FLAPS FOR RECONSTRUCTIVE SURGERY
In current reconstructive therapy, bone grafts, membranes, or a combination of these, with or without other agents, are used for a successful outcome. The flap design should therefore be set up so that the maximum amount of gingival tissue and papilla are retained to cover the material(s) placed in the pocket.Two flap designs are available for reconstructive surgery: the
papilla preservation flap and
conventional flap with only crevicular incisions.
The flap design of choice is the papilla preservation flap, which retains the entire papilla covering the lesion. However, to use this flap, there must be adequate interdental space to allow the intact papilla to be reflected with the facial or lingual/palatal flap.
When the interdental space is very narrow, making it impossible to perform a papilla preservation flap, a conventional flap with only crevicular incisions is made.
Papilla Preservation Flap
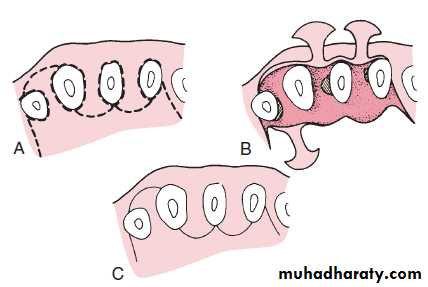
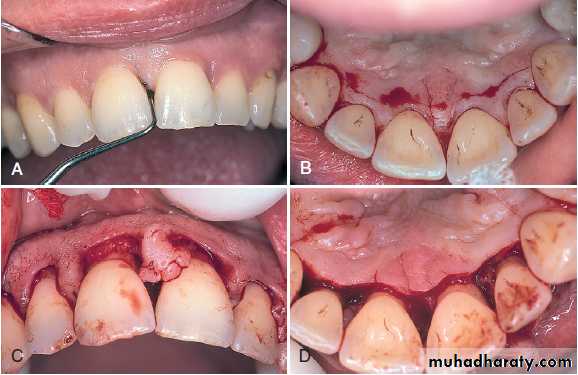
Step 1: A crevicular incision is made around each tooth with no incisions across the interdental papilla.Step 2: The preserved papilla can be incorporated into the facial or lingual/palatal flap, although it is most often integrated into the facial flap. In these cases, the lingual or palatal incision consists of a semilunar incision across the interdental papilla in its palatal or lingual aspect; this incision dips apically from the line angles of the tooth so that the papillary incision is at least 5 mm from the crest of the papilla.
Step 3: An Orban knife is then introduced into this incision to sever half to two-thirds the base of the interdental papilla. The papilla is then dissected from the lingual or palatal aspect and elevated intact with the facial flap.
Step 4: The flap is reflected without thinning the tissue.
Papilla preservation flap. A, Facial view after sulcular incisions have been made. B, Straight-line incision in the palatal area about 3 mm from gingival margins. This incision is then connected to the margins with vertical incisions in the midpart of each tooth. C, Papillae are reflected with the facial flap. D, Lingual view after reflection of the flap.
DISTAL MOLAR SURGERY
Treatment of periodontal pockets on the distal surface of terminal molars is often complicated by the presence of bulbous fibrous tissue over the maxillary tuberosity or prominent retromolar pads in the mandible. Deep vertical defects are also often present in conjunction with the redundant fibrous tissue. Some of these osseous lesions may result from incomplete repair after the extraction of impacted third molars .The gingivectomy incision is the most direct approach in treating distal pockets that have adequate attached gingiva and no osseous lesions. However, the flap approach is less traumatic postsurgically because it produces a primary closure wound rather than the open secondary wound left by a gingivectomy incision.
