Surgical aids to orthodontics
● Some orthodontic procedures require surgical assistance.● Unerupted or impacted teeth are the most common reason for surgical intervention but, occasionally, soft-tissue surgery is indicated.
● Some cases cannot be treated simply by orthodontics alone and require surgery to the mandible and/or maxilla—orthognathic surgery (osteotomies). Such cases require a combined approach and careful planning to ensure optimal results.
● Although treatment of facial deformity is not within the scope of general dentistry, the dentist has an essential role to play in the general dental care of such patients. This is especially important in cleft patients.
Surgery in the orthodontic patient will often be an integral part of a protracted treatment program which may, especially in the case of adult fixed appliance therapy, take 2 years or more to complete.
It is essential, at the planning stage of the dentoalveolar surgery, that patients understand (and are willing to comply with) the extent and duration of the proposed therapy.
The interface between oral surgery and orthodontics is difficult to define accurately but relates to those patients whose treatment decisions lie within both specialties. There will always be cases where choices must be made—to recommend orthodontics alone, surgery alone, a combination of the two or whether no intervention should be recommended.
MANAGEMENT OF UNERUPTED AND IMPACTED TEETH
Assessment of unerupted teeth—clinicalThe combined oral surgery and orthodontic treatment options for unerupted teeth are threefold: extraction, exposure ± orthodontics and autotransplantation (most frequently of canines).
The timing of extractions or exposure is dependent on the age of the patient and the stage of development of the dentition.
Assessment of unerupted teeth—radiographic
Most orthodontic assessment will include an ortho-pantomogram (OPG) and a lateral cephalometric view. Intraoral views are essential, however, for the management of unerupted maxillary anterior teeth due to the poor definition of the OPG in this region. In this situation, the OPT will usually be supplemented with periapical and/or upper anterior occlusal films.The use of ‘parallax’ analysis (Clark’s rule), in which two periapical views of the same area are taken from different angles, can be useful in determining whether the impacted teeth are buccal or palatal and therefore in planning the surgical approach to the teeth.
In radiographic analysis, the stage of tooth development must also be carefully considered because it is inappropriate to expose teeth whose development is incomplete.
Exposure of unerupted teeth
The decision to expose or not is principally based on three factors: the angulation of the unerupted tooth, the depth of impaction and the relationship to other teeth. In general terms there are four treatment options:● extraction
● autotransplantation● simple exposure
● exposure with the application of direct mechanical force
to the tooth.
The principles of treatment planning in relation to the anterior maxillary region can equally be applied in relation to unerupted teeth at other sites, most commonly mandibular second premolar teeth, central incisors, or even wisdom teeth.
The objective of exposing an unerupted tooth is to move it into a good functional and aesthetic position. In assessing teeth for exposure one of the prime considerations is the available space into which the tooth can erupt. This may be estimated by comparing the crown width of the unerupted tooth with the available space, either directly from the radiograph (with reference to the magnification in the system) or by measurement of the crown width of the contralateral corresponding tooth.
