed and the teeth are in
occlusion
• Reduction in the range of condylar movement.
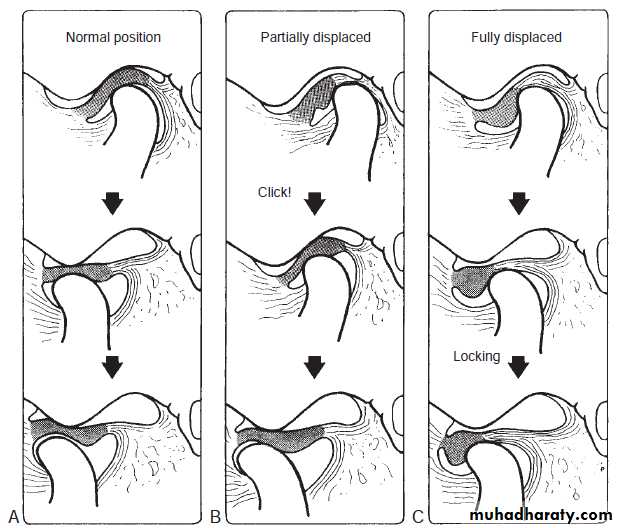
Internal Derangements :
• Abnormality in the position and sometimes the morphology of the articular disc that may interfere with normal function.• Unknown cause (or due to parafunction, direct trauma, and
forced opening beyond the normal range).
• The disc most often is displaced in an anterior direction, but it may be displaced anteromedially, medially, or anterolaterally. Lateral and posterior displacements are rare.
• The disc may resume a normal position with respect to the condyle (called reduction of the disc) during mandibular opening; when the disc remains displaced throughout the entire range of mandibular movement, the term non reduction is used.
• A longstanding displaced disc may become deformed, losing its normal
biconcave shape, and it may become thickened and fibrotic.
• Complications are degenerative joint disease and perforation through
the disc or (more commonly) the posterior attachment.
- Internal derangements can be diagnosed by MRI
Position and movement of the disc during jaw opening.
Normal position (A), mildly displaced anteriorly (with reduction , B ), and severely displaced anteriorly (without reduction, C ).Symptoms include:
• Clicking which may be painful.• Pain from the joint and/or musculature.
• Trismus and hesitation of movement and locking usually
with failure of opening.
• Conventional radiography may have revealed an alteration in the position of the head of the condyle, implying an abnormality in disc position.
MRI is the investigation of choice to show:
• Disc position — it may dislocate anteriorly or anteromedially
• Disc movement relative to the condyle during opening and closing.
Osteoarthritis:
• This degenerative arthrosis increases with age.• Causes pain in the stress bearing joints, such as the hips and spine.
Symptoms:include painful crepitus and trismus which are usually persistent.
Main radiographic features
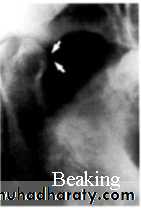
• Osteophyte (lipping) formation on the anterior aspect of the articular surface of the condylar head. Extensive osteophyte formation is referred to as beaking. Flattening of the head of the condyle on the anterosuperior margin .
• Subchondral sclerosis of the condylar head which becomes dense and more radiopaque-a process .
• A normal outline to the glenoid fossa though it may also become sclerotic.
Beaking
flatteningRheumatoid arthritis
• Is a generalized, chronic inflammatory, connective tissue disease affecting many joints.
Main radiographic features:
• Flattening of the head of the condyle.
• Erosion and destruction of the articular surface of the head of the condyle which may be extensive causing the outline to become irregular.
• Occasional osteophyte formation on the condyle.
• Hollowing of the glenoid fossa.
• Reduction in the range of movement.
• Features are usually bilateral and fairly symmetrical.
Juvenile Arthrosis:
• Manifests as condylar hypoplasia and characteristic morphologic abnormalities.• It affects children and adolescents during the growth of mandible.
• More common in females.
• Incidental finding in a panoramic projection.