Technique
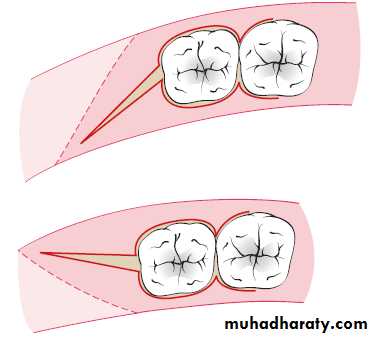
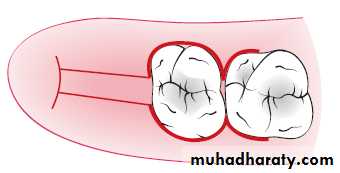
The two incisions distal to the molar should follow the area with the greatest amount of attached gingiva. Therefore the incisions could be directed distolingually or distobuccally, depending on which area has more attached gingiva. Before the flap is completely reflected, it is thinned with a #15 blade. After the reflection of the flap and the removal of the redundant fibrous tissue, any necessary osseous surgery is performed. Then flaps are approximatedUpper
LowerFlap design
Periodontal Plastic
and Esthetic Surgery
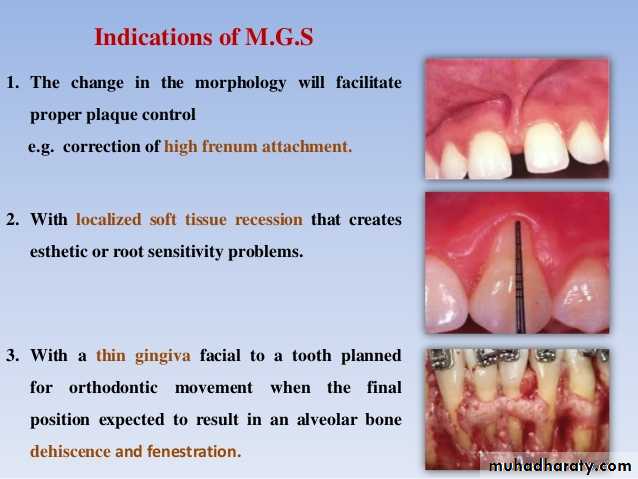
(Mucogingival Surgery)The term mucogingival surgery was initially introduced to describe surgical procedures for the correction of relationships between the gingiva and the oral mucous membrane with reference to three specific problem areas:
- attached gingiva,
- shallow vestibules, and
- frenum interfering with the marginal gingiva.
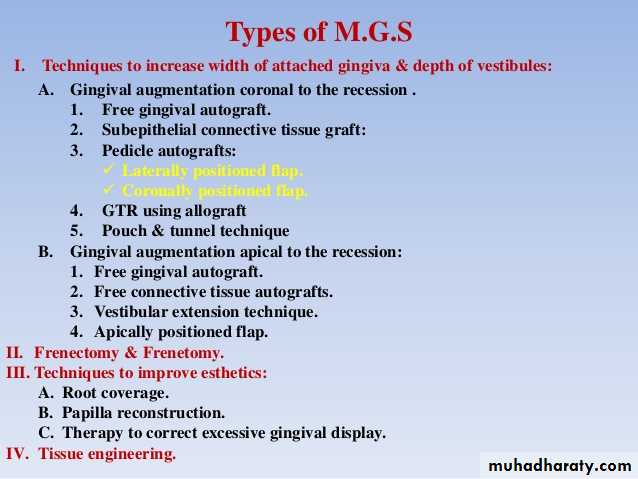
Periodontal plastic surgery is defined as the surgical procedures performed to correct or eliminate anatomic, developmental, or traumatic deformities of the gingiva or alveolar mucosa. Mucogingival therapy is a broader term that includes nonsurgical procedures such as papilla reconstruction by means of orthodontic or restorative therapy. Periodontal plastic surgery includes only the surgical procedures of mucogingival therapy.
