LASERS AND IT’S USES IN DENTISTRY
Technology helps to reduce treatment time and treatment more comfortable.

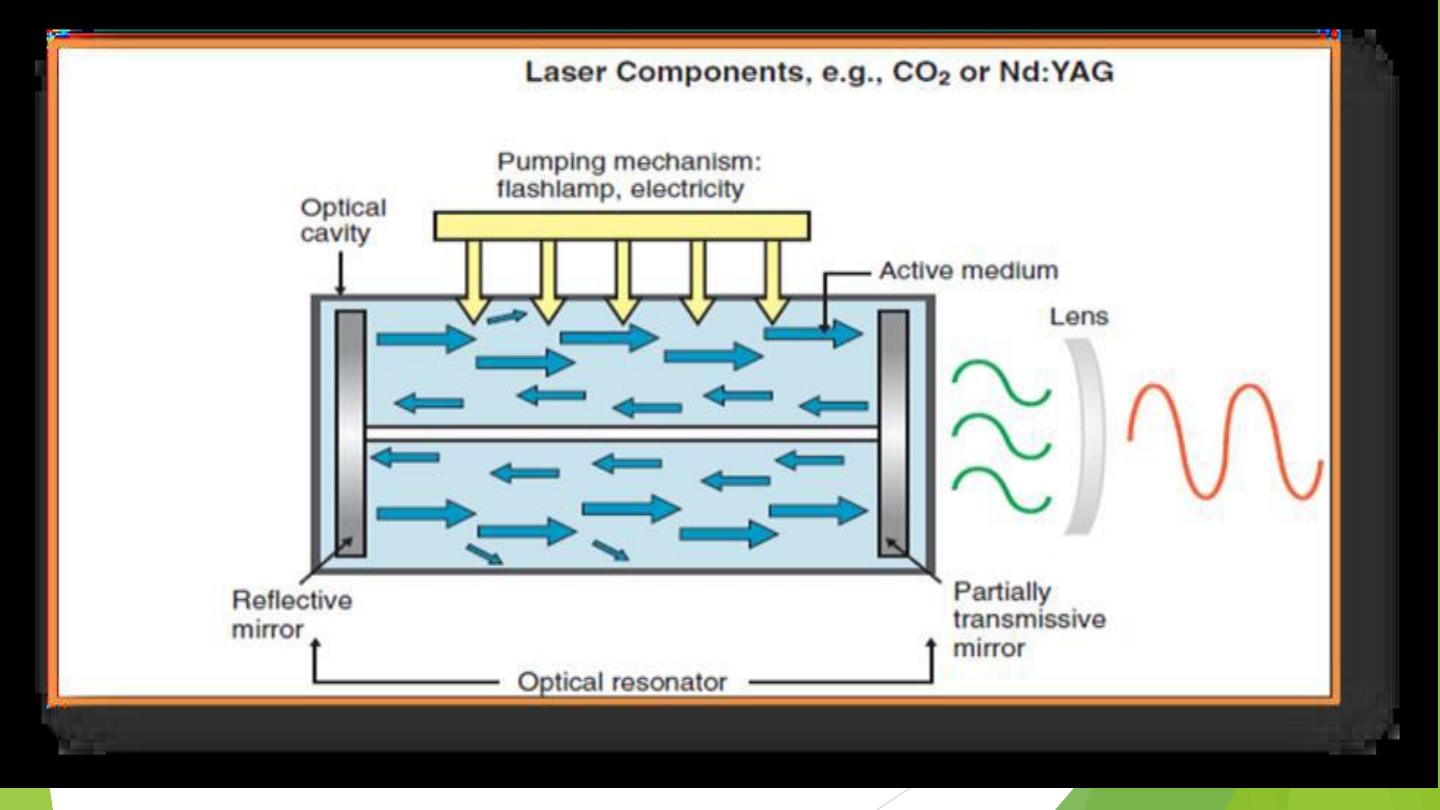
Fundamentals Of Laser Operation
Active medium [ Lasing Medium ]
Pumping mechanism
Optical Resonators
Laser Delivery System
Cooling system
Control Panel
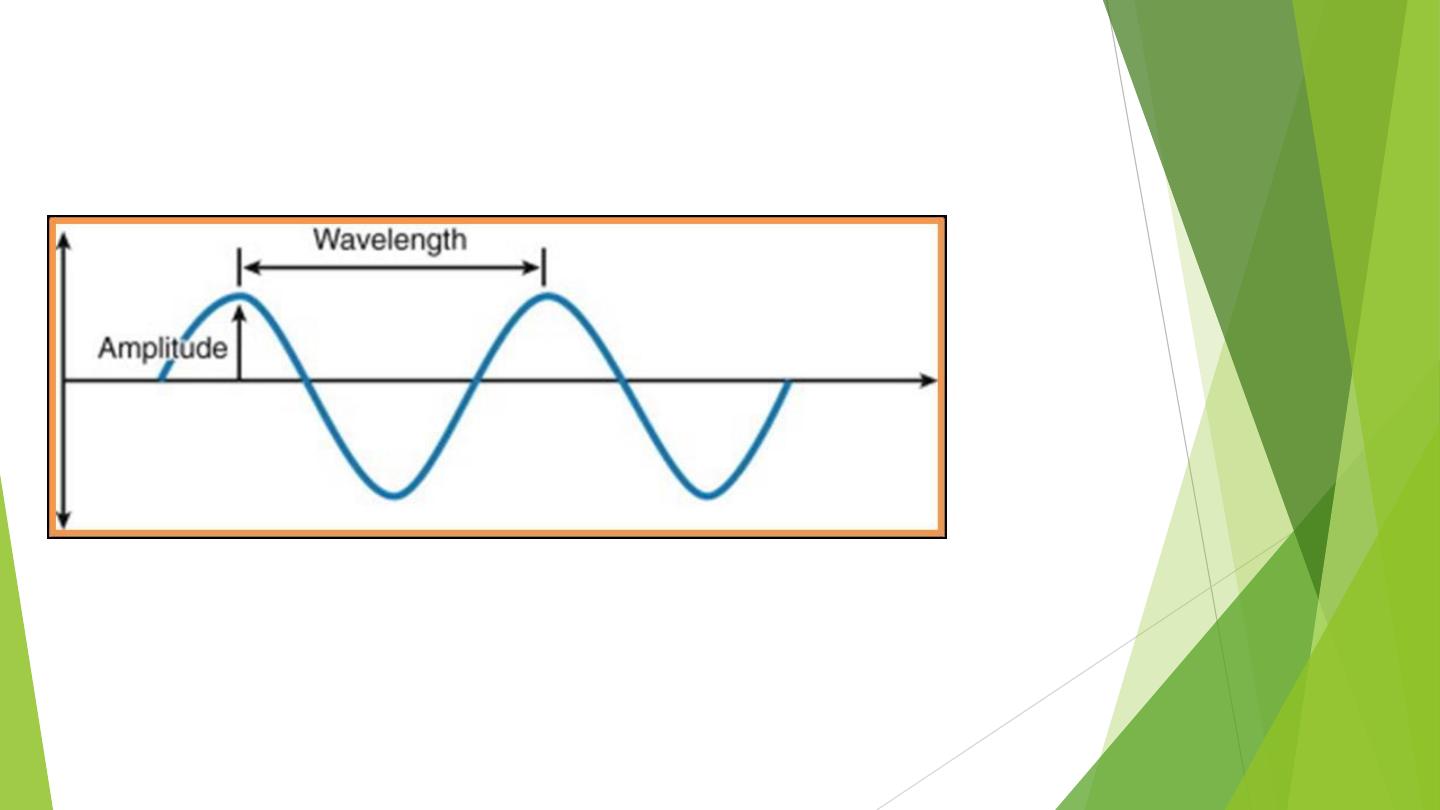
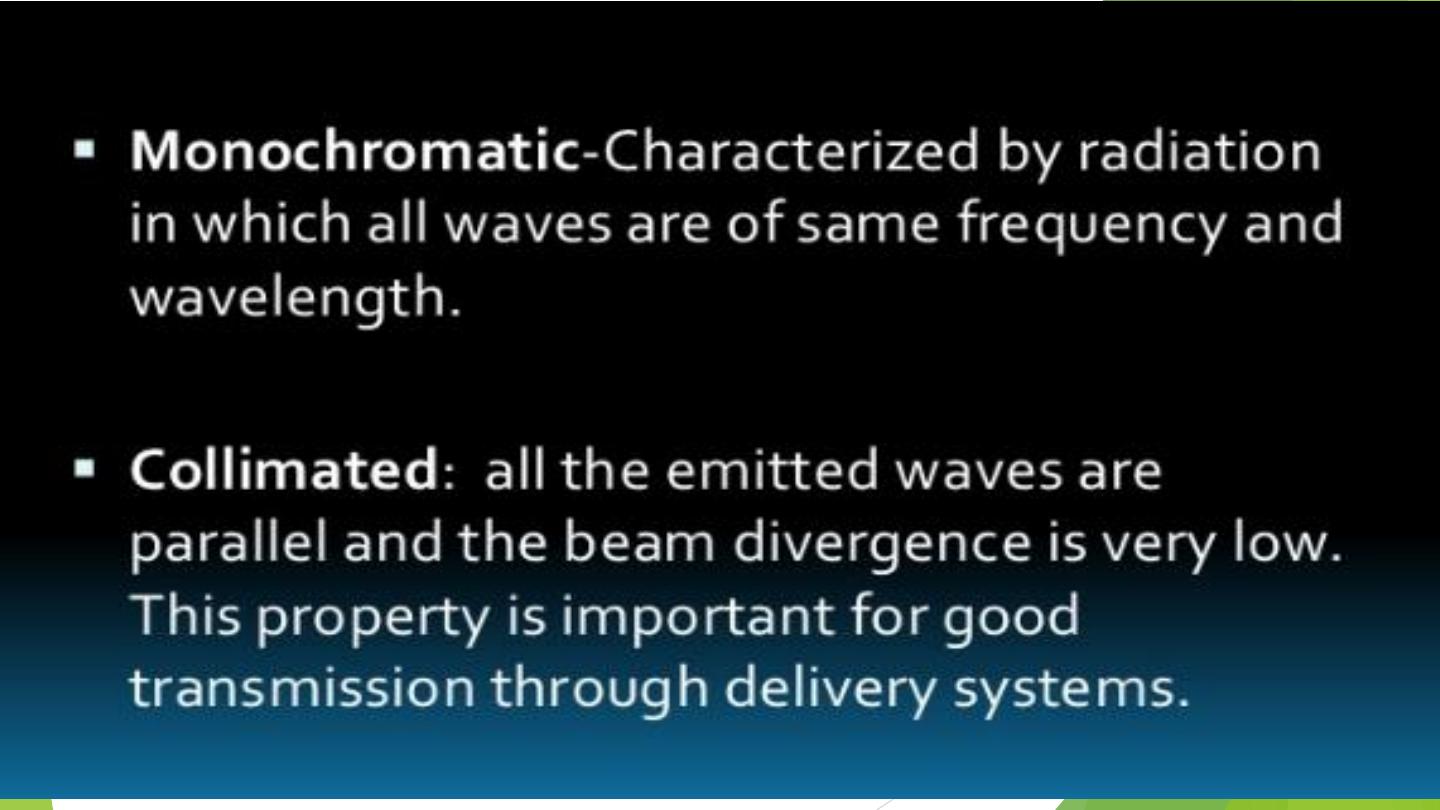
Waveform of photon
The waveform characterized by the distance between the crest of two successive wave peaks
referred to as the
wavelength
reported in nanometer (nm) or micrometer (μm). The wave of
photons, moving at the speed of light, can be defined by three properties
a. The first
is
amplitude
,
which is the total height of the wave oscillation from the top of the peak to
the zero line on a vertical axis. This is an indication of the amount of intensity in the wave.
b. The second property
is
wavelength,
which is the distance between any two corresponding axis.