ARMAMENTARIUM FOR EXPOSURE/BONDING PROCEDURE
Instruments and supplies needed for the surgical procedure of exposing and bonding an eruption device to an impacted canine include:1. Surgical instrumentation to allow incision, flap reflection, and suturing of the soft tissue as required
2. Orthodontic pliers that allow easy grasping, manipulation, and placement of the eruption bracket/chain
3. Eruption devices usually consisting of an orthodontic bracket with attached small gold-link chain
4. Light-cured orthodontic composite/adhesive or cyanoacrylate cement
5. Hemostatic agent, such as Hemodent, and cotton pellets for application/packing around the exposed tooth
Surgical technique
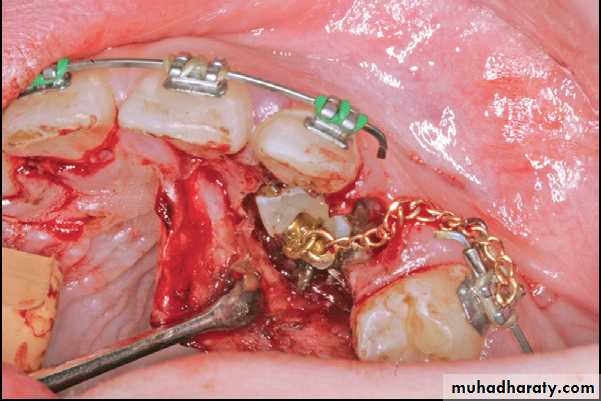
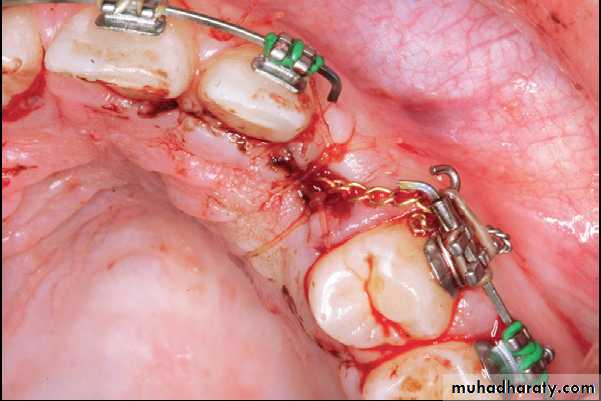
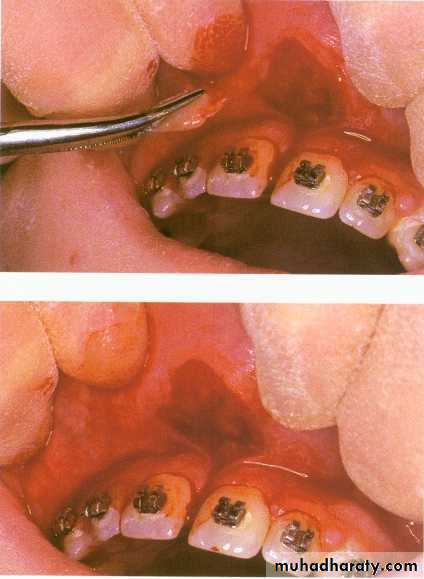
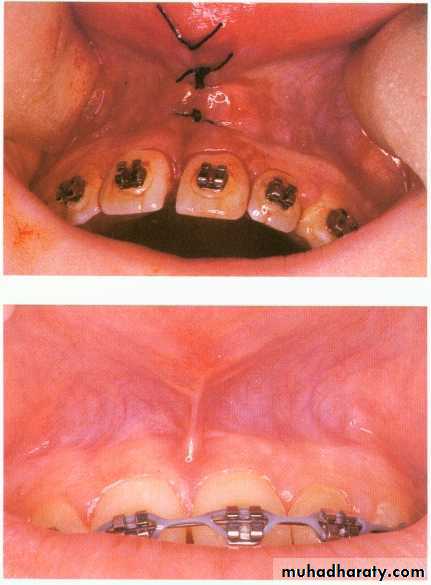
Two basic approaches, either a “closed” or “open” technique, are used to provide access to the impacted canine.1)) In the “closed eruption” technique, the crown of the canine is exposed, the orthodontic eruption device is attached to the crown, and the flap is sutured back over the tooth, leaving only the eruption chain exposed for orthodontic manipulation. The eruption chain is usually exited through either the crestal incision or the extraction site of the primary canine and ligated to the archwire or brackets on the adjacent teeth.
Flap, closed eruption procedure for exposure (A), and bonding (B) of palatally impacted canine. C, Flap sutured back over the tooth, leaving only the eruption chain exposed.
2)) In the “open eruption” technique, the crown of the impacted tooth is exposed with either an opening cut into the overlying tissue without flap reflection, or a flap is reflected, a window cut in it, and then the flap is repositioned.
Flapless open procedure (A), with periodontal dressing applied (B) for palatally impacted canine
Exposure at its simplest consists of removal of the soft tissues overlying the crown of an unerupted tooth under local anaesthetic (open exposure).
The exposure of teeth in this fashion has major disadvantages:
● removal of the attached keratinized gingiva
● the possibility of re-epithelialization and healing of
the defect before the tooth has time to erupt
● the loss of an acceptable mucogingival contour.
After exposure of the impacted tooth, the overlying bone is removed with a bur or curette, and the follicle is minimally debrided to allow access to the tooth. In the closed technique, the eruption bracket/chain is bonded to the tooth at the time of surgery; in the open technique, it can be done at the time of surgery by the surgeon or done at a subsequent appointment with the orthodontist.
