Maxillary Sinus disease
Dr. Wafaa Khalil
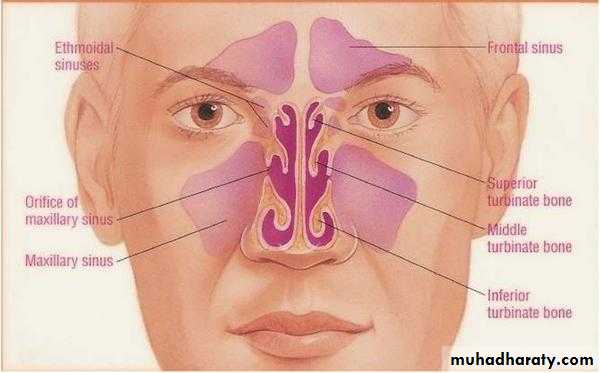
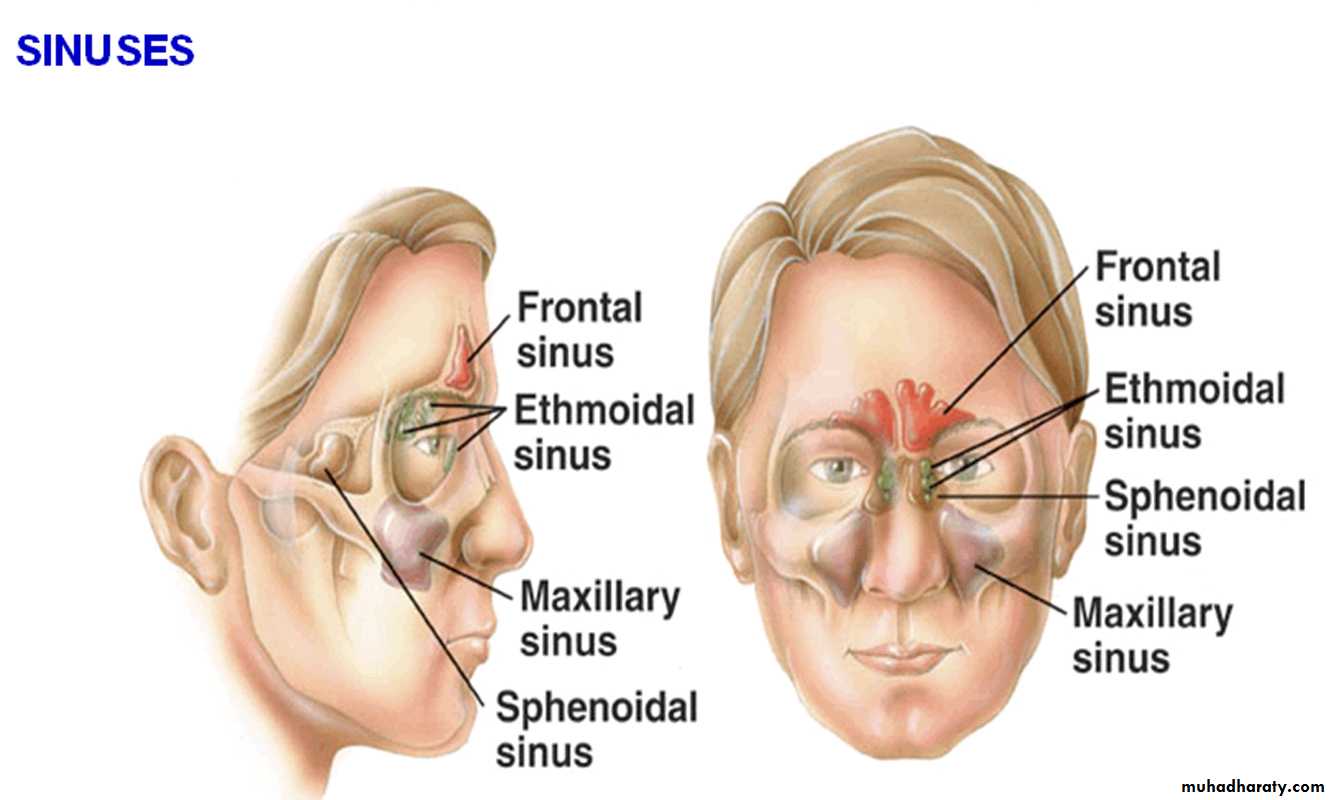
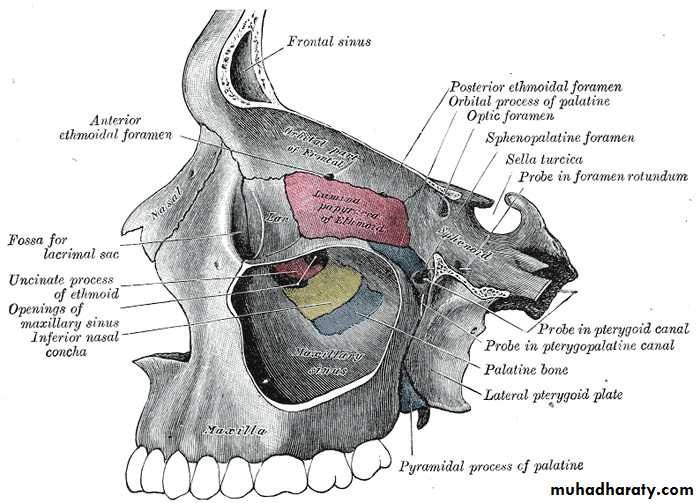
The maxillary sinus is a pneumatic space. It is the largest bilateral air sinus located in the body of the maxilla and opens in the middle nasal meatus of the nasal cavity with single or multiple openings are termed ostium maxillare, which found in a recess called hiatus semilunaris..
Maxillary Sinus
(Antrum of Higmore)The average dimensions of the sinus are approximately 3.5 (anteroposterior) x 3.2 (height) x 2.5 (width) cm
The average capacity of the maxillary sinus is about 15 ml
Development:• The maxillary sinuses are the only sizable sinuses present at birth
• They develop at the third month of intrauterine life, in the place existing between the oral cavity and the floor of the orbit.
• The maxillary sinus enlarges variably and greatly by pneumatization until it reaches the adult size by the eruption of the permanent teeth.
• Enlargement of the maxillary sinus is consequent to facial growth.
• Growth of the sinus slows down with decline of facial growth during puberty but continues throughout life.
Anatomy:
The maxillary sinus varies greatly in size, shape and position not only in different individuals but also in different sides of the same individual.It is pyramidal in shape having a base, an apex and four walls:
The base: lateral wall of the
nasal cavity.
The apex: directed laterally
towards the zygomatic
process of the maxilla.
The four walls:
• Anterior wall: facial surface of the maxilla.• Posterior wall: infratemporal surface of the maxilla.
• Roof: floor of the orbit.
• Floor: alveolar process of the maxilla.
Function of the maxillary sinus:
1. Lightening the weight of the skull.2. Resonance of voice.
3. Olfactory and respiratory modulations through regulation of the air pressure within the sinus during respiration.
4. Inspired air conditioning.
5. Craniofacial protection against mechanical trauma.
6. Production of the bactericidal enzyme (lysozyme) which may be significant in protection against bacterial infection of the nasal mucosa.
Blood Supply
Blood supply to the mucous membrane is from arteries which pierce the bone; and are derived from facial, maxillary, infraorbital and greater palatine arteries.
The veins accompany the arteries, and drain into anterior facial vein and then to pterygoid plexus of veins.
The lymphatic drainage of maxillary sinus is through the infraorbital foramen or through the ostium and then to submandibular and deep cervical lymph nodes.
Nerve Supply
From superior dental nerves (anterior, middle and posterior), and the greater palatine nerve.
Physiology
The sinuses are lined by respiratory epithelium; namely, the mucus secreting; pseudostratified, ciliated, columnar epithelium. It is also known as schneiderian membrane.
The mucociliary mechanism is useful means for removal of particulate matter, bacteria, etc. The cilia move the mucus and other debris towards the ostium
and subsequently discharged in the middle meatus.