The wavelength of this monochromatic light is dependent on
the medium in the optical
cavity
. For example, the solid state Erbium:yttrium-aluminum-garnet (Er:YAG)Laser, which is an
erbium rod doped with yitrium, aluminum, and garnet impurities—produces energy of 2940 nm (sometimes
noted as 2.94 mm). One of the principal wavelengths of the CO2 laser is 10,600 nm (10.6 mm).
c. The third is the frequency (v),
As waves travel, they rotate around the zero axis
; certain number
of times per second; this is called
oscillation
The number of oscillations per unit time is defined as
frequency.
The frequency is measured in hertz (Hz);
1 Hz equals one oscillation per second. It is inversely proportional to wavelength: the shorter the wavelength,
the higher the frequency, and vice versa expressed in Hertz (Hz) or cycles per second.
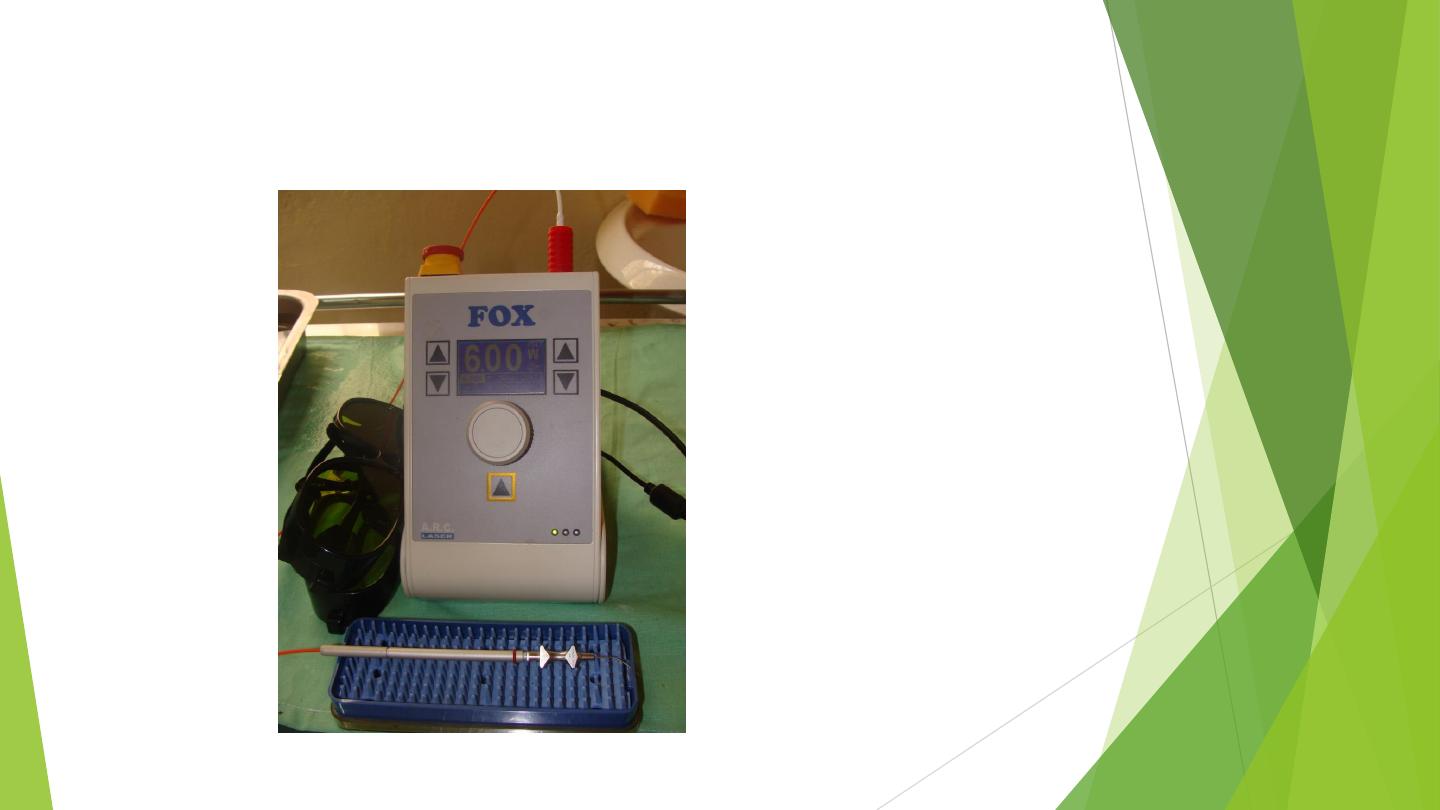
Energy
is a measure of work and is reported in
joules
(J).
Power
is a measure of the rate that work is taking
place, is measured in
J/s and reported in
watt
s (W).