Hemostasis can be achieved using electrosurgery or by packing cotton pellets soaked in hemostatic agents around the exposed tooth. The isolated tooth is then etched, rinsed and dried, and the eruption device bonded to the tooth using a light-cured, acid-etch composite material. Positioning of the bracket as near to or on the incisal edge of the tooth provides the orthodontist with the best mechanical advantage for positioning of the tooth
Uprighting of Second Molars
1)) Orthodontic uprighting
2)) Surgical uprighting: The advantages of this approach are that only a single surgical procedure is necessary with a shorter overall treatment time compared with other nonsurgical options. Although there is a potential risk of root fracture and pulpal necrosis, these are exceedingly rare when the appropriate technique is used.
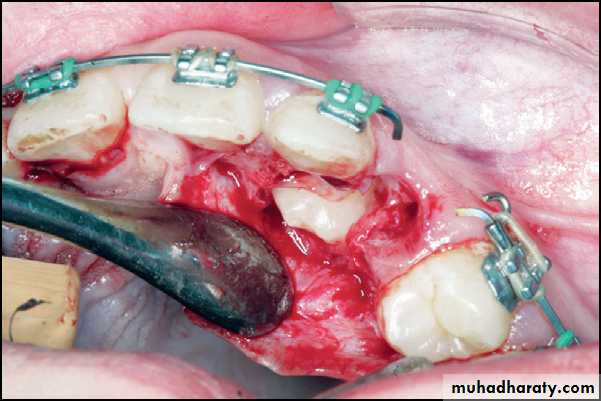
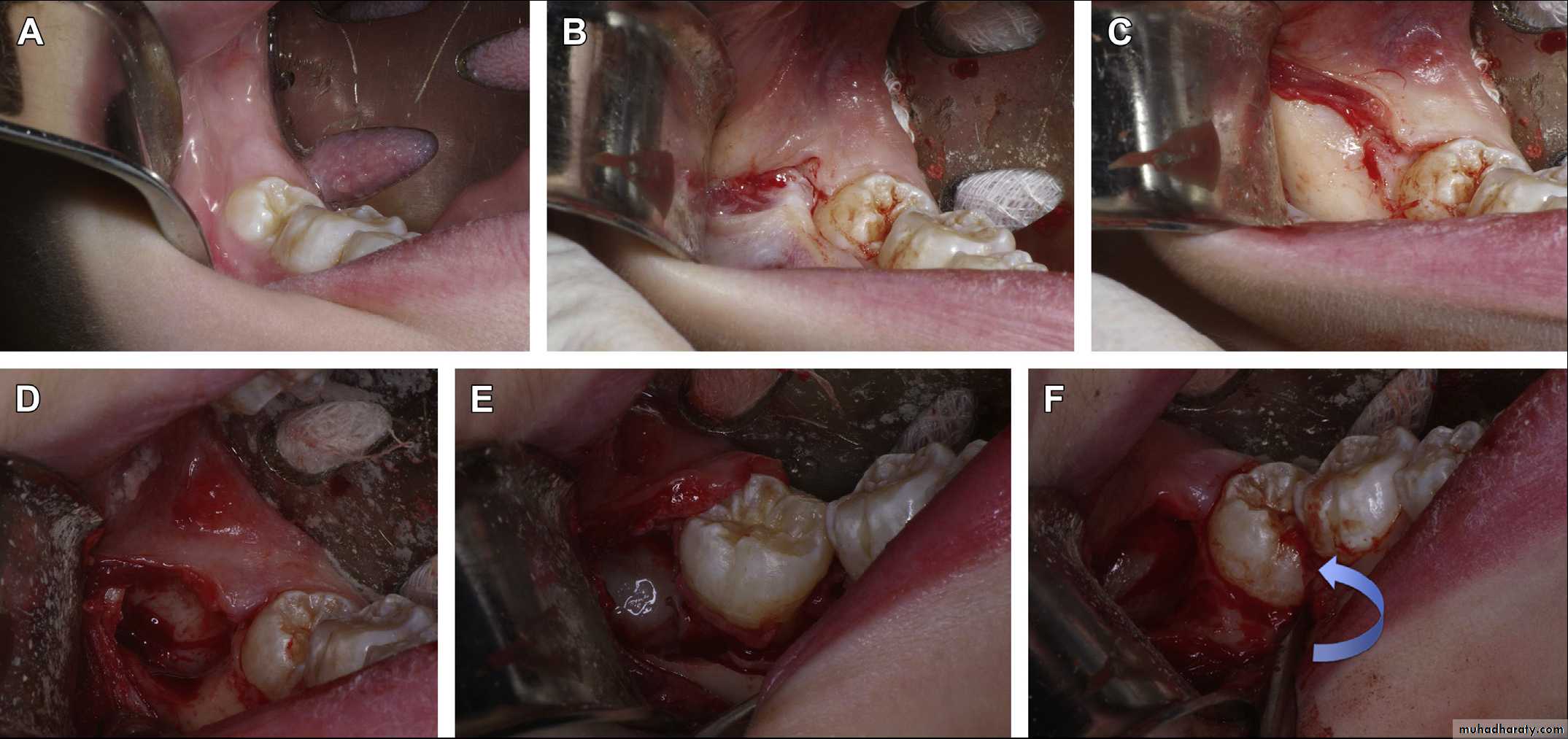
Procedure