Clinical considerations
• Nerves that supply maxillary teeth are those that supply the maxillary sinus accounting for dental pain from healthy teeth arising from maxillary sinusitis.2. Bone forming the floor of the sinus can also be the bone surrounding the apex of a tooth. Consequently periapical infection of teeth can spread to maxillary sinus. The reverse can occur with maxillary sinus infection being perceived as originating from teeth.
3. Pain from carious lesion or other insults to the dental pulp may be referred to the sinus.
4. Accidental communication between the sinus and oral cavity may occur during tooth extraction or surgical procedures leading to oroantral fistula.
5. Roots of maxillary posterior teeth may have close relationship to the floor of the maxillary sinus. Molars are more related than premolars in the following order: second molar were closest to the floor. The next in order of frequency were; first molar, third molars, second premolar, first premolar and rarely the canine.
Classification
• Infections– Acute maxillary sinusitis
– Chronic maxillary sinusitis
• Cysts
– Antral lining cyst
– Odontogenic cyst
• Bone dysplasias
– Fibrous dysplasia
– Paget’s disease of bone
• Malignant tumors
– Squamous cell carcinoma– Osteosarcoma
• Invasive tumors
– Salivary gland tumors/ Adenocarcinoma
– Basal cell carcinoma
• Benign tumors
– Ossifying fibroma
– Osteoma
– Odontogenic tumors
– Adenomas
MAXILLARY SINUSITIS
Infection or Inflammation of
the maxillary sinus
Although the term sinusitis is commonly in use, the process may more accurately be described by the term rhinosinusitis because the nasal and sinus mucosal surfaces are contiguous and it would be impossible to have sinusitis without a coexisting rhinitis.
Sinusitis Classification
ACUTE SINUSITIS < 3 weeksSUBACUTE SINUSITIS 3 weeks-3 months
CHRONIC SINUSITIS > 3 months
Etiologic Organisms
Aerobic bacteriaStrep. pneumoniae (30)
Alpha & beta hemolytic Strep
Staph. aureus
Hemophilus influenzae (25 to 30)
Escherichia coli
Anerobes (10 % acute, 66 % chronic)
Peptostreptococcus, Propionobacterium, Bacteroides, Fusobacterium
Fungi (2 to 5)
Viruses (5 to 10)
SYMPTOMS
Nasal obstruction/blockage
Headache
Fever in acute condition only
Yellow or green-coloured mucus from the nose
Swelling of the face
Aching teeth in the upper jaw and facial pain / pressure
Loss of the senses of smell and taste (Hyposmia/anosmia)
Persistent cough due to postnasal drip
Halitosis
Generally feeling unwell
ETIOLOGY
Allergic responseschemical irritation
Infections mechanical obstruction
Infected maxillary tooth
RISK FACTORS
LocalFrequent cold
Cigarette smoking
Regular use of nasal decongestant sprays
Untreated hay fever or other allergies
Structural abnormalities of the nose
Nasal polyps
Dental disease
Systemic
Diabetes
Immunocompromise (AIDS)
Malnutrition
Blood dyscrasias
Chemotherapy
Long term steroid Rx
Pathogenesis
Basic cause is osteomeatal complex (the middle meatal region & the frontal, ethmoid, & maxillary sinus ostia there) inflammation & infection
Sinus ostia occluded
Colonizing bacteria replicate
Ciliary dysfunction
Mucosal edema
Abnormal quantity or quality of secretion
Lowered PO2 & pH
MAXILLARY SINUSITIS
FROM DENTAL ORIGIN1.Periapical abscess : secondary to direct extension of infectious or inflammatory processes through the apices of maxillary teeth into the sinus
2.Periodontal diseases: communication with the maxillary sinus via a periodontal pocket
3.Infected dental cyst: most common of all cysts of the oral region, cyst originate from epithelium rest of Malassez
4.Dental material in antrum: 1.Displacement of root extraction of third molar > second molar > canine
PA or occlusal film loss of lamina dura
2.Implant
3.Root canal overfilling
Infection following a sinus lift procedure appears to be more likely when there is preexisting osteomeatal inflammation
5.Oroantral communication: causes
Extraction Trauma
Tumour Cyst
Complications of Acute Sinusitis
• Periorbital, frontal, or cheek edema
• Proptosis
• Ophthalmoplegia
• Ptosis
• Diplopia
• Meningeal signs
• Neuro deficits of cranial nerves II to VI
Clinical Examination of Maxillary Sinus
a. Extraoral examination: Pain and tenderness, swelling over the prominence of cheek bonesb. Intraoral examination:
• Pain and tenderness, swelling over the maxilla between the canine fossa and the zygomatic buttress.