Lasers consist of basic components, which include an active lasing medium, is
composed of chemical elements molecules, or compounds. Lasers are generically
named for the material of the active medium, which can be
Laser production step
a. Amplification
a. A container of gas, such as carbon dioxide (CO
2
) gas in a CO
2
laser;
b. A solid crystal, such as a crystal of yttrium, aluminum, and garnet (YAG) in an erbium (Er)
YAG or a neodymium (Nd) YAG laser.
c. A solid-state semiconductor, such as the semiconductors found in diode lasers.
d. A liquid,
, this is enclosed within a laser cavity bounded by two parallel reflectors (mirrors). High-
energy radiation is pumped into the active medium by means of a pump source.
The energy provided by an intense optical or electrical discharge. The energy from the pump
source is absorbed by the active raised to their upper energy state. The electrons in this
excited state then spontaneously give off that energy in the form of a photon This is called
spontaneous emission
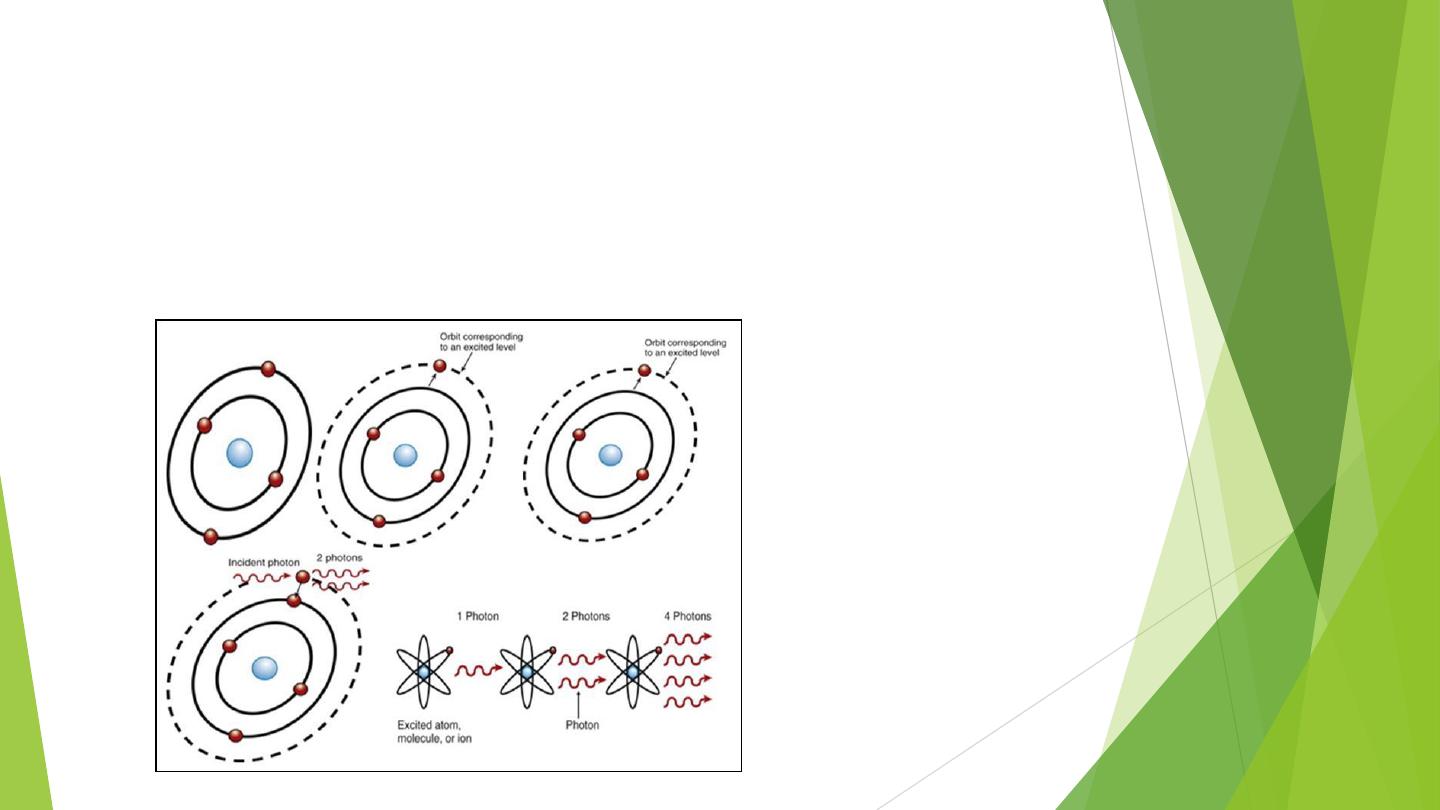
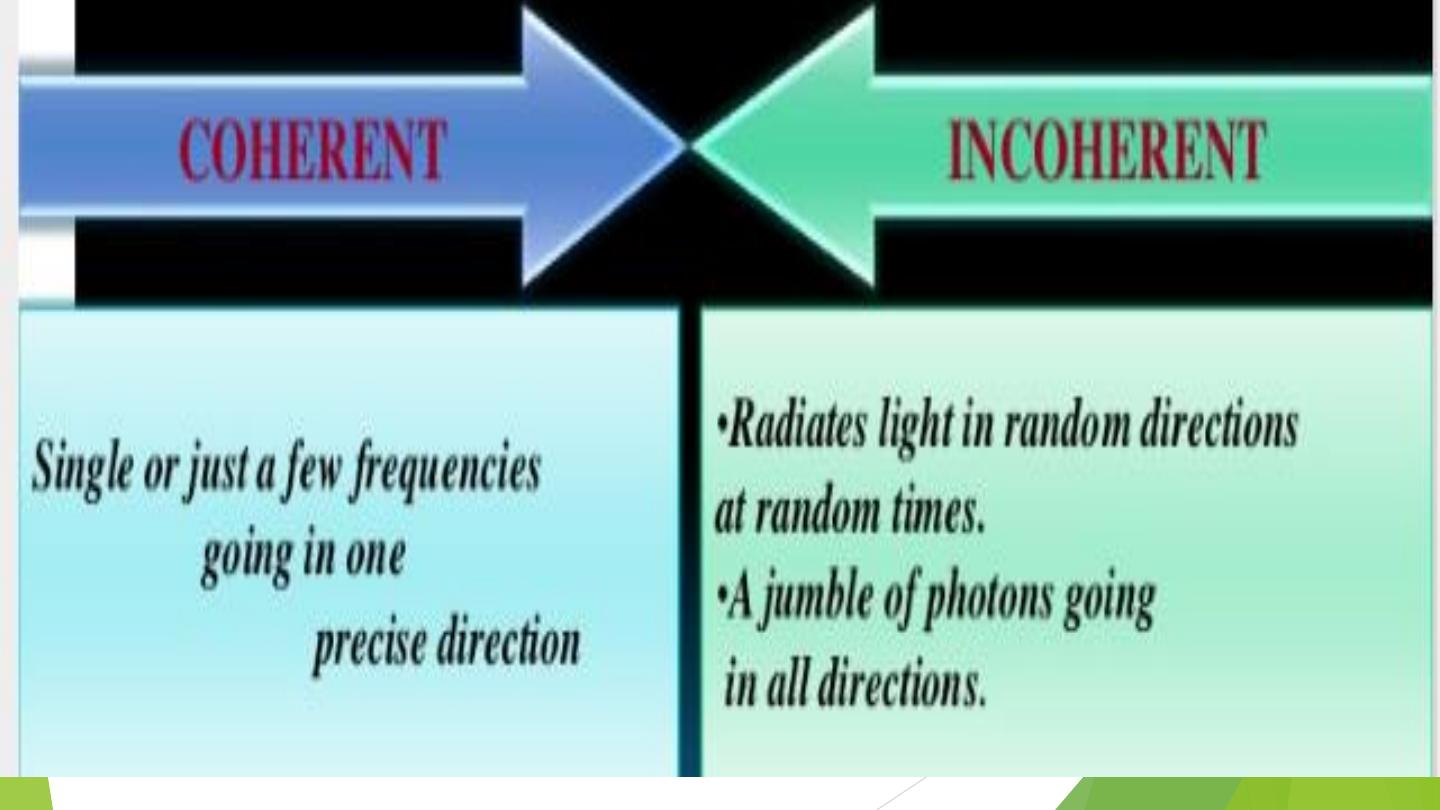
b. Stimulated Emission
The laser‘s energy source, either from an electrical field or from light, produces a photon within
the optical cavity that is spontaneously emitted.This photon act together s with a molecule of the
medium, causing an electron to skip to a less steady superior energy level. Because this
electron position is unstable, it will immediately relapse back to its stable state, releasing
another photon as it returns to its more steady lower state.