The procedure should ideally be performed when two-thirds of the second molar root is formed, which is usually between the ages of 11 and 14. If surgery is performed too soon then the tooth may be unstable and may shift in position. If performed too late then there is risk of root fracture and possible disruption of blood supply leading to pulpal necrosis.After adequate anesthesia, a mucoperiosteal flap is elevated distal to the first molar. Ostectomy is performed as necessary with a surgical drill to expose the second molar, and soft tissue around the crown is debrided. A dental elevator is used to apply distal and occlusal pressure to the tooth until the mesial marginal ridge of the second molar is at the same level as the distal marginal ridge of the adjacent first molar.
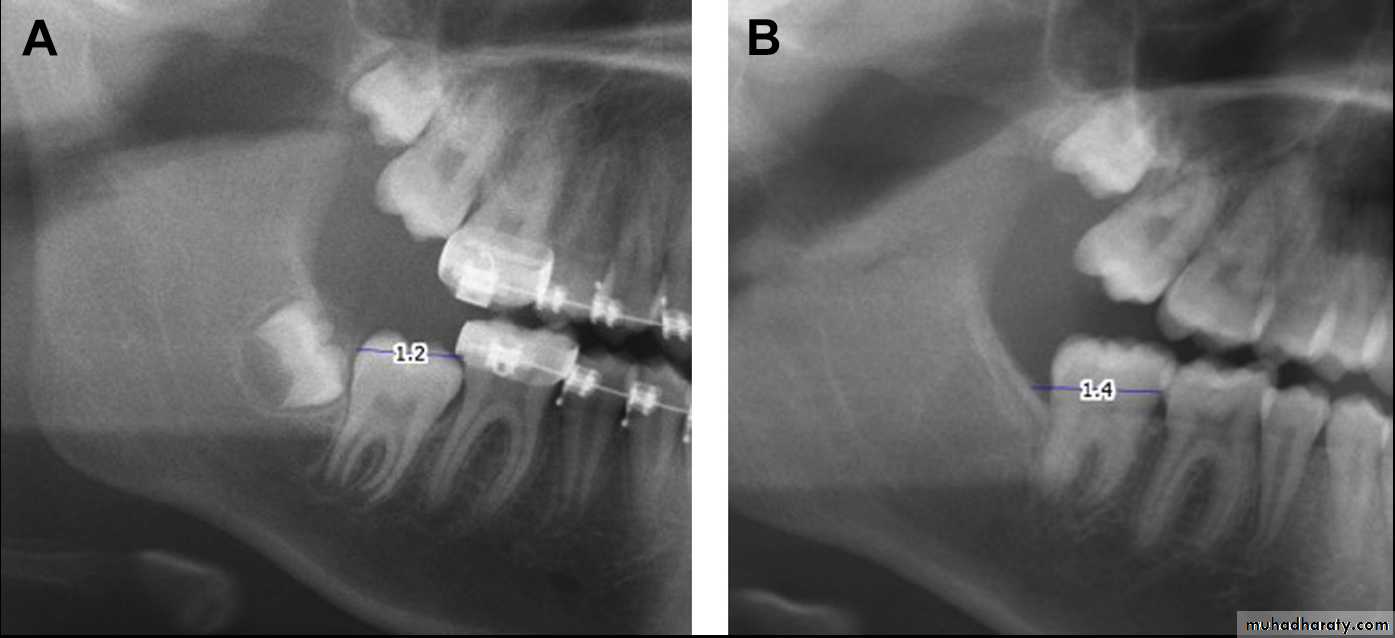
A, Posterior eruption space, measured from the distal contact point of the first molar to the most inferior point on the ascending ramus, on a preoperative image. B, Postoperative radiograph of the same patient.