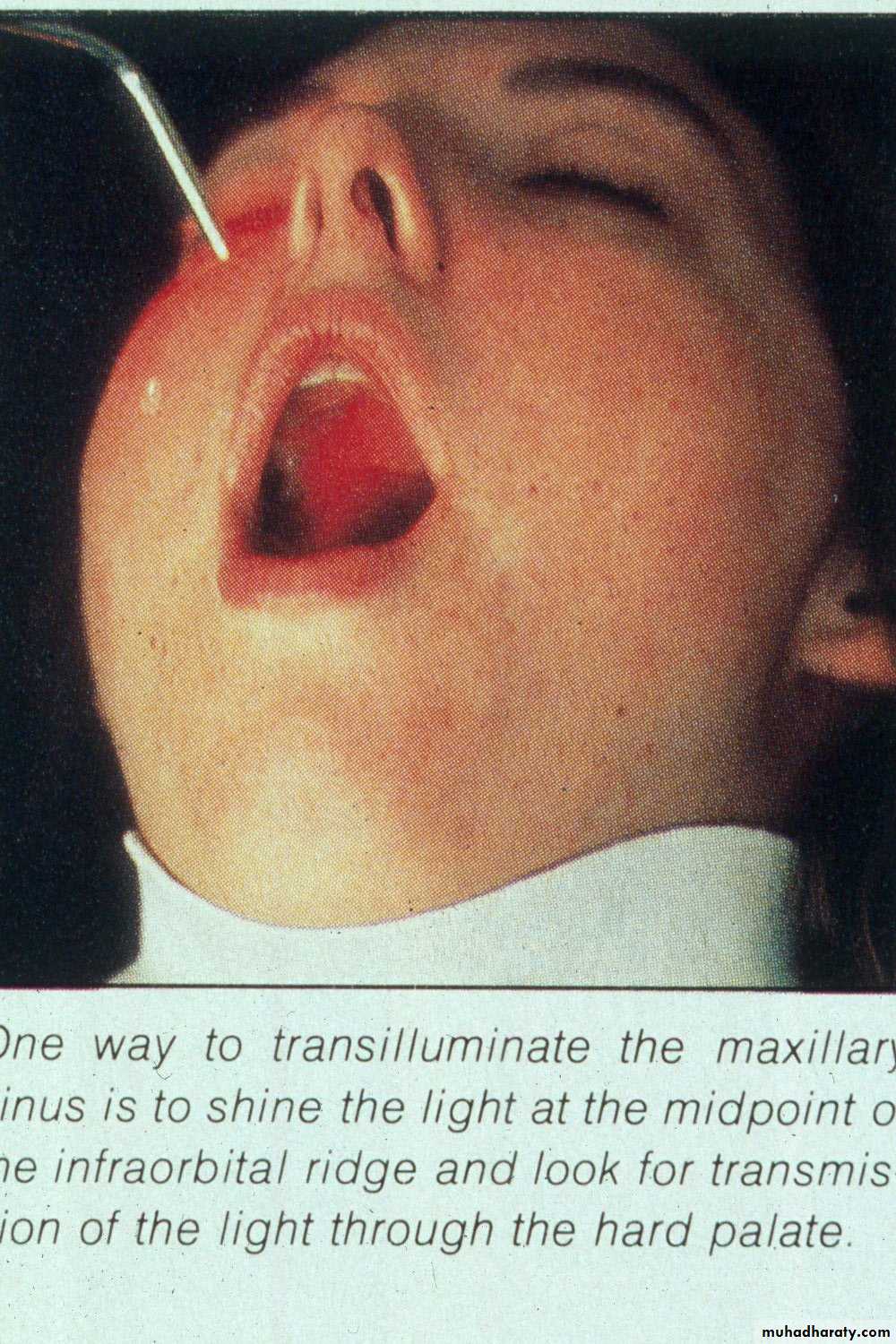
• Transillumination: The affected sinus shows decreased transmission of light; due to accumulation of fluid, debris, pus, and thickening of the sinus mucosa.