OBJECTIVES
The five objectives of periodontal plastic surgery are as follows:1. Problems associated with attached gingiva
2. Problems associated with a shallow vestibule
3. Problems associated with an aberrant frenum
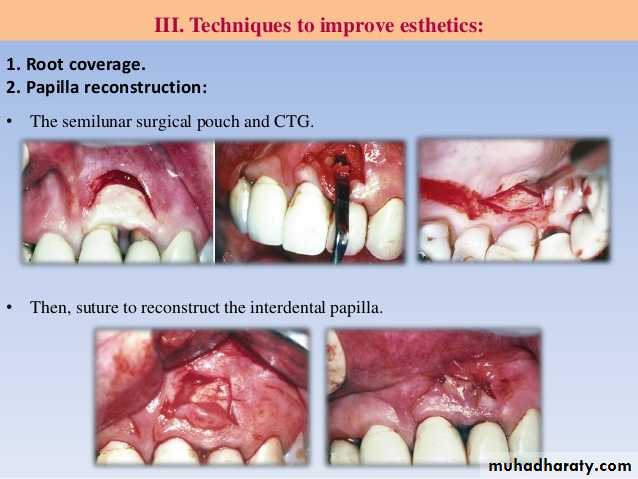
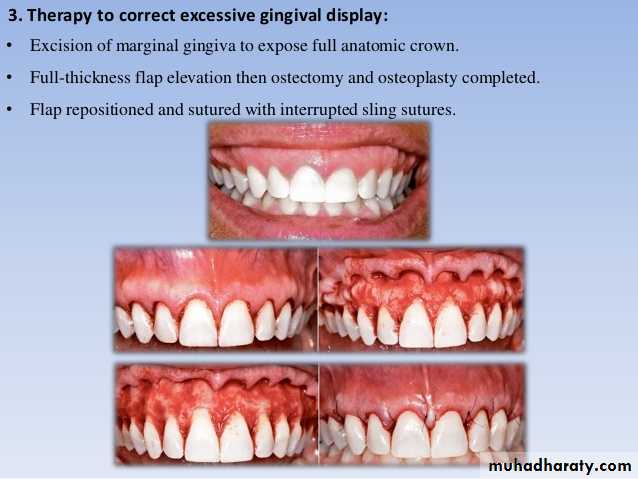
4. Esthetic surgical therapy
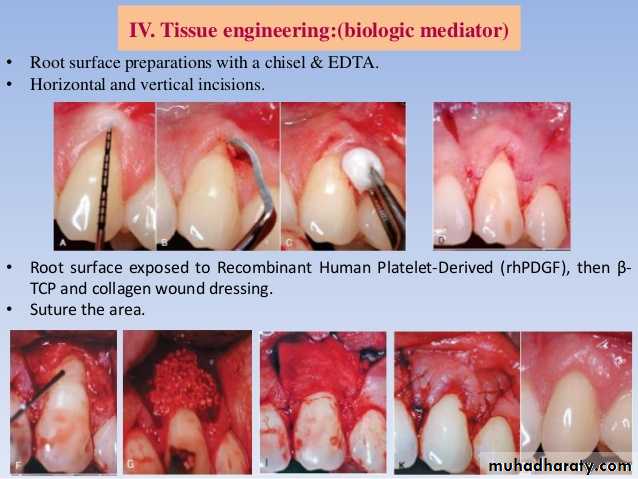
5. Tissue engineering
Problems Associated with Attached Gingiva
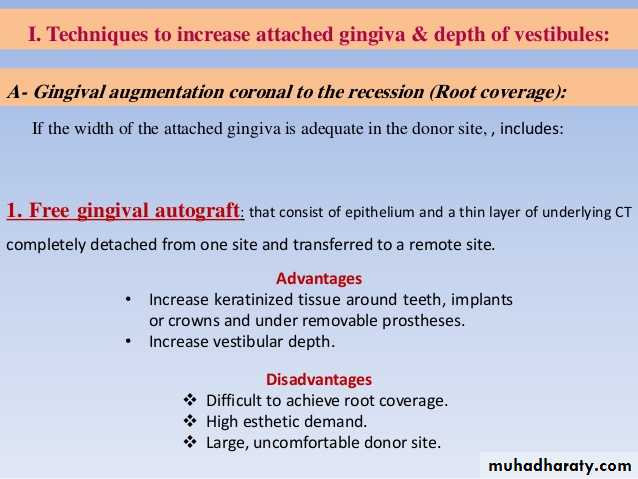
- The ultimate goal of mucogingival surgical procedures is the creation or widening of attached gingiva around teeth and implants. The width of the attached gingiva varies in different individuals and on different teeth of the same individual.
- Attached gingiva is not synonymous with “keratinized gingiva” because the latter also includes the free gingival margin.