Radiographic appearance:
• Condylar head develops a characteristic “toadstool” appearance.
• Condylar neck is shortened or even absent in some cases
Treatment: orthognathic surgery
orthodontic therapy
The condylar heads have a toadstool appearance & are posteriorly inclined. The condylar necks are absent.
Ankylosis:
True ankylosis: fusion of the bony elements of the joint .Causes:
• Trauma, particularly condylar head fractures and birth injury, and bleeding into the joint.
• Infection
• Severe juvenile rheumatoid arthritis.
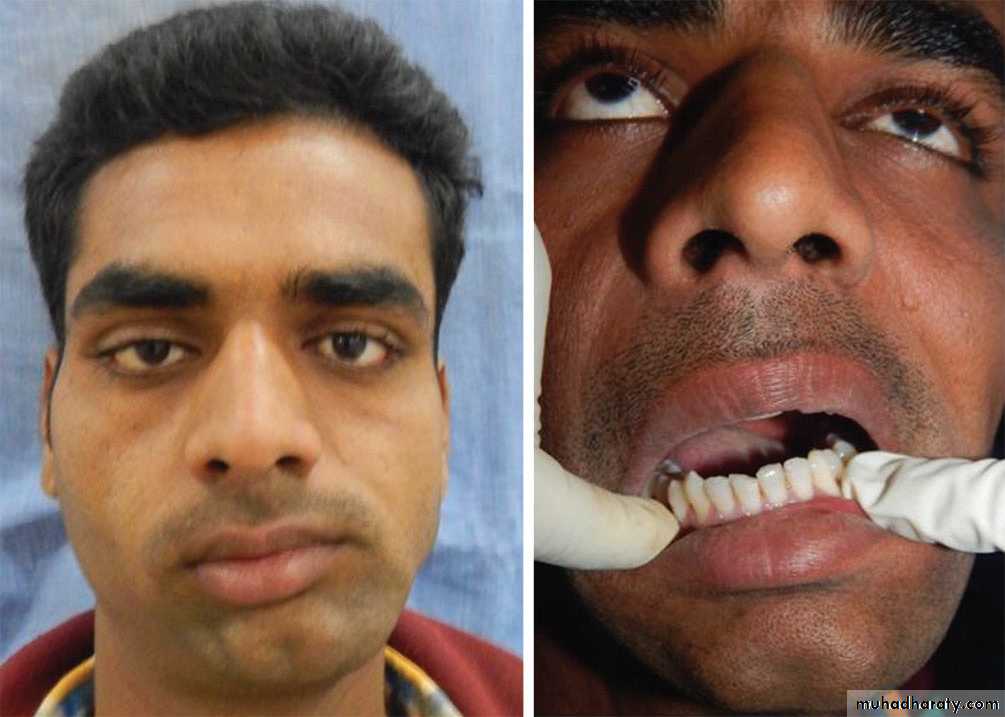
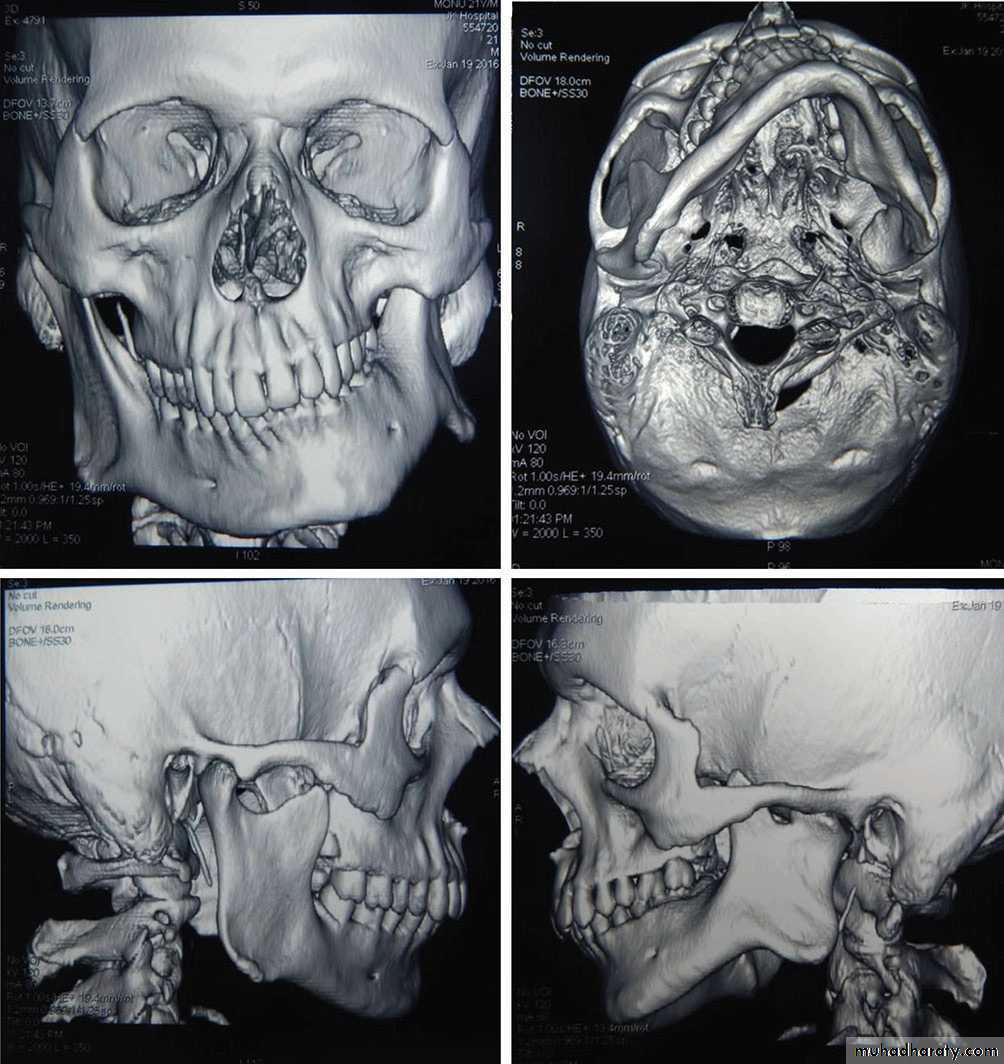
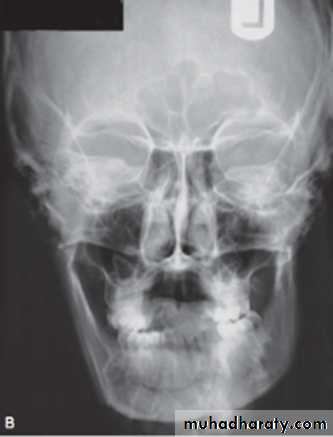
Main radiographic features
• Little or no evidence of a joint space.
• Bony fusion between the head of the condyle and the glenoid fossa with total loss of the normal anatomical outlines.
• Associated evidence of condylar neck hypoplasia and mandibular underdevelopment on the affected side producing asymmetry.
Tumours:
• Benign or malignant tumors affect the head of the condyle.• either intrinsic or extrinsic.
• Intrinsic develops in condyle, temporal bone or coronoid process.
• Extrinsic tumor may affect the morphology, structure and function of the joint without invading the joint itself.
Benign Tumors:
Osteoma, osteochondroma, Langerhans histocytosis and osteoblastomas,Chondroblastomas, fibromyxomas, benign giant cell lesions and anneurysmal bone cysts.
Benign tumors and cysts of the mandible may involve the entire ramus and condyle
Grow slowly, TMJ swelling ,Pain and decrease in range of motion.
While tumors of coronoid process are painless but may complain of progressive limitation of motion.