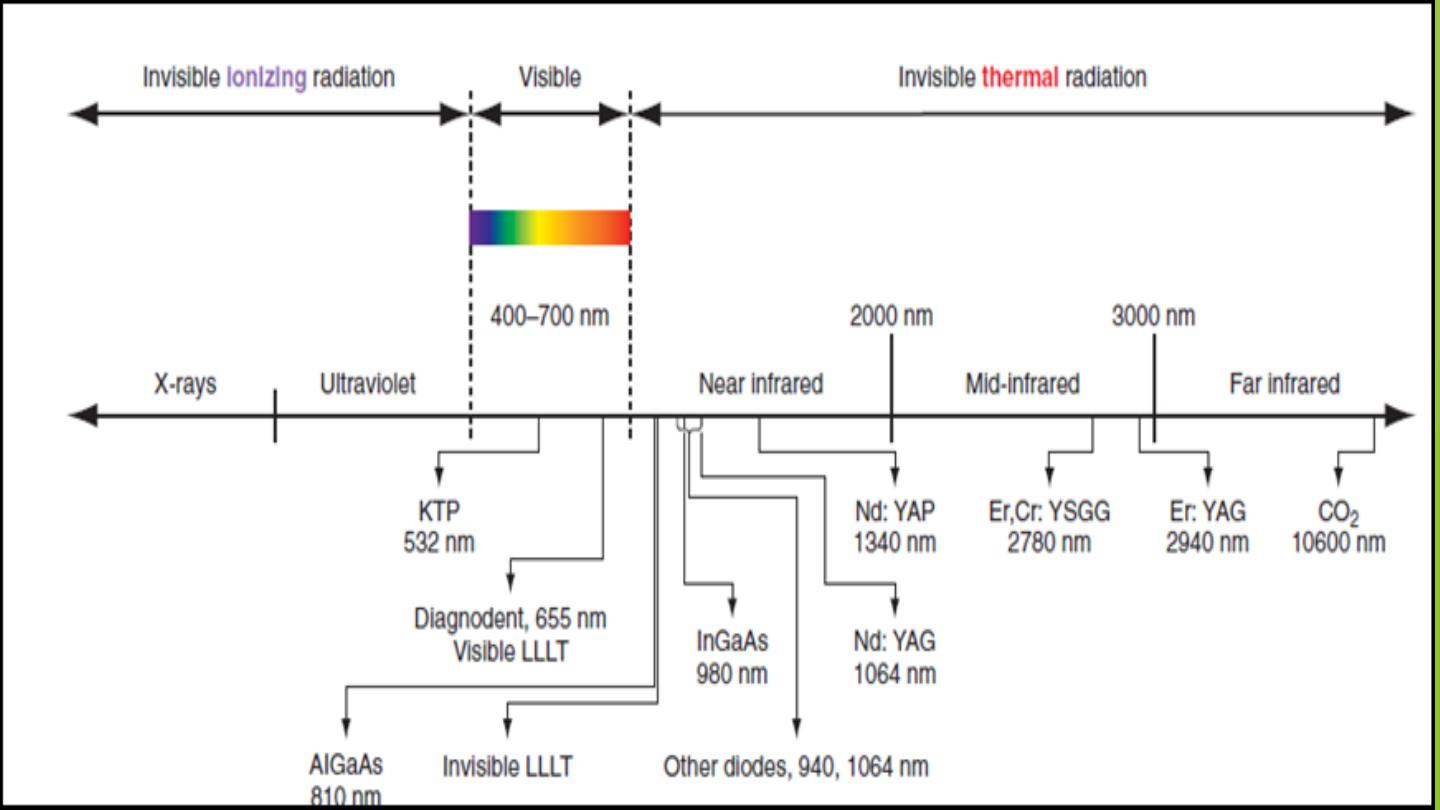
The
electromagnetic spectrum
is the entire collection of wave energy,
ranging from gamma rays, with wavelengths of 10 to 10
−12
m, to radio
waves, with wavelengths of thousands of meters .
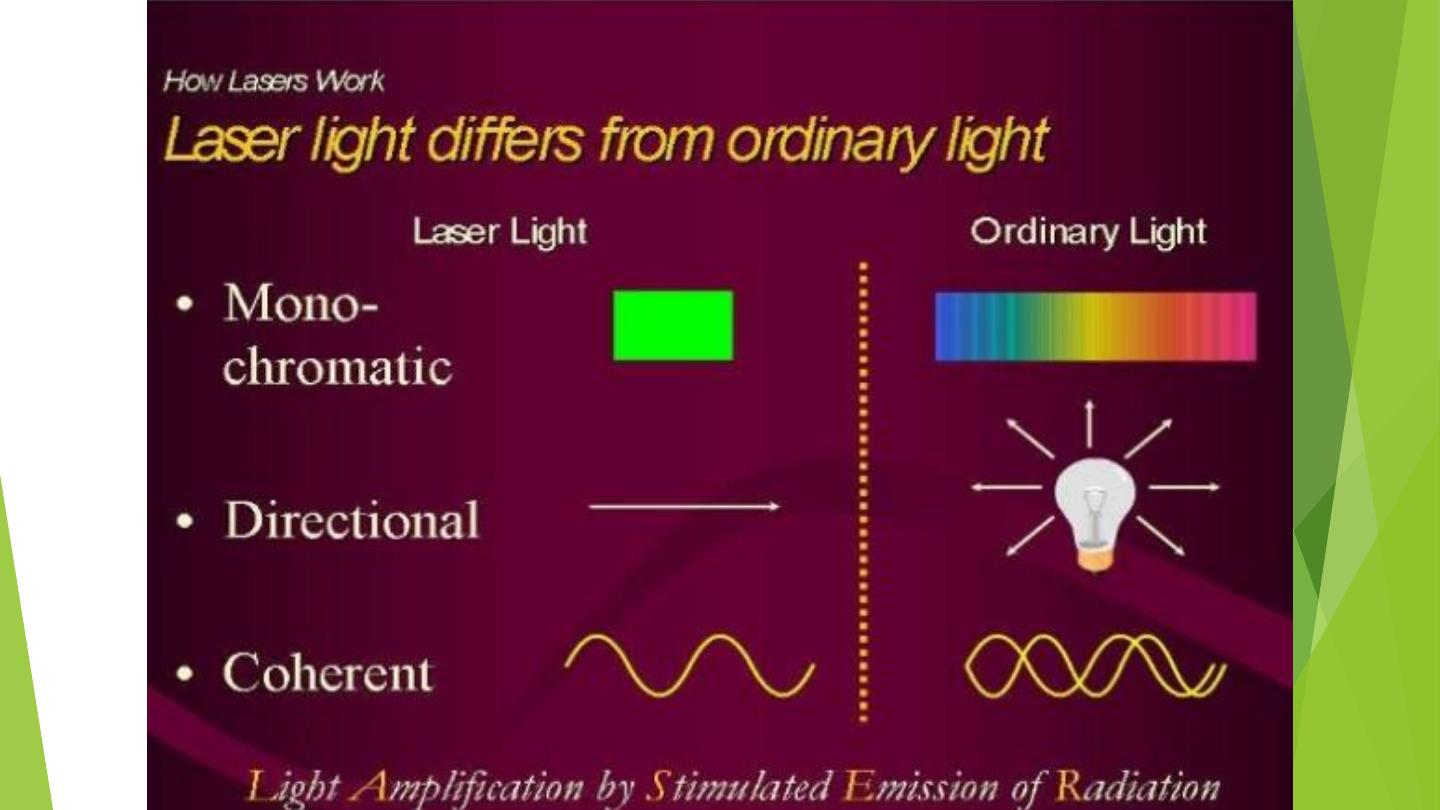
The light waves formed by the laser are a specific form of radiation, or
electromagnetic energy.
It is important to note that the separating line between the
ionizing, cellular DNA mutagenic, portion of the spectrum and
the nonionizing portion is at the
connection of ultraviolet and
visible-violet light.
Thus, either all dental lasers emit a visible-light wavelength or
an invisible, infrared-light wavelength in the portion of the
nonionizing spectrum called thermal radiation.
C. Radiation