Use of Paranasal Sinus Transillumination to Diagnose Sinusitis
It is one of the methods of examination, and can be carried out because of the relative thinness of the walls of the maxillary sinus.• First remove patient's dentures
• Use darkened room
• Placing a strong light in the center of mouth of the patient with the lips closed.
• The results of a normal sinus will be a definite infraorbital crescent of light, a brightly lit eye and glowing pupil. Or it can be done as;
• Shield light source from observer's eyes
• Shine light over max. sinus & observe light transmission through hard palate
• Report results as opaque, dull, or normal for either side
• Less accurate method than conventional radiography
Radiology of Maxillary Sinus
• Extraoral views:• Occipitomental View (15° OM): it’s called Water’s view. The presence of pus will produce a horizontal fluid level in this view; provided that there is air above it. As a measure of confirmation of the diagnosis, the view is repeated with the head tilted toward the side of pathology. The fluid level remains horizontal.
• Lateral Skull: (i) confirming the presence of fluid level and cyst (ii) in localizing a foreign body, e.g. root; particularly when the foreign body is located higher up in the sinus.
• Submentovertex View: This view is helpful in visualizing the posterior walls of maxillary sinus.
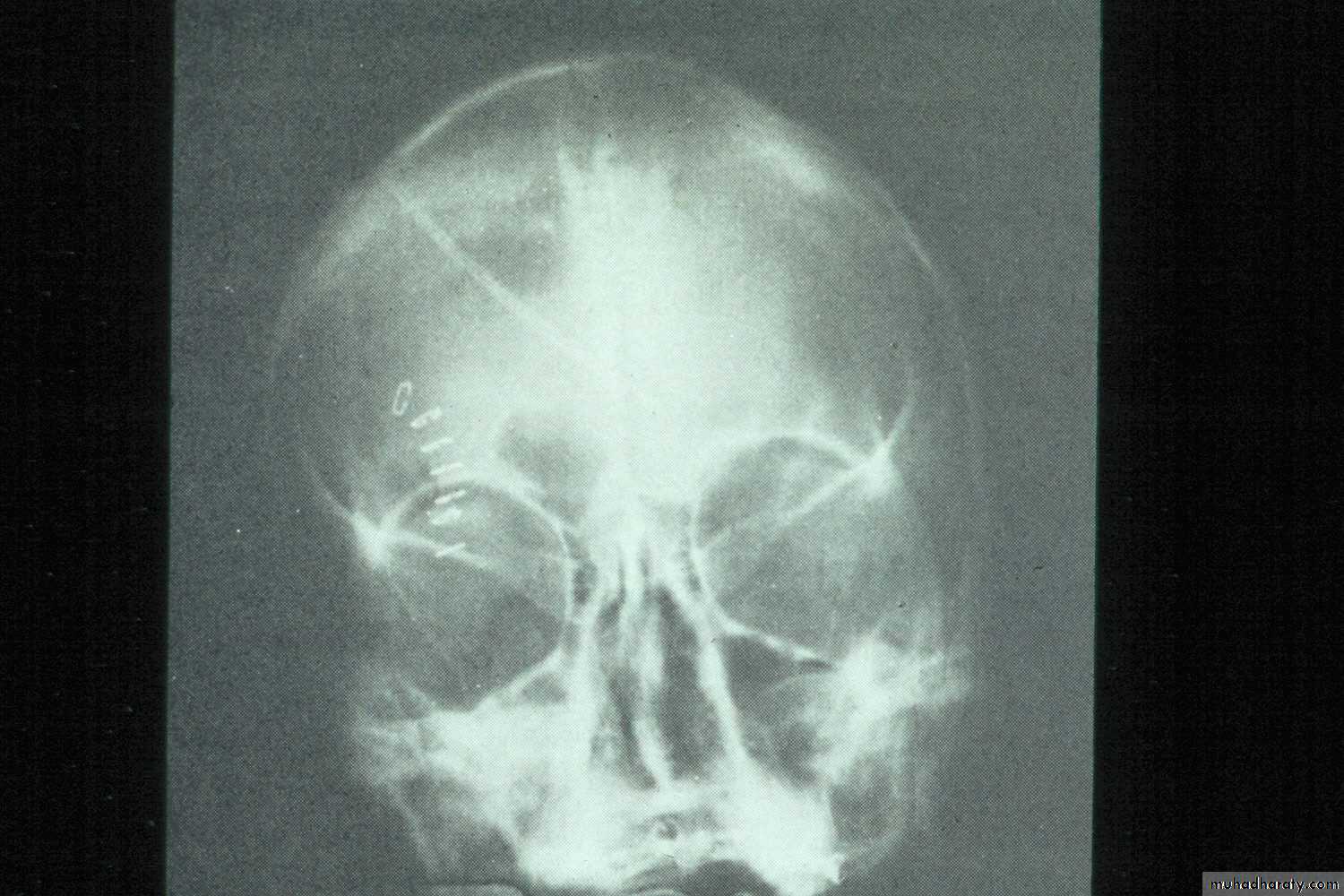
d. Occipitofrontal View: Is recommended to detect multisinusitis,
pansinusitis, if present.e. Tomography:This technique provides details of sinus structure.
(i) Solid masses within maxillary sinus such as osteoma; andantroliths,