- The width of the attached gingiva is determined by subtracting the depth of the sulcus or pocket from the distance between the crest of the gingival margin and the mucogingival junction.
The original rationale for mucogingival surgery was predicated on the assumption that a minimal width of attached gingiva was required to maintain optimal gingival health. However, several studies have challenged the view that a wide, attached gingiva is more protective against the accumulation of plaque than a narrow or a nonexistent zone. No minimum width of attached gingiva has been established as a standard necessary for gingival health. People who practice good, atraumatic oral hygiene may maintain excellent gingival health with almost no attached gingiva.
However, those individuals whose oral hygiene practices are less than optimal can be helped by the presence of keratinized gingiva and vestibular depth. Vestibular depth provides space for easier placement of the toothbrush and prevents brushing on mucosal tissue. To improve esthetics, the objective is the coverage of the denuded root surface.
The maxillary anterior area, especially the facial aspect of the canine, often presents extensive gingival recession. In such cases, the covering of the denuded root surface not
only widens the zone of attached gingiva but also creates a improved esthetic result. This recession and the resultant denuded root surface have a special esthetic concerns for individuals with a high smile line.
A wider zone of attached gingiva is also needed around teeth that serve as abutments for fixed or removable partial dentures, as well as in the ridge areas bearing a denture. Teeth with subgingival restorations and narrow zones of keratinized gingiva have higher gingival inflammation scores than teeth with similar restorations and wide zones of attached gingiva. Therefore, in such cases, techniques for widening the attached gingiva are considered preprosthetic periodontal surgical procedures.
Widening the attached gingiva accomplishes the following four objectives:
1. Enhances plaque removal around the gingival margin.2. Improves esthetics.
3. Reduces inflammation around restored teeth.
4. Gingival margin binds better around teeth and implants with attached gingiva.
Problems Associated with Shallow Vestibule
Another objective of periodontal plastic surgery is the creation of vestibular depth when it is lacking. Gingival recession displaces the gingival margin apically, thus reducing vestibular depth. With minimal vestibular depth, proper hygiene procedures are jeopardized. The sulcular brushing technique requires the placement of the toothbrush at the gingival margin, which may not be possible with reduced vestibular depth.Minimal attached gingiva with adequate vestibular depth may not require surgical correction if proper atraumatic hygiene is practiced with a soft brush. Minimal amounts of keratinized attached gingiva with no vestibular depth benefit from mucogingival correction. Adequate vestibular depth is also necessary for the proper placement of removable prostheses.
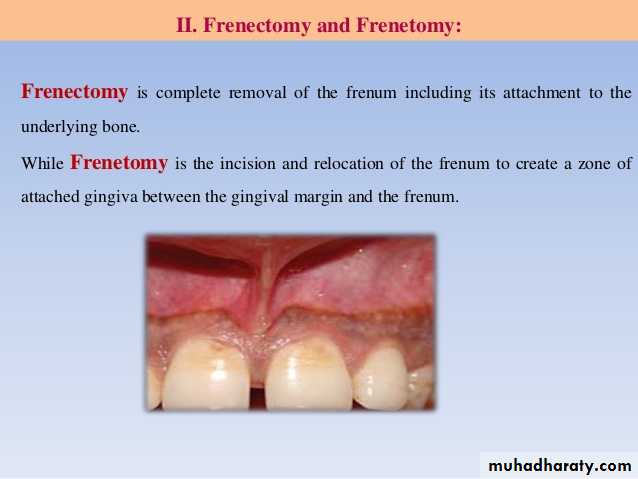
Problems Associated with Aberrant Frenum
Another important objective of periodontal plastic surgery is to correct frenal or muscle attachments that may extend coronal to the mucogingival junction. If adequate keratinized, attached gingiva is present coronal to the frenum, it may not be necessary to remove the frenum. A frenum that encroaches on the margin of the gingiva may interfere with plaque removal, and the tension on the frenum may tend to open the sulcus. In such cases, surgical removal of the frenum is indicated.ETIOLOGY OF MARGINAL TISSUE RECESSION
The most common cause of gingival recession and the loss of attached gingiva is abrasive and traumatic tooth-brushing habits. The bone and soft tissue anatomy of the buccal, radicular surface of the dentition is usually thin, especially around the anterior area.Teeth positioned buccally may have a even thinner bone and gingiva. In many instances, such areas may have a complete absence of bone beneath the thin overlying gingival tissue. Such defect in the bone is called a dehiscence. This anatomic status combined with external trauma from overzealous brushing can lead to the loss of gingival tissue.