Laser Operation Modes
Once the laser is produced, its output power may be delivered in the
following modes
a- Continuous wave is that energy that emitted constantly for as long
as the laser is activated. Co2 and diode lasers run in this manner
b- pulsed wave The pulsed lasers can be further divided into gated and
free-running modes .
I. Gated-pulse mode, meaning that there are periodic alternations of the
laser energy, similar to a blinking light.
This ―gating‖ helps to minimize
some of the unwanted remaining thermal damage generally associated
with continuous wave laser.
Some instruments can produce pulses as
short as microseconds (μsec) or milliseconds (msec).
II. Free running pulsed mode is produced by a flash lamp, where true
pulses originate from the instrument. Nd:YAG, Nd:YAP, Er:YAG, and
Er,Cr:YSGG devices work as free running pulsed lasers

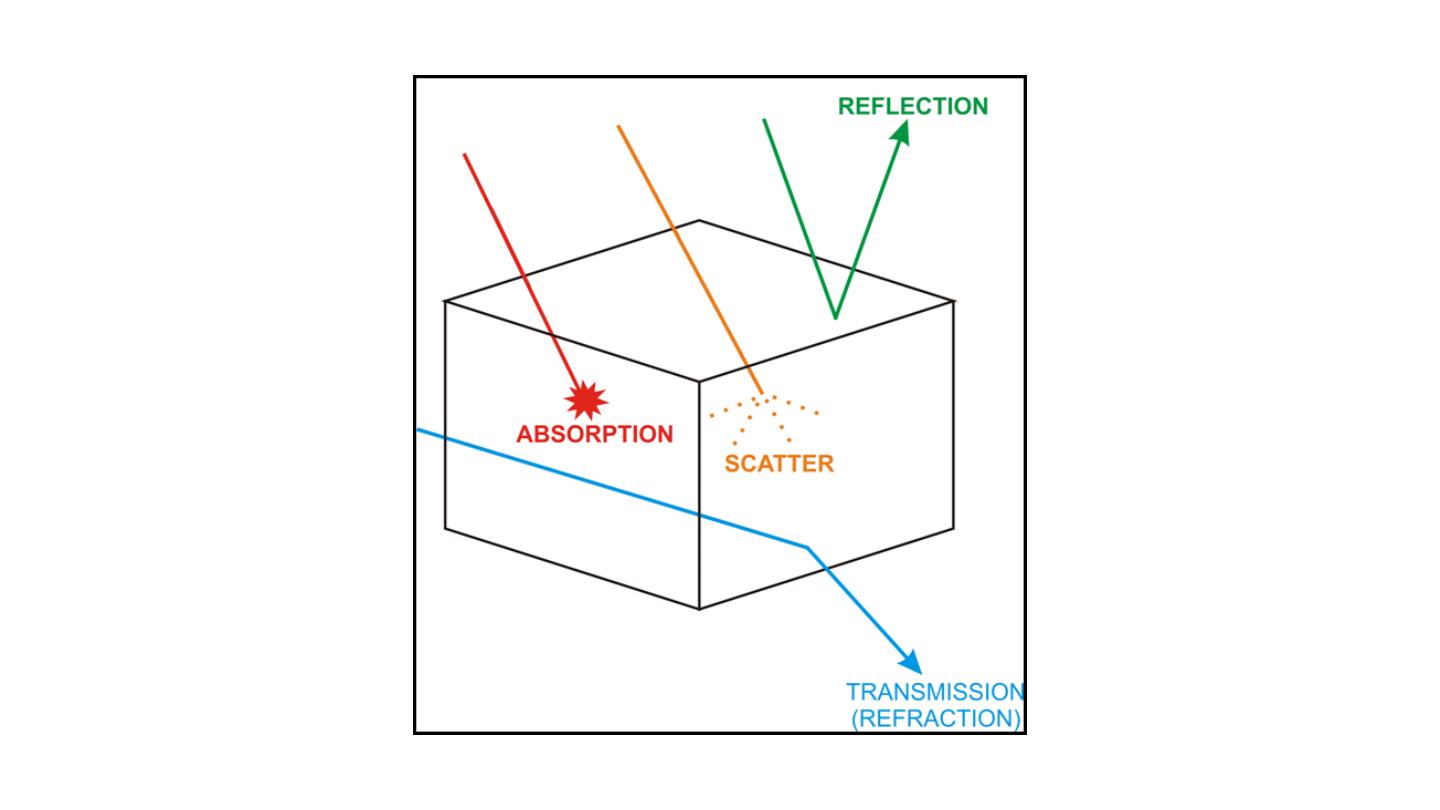
Laser – Tissue Interactions
According to the
optical properties of the tissue
, the light energy from a laser may have four
different interactions with the target tissue .
Reflection:
Reflected light bounces off the tissue surface and is directed outward. Energy
dissipates after reflection.
Transmission:
Light can also travel beyond a given tissue boundary. Transmission irradiates the
surrounding tissue, which must be quantified. Its effects should be considered before laser
treatment can be justified.
Scattering:
occurs when the light energy bounces from molecule to molecule within the tissue.
It distributes the energy over a larger volume of tissue, dissipating the thermal effects.
Absorption:
occurs after a characteristic amount of scattering and is responsible for the
thermal effects within the tissue. It converts light energy to heat energy. The absorption
properties of tissue and cells depend on the type and amount of absorbing pigments or
chromophores. E.g. Hemoglobin, water, Melanin, Cytochromes etc.

1. Photoablative reactions
Occur when molecular bonds are divided. The ruby laser, for example, can split the molecular
bonds of tattoo ink with minimal local thermal damage.
Macrophages remove the tattoo ink after
the molecular bonds are broken.
2. Photochemical reactions
Occur when infrared, visible or ultraviolet laser light interacts with
photosensitizers to produce
chemical and physical reactions.
This forms the basis for photodynamic therapy.
3. Photomechanical effect
Occurs when the laser energy is pulsed to disrupt tissue or stones by the mechanism of shock waves.
An example of this mechanism would be the use of the Holmium YAG laser to shatter ureteric and
renal calculi.
Reaction of Laser with Living Tissue
The reaction of laser energy with living tissue can be photoablative, photochemical,
photomechanical or photothermal. Most lasers react with a combination of all these
mechanisms although for a specific wavelength and delivery system one form of
tissue reaction may predominate.