Auto-transplantation and re-implantation
In the past, autotransplantation was a popular treatment for unerupted canine, premolar and even molar teeth but there are some considerable biological problems associated with the technique to be overcome.
Most transplanted teeth will develop evidence of root resorption or even ankylosis if they are not root-treated. The success rate of transplantation can be maximized by careful handling of the tooth and preparation of the socket with minimal trauma.
Resorption is directly infl uenced by the extent of trauma to the periodontal tissues on the root surface and care must be taken to minimize this during the removal of the tooth.
During the removal of the unerupted tooth only the crown of the tooth should be manipulated with instruments and whilst the socket is being prepared
the tooth is ‘stored’ in the buccal or palatal sulcus beneath the fl ap.
When preparing the ‘socket’, bone removal should be undertaken very carefully, with particular reference to not generating heat. A slow running, well-irrigated bur is the preferred option to achieve this, although some surgeons use small chisels or osteotomes to remove the bone or expand the socket.
The repositioned tooth should be secured free from occlusion and splinted in place, usually by direct bonding using orthodontic brackets or wire and composite. Alternatively a thin vacuum-formed splint can be constructed and cemented in place. Following removal of the splint (usually after 3 weeks) the tooth should be root-filled with calcium hydroxide and reviewed clinically and radiographically at regular 3-month intervals for at least 1 year to check for resorption or ankylosis.
SUPERNUMERARY TEETH AND ODONTOMES
Supernumerary teeth and odontomes often must be removed as they can delay eruption or impede orthodontic tooth movement, particularly of maxillary incisors. If supernumerary teeth are removed from the path of eruption, the underlying teeth will often erupt given sufficient space. It has been estimated that this will occur spontaneously in approximately 60% of cases.An inverted supernumerary tooth—usually referred to as a mesiodens if it occurs in the incisor region. It should only be removed if there is a genuine clinical indication.
Odontomes are less common than supernumerary teeth, although the differentiation between the two is considerably blurred. Odontomes may be simple (tooth-like), compound (multiple tooth-like) or complex composite (containing elements of the tooth germ in a disorganized fashion). Like unerupted teeth, odontomes need only be removed if there are clinical indications (as infection, they are obstructing eruption of other teeth, and esthetic problems).
FRENECTOMY
Frenectomy—the surgical removal of fraenal attachments (usually in the midline) in the upper or lower jaw—may be a valuable surgical adjunct to orthodontic therapy.
Labial frenectomy
Upper labial frenectomy aims to remove or reposition the entire labial frenum, including its attachment to bone, and to remove all interdental tissue. It must be remembered that spacing of the incisors in children is a normal developmental process and is present until the eruption of the permanent canine teeth in adolescents.Labial frenectomy should usually be delayed until after orthodontic treatment, unless the labial frenum prevents closure of a diastema or displays evidence of trauma. The technique is usually performed if the frenum extends to the incisive papilla and contributes to post-treatment stability of the orthodontically closed diastema.
Procedure
Under local anesthesia the upper lip is firmly retracted, demonstrating the extent of the fraenal attachment. If the frenum is particularly fibrous, its whole length is outlined and excised with a scalpel using an elliptical or rhomboid incision. The remaining fibres attached to the exposed bone can be curetted or gently removed with a bur but care must be taken not to damage the roots of adjacent teeth. The mucosa is then undermined and the defect closed with simple interrupted sutures. Patients are normally reviewed in 5–7 days.Lingual frenectomy
Lingual frenectomies are occasionally recommended in younger children to assist in phonetic development or to avoid functional embarrassment. In older patients it may also be undertaken if tongue movement is so restricted that patients cannot lick the buccal surfaces of their upper molars to aid oral hygiene.The procedure is usually performed under local anesthesia. The surgical technique is similar to that of a labial frenectomy although minimal tissue removal, if any, is required.