Recession of the gingival tissue and bone exposes the cemental surface of the root, which results in abrasion and “ditching” of the cemental surface apical to the cementoenamel junction (CEJ). The cementum is softer than enamel and will be destroyed before the enamel surface of the crown.
Another cause for gingival recession is periodontal disease and chronic marginal inflammation. The loss of attachment caused by the inflammation is followed by the loss of bone and gingiva.
Advanced periodontal involvement in areas of minimal attached gingiva results in the base of the pocket extending close to, or apical to, the mucogingival junction. Periodontal therapy of these areas also results in gingival recession caused by the loss of gingiva and bone.
Frenal and muscle attachments that encroach on the marginal gingiva can distend the gingival sulcus, which creates an environment for plaque accumulation. This condition increases the rate periodontal recession and will contribute to the recurrence of the recession even after treatment. These problems are more common on facial surfaces, but may also occur on the lingual surface.
Orthodontic tooth movement through a thin buccal osseous plate may lead to a dehiscence beneath a thin gingiva. This also can lead to the recession of the gingiva
FACTORS THAT AFFECT SURGICAL OUTCOME
1. Irregularity of TeethThe location of the gingival margin, width of the attached gingiva, and alveolar bone height and thickness are all affected by tooth alignment. On teeth that are tilted or rotated labially, the labial bony plate is thinner and located farther apically than on the adjacent teeth; therefore the gingiva is recessed so that the root is exposed. On the lingual surface of such teeth, the gingiva is bulbous, and the bone margins are closer to the CEJ.
2. Mucogingival Line (Junction)
Normally, the mucogingival line in the incisor and canine areas is located approximately 3 mm apical to the crest of the alveolar bone on the radicular surfaces and 5 mm interdentally. In periodontal disease and on malposed disease free teeth, the bone margin is located farther apically and may extend beyond the mucogingival line. The distance between the mucogingival line and the CEJ before and after periodontal surgery is not necessarily constant. After inflammation is eliminated, the tissue tends to contract and draw the mucogingival line in the direction of the crown.CRITERIA FOR SELECTION OF TECHNIQUES
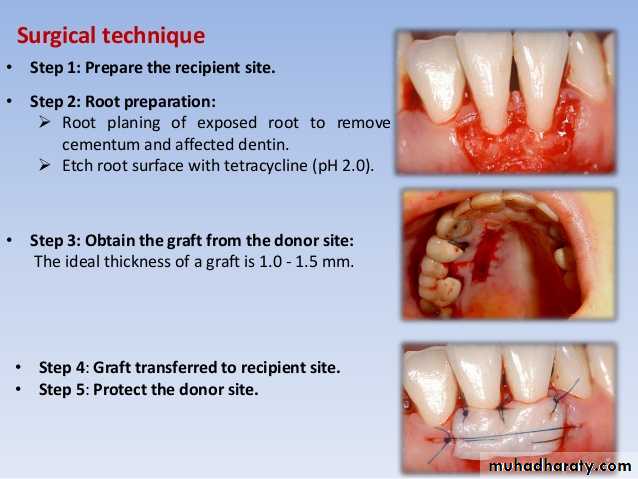
1. Surgical site free of plaque, calculus, and inflammation.Periodontal plastic surgical procedures should be undertaken in a plaque-free and inflammation-free environment to enable the clinician to manage gingival tissue that is firm. Meticulous, precise incisions and flap reflection cannot be achieved when the tissue is inflamed and edematous. Thorough scaling and root planing, as well as meticulous plaque removal by the patient, must be accomplished before any surgical procedure.