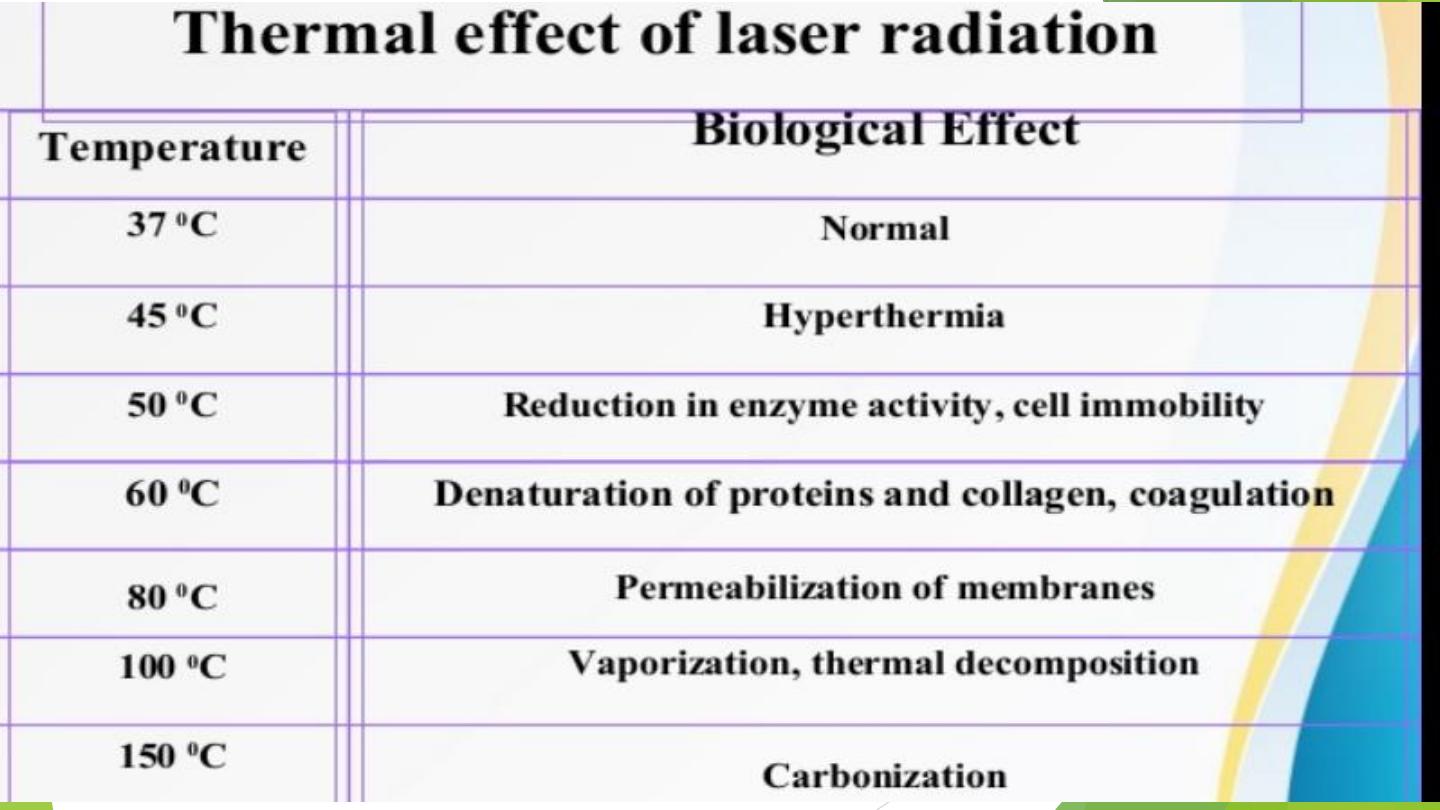
The conversion of absorbed laser light into heat is a photothermal reaction. The tissue effect can be
cutting, coagulation or vaporization depending on the laser wavelength and the laser delivery
device. The heat in the tissue produces a series of changes in the tissue as the temperature rises. The
changes are denaturation, coagulation, vaporization, carbonization .
4-photothermal reaction
When laser light strikes tissue, it scatters until all the laser energy is either
absorbed or reflected. The absorption of laser energy heats tissue. The
volume of tissue affected is larger than the area shown by the laser spot
size. The depth of penetration by a given wavelength of laser light is
determined by the absorption and scattering of the type of tissue and the
wavelength of the laser.

Potential advantages of laser
1. No-touch techniques that ensures sterile surgical site.
2. Reduced blood loss. •
3. Limited fibrosis and stenosis. •
4. Fiber optic delivery. •
5. Potential reduction in spread of metastasis by sealing lymphatic
vessel and killing of malignant cells
6. Fewer instruments in the field.
7. Reduce post-operative pain.
8. Sterilization of the impact site.
9. Dry surgical field.
10. Reduced edema

Potential Hazard of Laser Machine
1. Hazard to eye: corneal or retinal burns (or both). Chronic exposure to excessive levels
may cause corneal or retinal injury
2. Hazard to skin: Sever burns & scarring.
3. Electrical hazard: High voltage – life threatening. 4. Fire :
4. The solvents used in dye lasers are flammable. High voltage pulse or flash lamps may
cause ignition.
Possible Complications of Laser Therapy
1. persistent erythema(2-3 months).
2. oedema1. persistent erythema(2-3 months).
3. 2. Pigmentary changes: hyper / hypopigmentation.
4. Textural change, atrophy.
5. Scarring, keloid.