* Radiographic Features:
Condylar enlargement with irregular outline.Osteoma and osteochondroma appear as abnormal, pedunculated mass attached to the condyle.
• Treatment: Surgical excision of tumor and occasionally excision of condylar head or coronoid process.
• Malignant Tumors:(black arrows)
• A- Primary (rare): - Intrinsic
• - Extrinsic
• Intrinsic: Chondrosarcoma
• Osteogenic sarcoma
• Synovial sarcoma
• Fibrosarcoma
• Extrinsic: Direct extension of adjacent parotid salivary gland malignancies.
•
B. Metastatic (more common)
May be asymptomatic or patients may have symptoms of TMJ dysfunction (pain, limited mandibular opening, mandibular deviation and swelling)* Radiographic Features:
Variant degree of bone destruction with ill defined, irregular margins
CT modality of choice
MRI useful for displaying extent of involvement into surrounding tissues.
* Treatment:
Surgical removal of tumor.
May include radiotherapy and chemotherapy.
Fractures and trauma:
Fractures of the condylar necks are common after a blow to the chin .With this type of injury the condylar neck does not fracture but the head of the condyle either fractures, a so-called intra-capsular fracture ,or is forced upwards, through the glenoid fossa into the middle cranial fossa .
CT will demonstrate the extent of any injury. Trauma can also result in unilateral or bilateral dislocation .
OPG: showing bilateral dislocation of the
condyles (open arrows) out of the glenoid fossae (white arrows).Developmental anomalies:
1- Condylar Hyperplasia:- Enlargement and deformity of the condylar head.
- Secondary effect on the mandibular fossa as it remodels to accommodate the abnormal condyle.
Etiology: Trauma, infection, hereditary
More common in males.
Self limiting.
Progresses slowly or rapidly.
Mandibular asymmetry.
Chin deviated to the unaffected side.
Radiographic Features:
• May appear normal but symmetrically enlarged or it may be altered in shape (e.g., conical, spherical, elongated, lobulated)or irregular in outline.
• May be more radiopaque due to additional bone present.
• Condylar head & neck may be elongated with a compensating
forward bend, forming an inverted L.
• Glenoid fossa may also be enlarged.
• Ramus and mandibular body on the affected side also may be enlarged, resulting in a characteristic depression of the inferior mandibular border, increased vertical dimension of ramus and may be thicker in the anteroposterior dimension.
Treatment:
Orthodontics combined with orthognathic surgery.
2- Condylar Hypoplasia
• Failure of the condyle to attain normal size because of congenital and developmental abnormalities or acquired diseases that affect condylar growth.• The condyle is small, but condylar morphology is normal.
• Underdeveloped ramus and occasionally mandibular body.
• Unilateral or bilateral.
Radiographic Features:
• The condylar neck and coronoid process usually are very slender and are shortened or elongated in some cases.
• The ramus and mandibular body on the affected side may also be small, resulting in a mandibular asymmetry and occasional dental crowding, depending on the severity of mandibular underdevelopment.
Treatment: Orthognathic surgery.
Bone grafts.
Orthodontic therapy maybe required.
3- Coronoid Hyperplasia:
- Acquired or developmental- Elongation of the coronoid process
- Developmental > bilateral.
Acquired > uni or bilateral.
-Inability to open mouth.
-Painless.
Radiographic features:
• TMJs usually appear normal
• Unilateral cases should be
differentiated from a tumor of the
coronoid process (osteochondroma or osteoma)
• Unlike coronoid hyperplasia, tumors have an irregular shape
• Treatment: surgical removal or the coronoid process and postoperative physiotherapy
Sagittal CT. Elongated coronoid process extends above the inferior rim of the zygomatic arch (arrow)
with normal shaped .
4- Bifid Condyle:
• Vertical depression, notch, or deep cleft in the center of the condylar head.
• Rare, often unilateral
• Incidental finding
• Some patients may have sings of TMDs (noises + pain)
Radiographic Features:
Depression on the superior condylar surface giving a heart shape