(ii) early erosion of walls of maxillary sinus from malignant diseases.
f. Orthopantograph: is helpful in routine detection of lesions such as odontogenic and mucosal cysts of maxillary sinus.
2. Intraoral Views: (i) locating and retrieving foreign bodies in the sinus such as: teeth, roots, osseous fragments.
(ii) Careful planning of their surgical removal.
Acute Sinusitis
Radiography
Radiographic signs of sinus pathology :
Air fluid levels
Partial or complete opacification
Bony wall displacement
4 mm or more of mucosal wall thickening
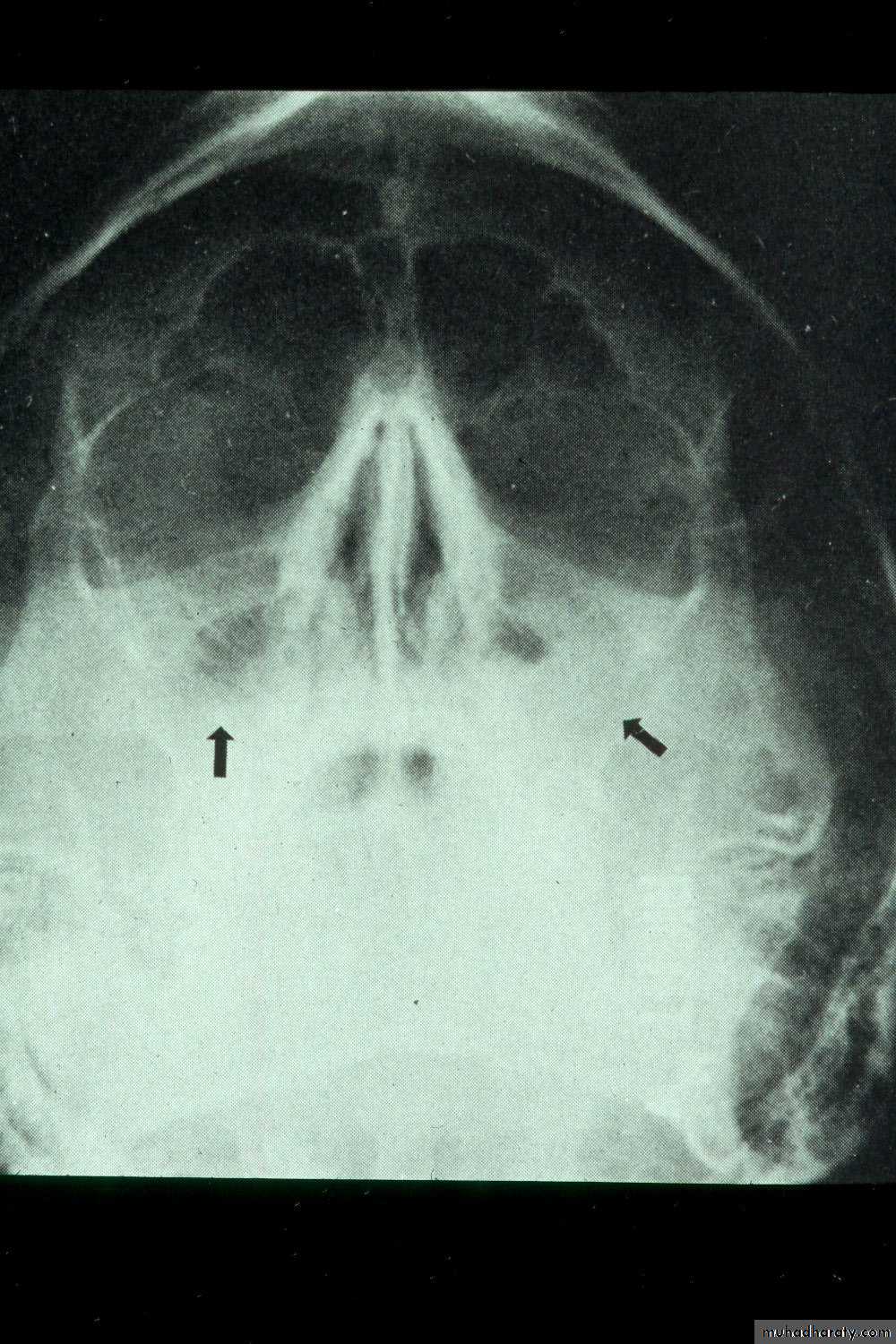
Water’s view with air-fluid level in left maxillary sinus
Water’s view showing air-fluid level in right maxillary sinus and mucosal thickening in left maxillary sinus
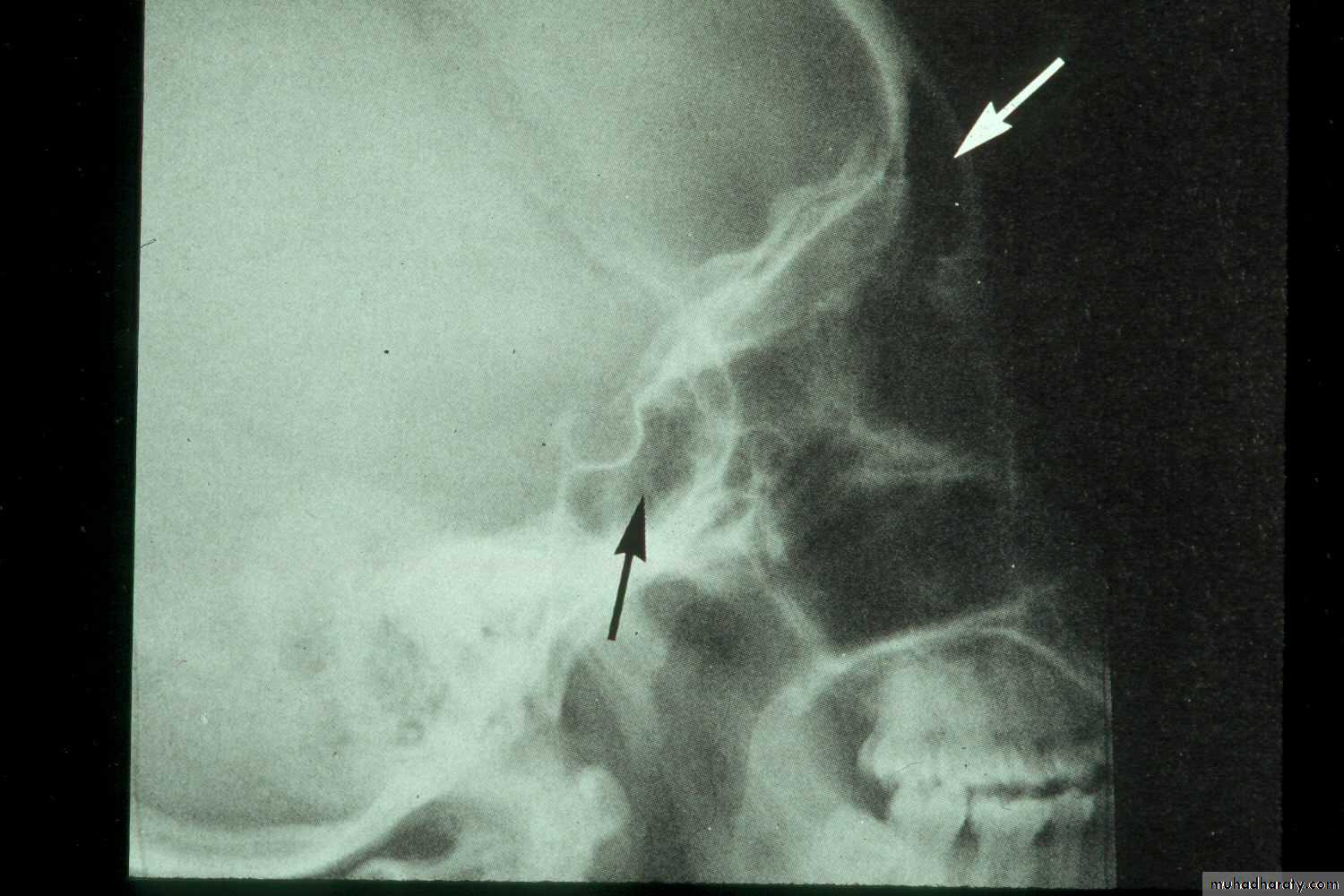