Laser Light Delivery
Articulated arms-CO2 laser
Fiber optic delivery system

Erbium lasers
The erbium group of dental lasers consists of two wavelengths with similar but not identical
properties.
The erbium:yttrium-aluminum-garnet (Er:YAG) laser produces a wavelength of 2940 nm
and the
erbium, chromium:yttrium-scandium-gallium-garnet (Er,Cr:YSGG) laser produces a
wavelength of 2780 nm

Many advantages has been proposed in using the laser over the traditional method of bone
cutting like
no vibration and mechanical defects,
no bone powder,
easy control , more precise and comfortable
, and clear visual field.
The ideal laser for bone cutting would be capable of high ablation rate with high pulse
repetition rate to remove large tissue volumes in a short time, and at the same time would be
capable of minimizing peripheral thermal injury around the cuts to prevent delayed wound
healing.
advantages

Mode of laser Using
A. Focusing
Lasers can be used either in a focused mode or in a defocused
mode. A
focused mode
is when the laser beam hits the tissue at
its focal points or smallest diameter.
B. Defocused mode.
By defocusing the laser beam or moving the focal spot away
from the tissue plane, this beam size that hits the tissue has a
greater diameter, thus causing a wider area of tissue to be
vaporized. However, laser intensity / power density is reduced
C. Contact mode
The fiber tip is placed in contact with the tissue. The charred
tissue formed on the fiber tip or on the tissue outline increases
the absorption of laser energy and resultant tissue effects

In considering, the biologic effects of laser light on, hard tissue there are
many factors to consider. These factors include
1-the specific wavelength of the laser,
2-the energy density,
3- pulse duration of the laser radiation,
and the properties of the tissue interacting with the light.
These properties include absorption, transmission, scattering, and reflection
of the laser energy. All erbium lasers share a common characteristic of an
affinity for the wave lengths to be highly absorbed by water, hydroxyapatite,
and collagen
The optical penetration depth of the erbium lasers (Er:YAG and
Er,Cr:YSGG) are only a few micrometers.

Nowadays, different laser wavelengths are available, but only the mid-infrared (MIR),
erbium, chromium:YSGG 2,780 nm and the erbium:YAG 2,940 nm lasers are useful for
treating hard dental tissues, due to their selective absorption by water and hydroxyapatite
Mechanism of Action of Erbium Laser
Erbium lasers are unique in that they are the only lasers that can cut both hard and soft
tissues. The erbium lasers‘ ability to remove composite restorations is due to their
photonic absorption in the water that exists within all composite restorations.
Hard
tissue ablation results from micro-evaporative expansive events that occur
within the target due to an extremely rapid buildup of heat and spontaneous
evaporation of the available water content.
This process also is referred to as a
thermomechanical effect
due to the pressure
buildup involved. This type of laser/tissue interaction results in a characteristic popping sound.


Carbon dioxide (CO
2
) lasers
continue to be a major instrument for soft tissue surgery for excellent affinity to
water-based tissues. The wavelength of 10,600nm is readily absorbed by water thus,
it will not penetrate far into tissues (0.1-0.23mm) without repeated or prolonged use
making it ideal for superficial lesions and resurfacing of the skin. It is also used for
removal of the sialoliths.
Nd:YAG lasers
(1064nm) are used for hair removal, in addition for removal of
tattoos and pigmented lesions . Nd:YAG and Ho:YAG (2.12μm) are frequently used
in bone and cartilage ablation.
Photons are produced by electric current with wavelengths of 810, 940 and 980nm.
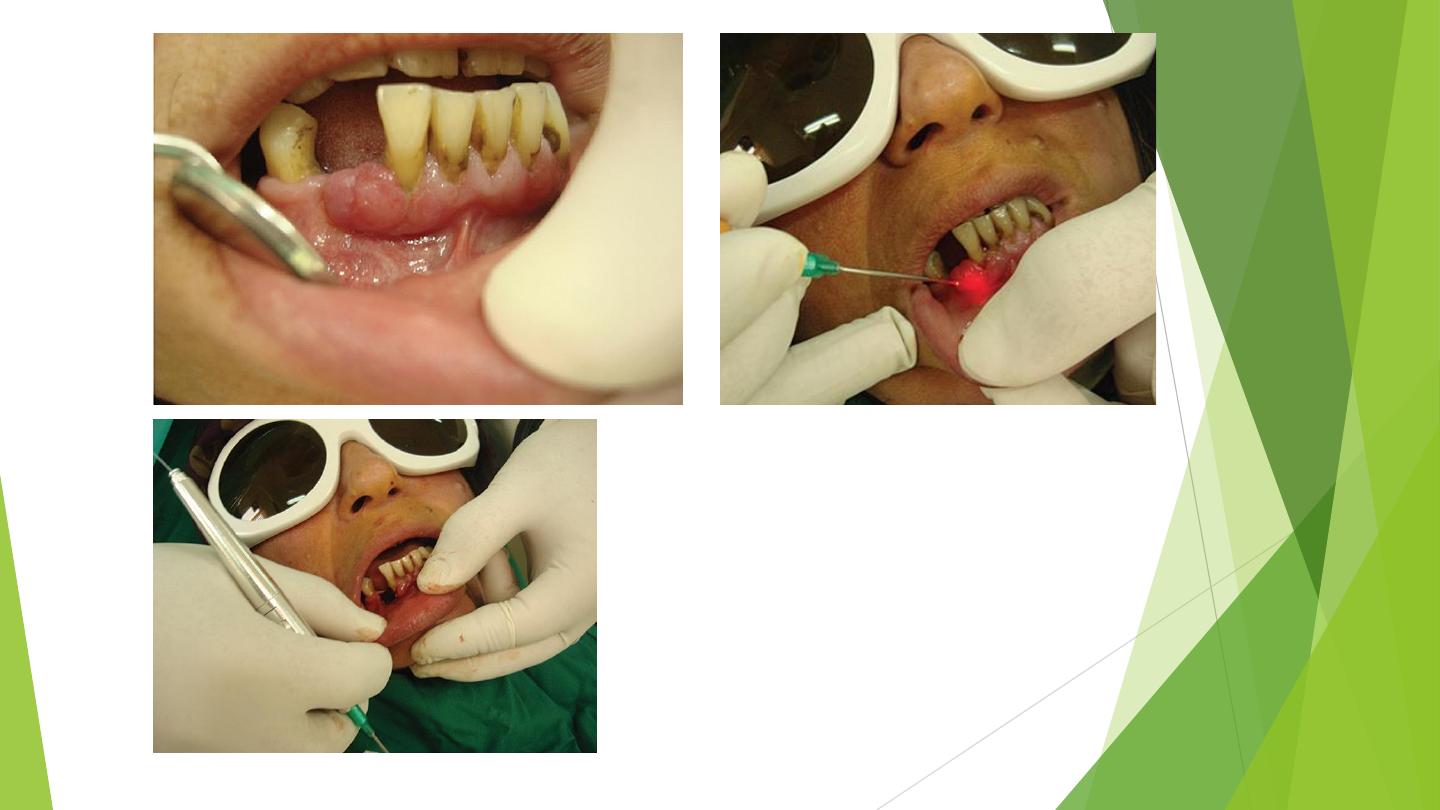
The application of diode laser in soft
1-facial pigmentation
2- vascular lesions and in oral surgery excision; for example frenectomy, epulis fissuratum and
fibroma.
The advantages of laser application are that it provides relatively bloodless surgical and post
surgical courses with minimal swelling and scarring. We used diode laser for excisional biopsy of
pyogenic granuloma and gingival pigmentation.
Diode laser