Periodontal problems associated with a high lingual frenum, resulting in direct trauma and poor oral hygiene.
Surgical Assistance for Rapid Orthodontic Treatment
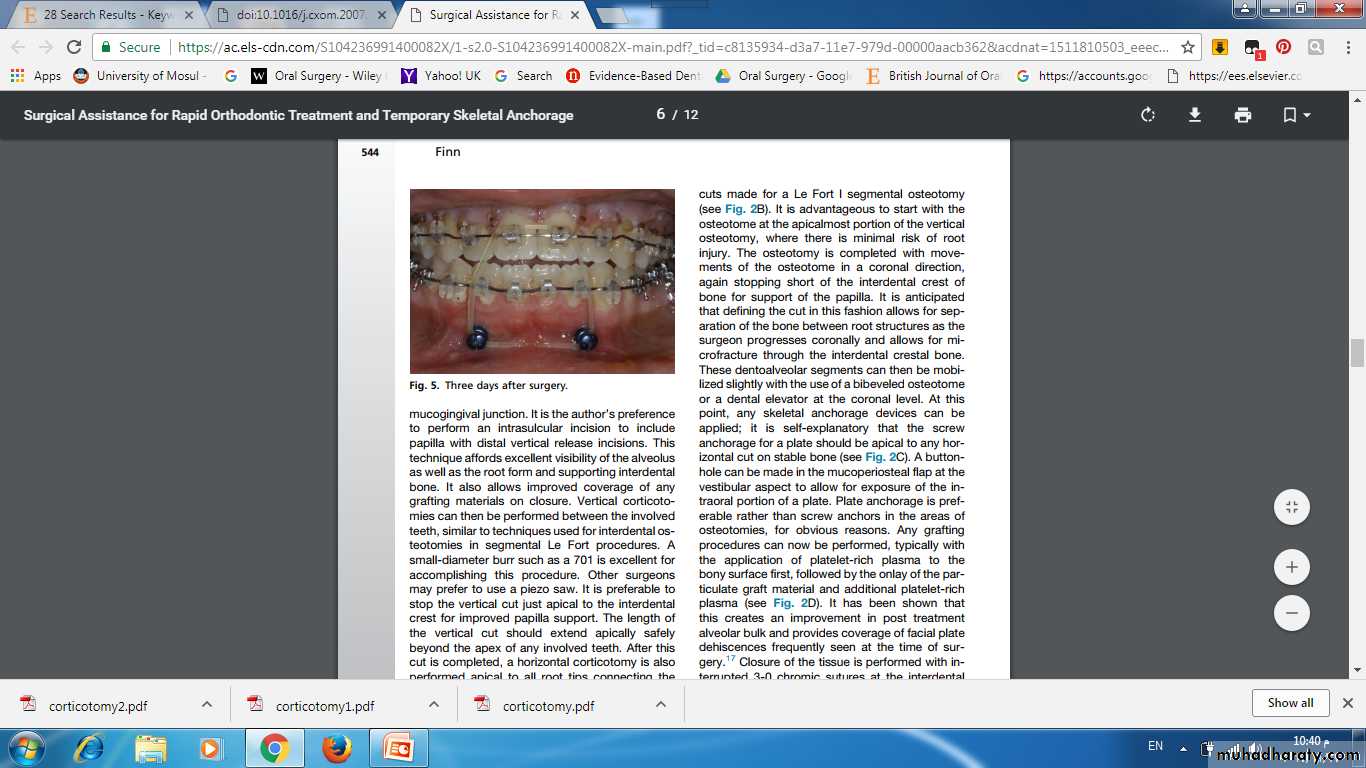
CorticotomySurgically assisted osteogenic orthodontics is a departure from earlier described techniques such as accelerated osteogenic orthodontics in that multiple modalities are combined not only to shorten treatment time but to accomplish results that cannot be achieved with orthodontics alone. Accelerated osteogenic orthodontics simply improves treatment time of otherwise regularly performed orthodontics, whereas surgically assisted osteogenic orthodontics can replace procedures such as orthognathic surgery or facilitate otherwise improbable orthodontic mechanics.
Procedure
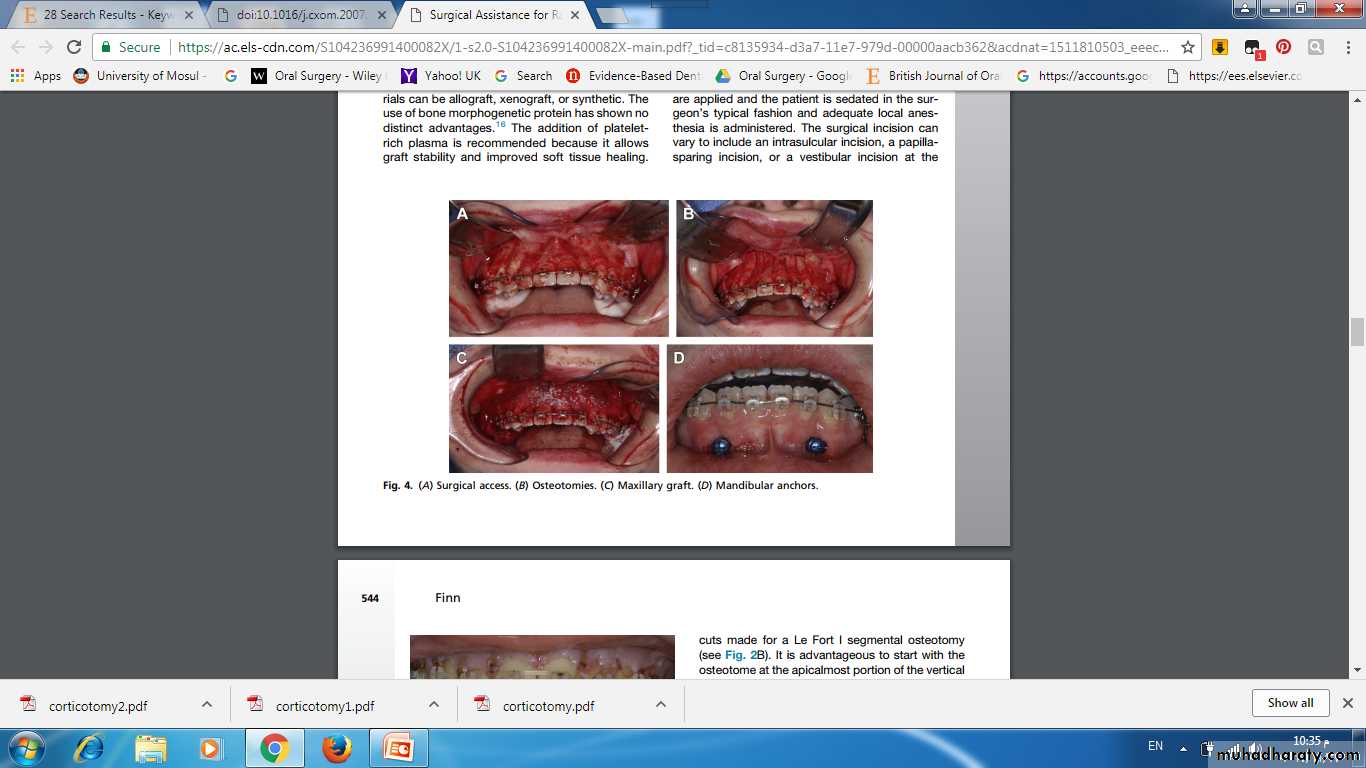
After elevating a mucoperiosteal flap, a series of vertical corticotomies are made in the labial and palatal compact bone around teeth to be moved. The apical ends of these cuts are joined by horizontal cuts, leaving the teeth supported by cancellous bone only. Bone chips or bone substitutes can be used to fill the gaps. After closure, strong orthodontic pressure, usually by traction elastics, is applied. A retainer should be worn for few days postoperatively.• Surgical access.
• (B) Osteotomies.
• Maxillary graft.
• Mandibular anchors.
• Temporary skeletal anchorage.
E