Lateral view of normal frontal and sphenoid sinuses
Hypoplastic left frontal sinus and nosocomial right maxillary sinusitis
Use of Computed Tomography (CT) for Diagnosis of Sinusitis• Advantages of CT :
Visualizes ethmoid air cells
Evaluates cause of opacified sinus
Differentiates bony changes of chronic inflammation from osteomyelitis
• Indicated only if complications suspected or if diagnosis uncertain (not needed initially for most cases)
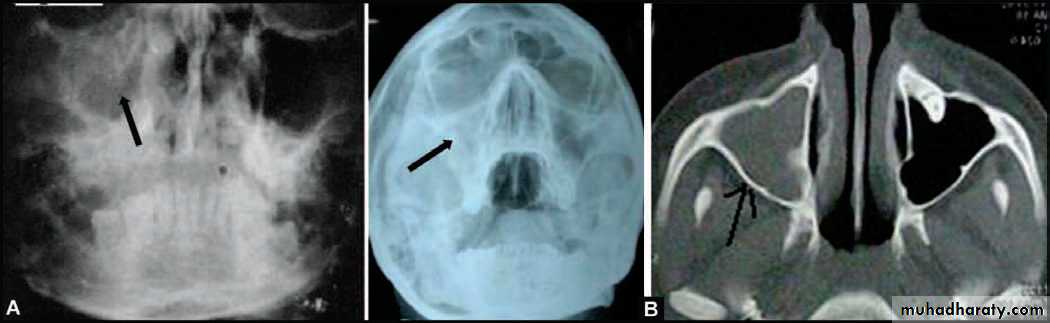
(A) PA view of Water’s position showing haziness of the (R) maxillary sinus, following extraction of upper right first molar 3 months back. Chronic maxillary sinusitis with oroantral fistula (B) PA view Water’s position and CT scan picture of another patient showing complete haziness of (R) maxillary sinus, indicating chronic maxillary sinusitis
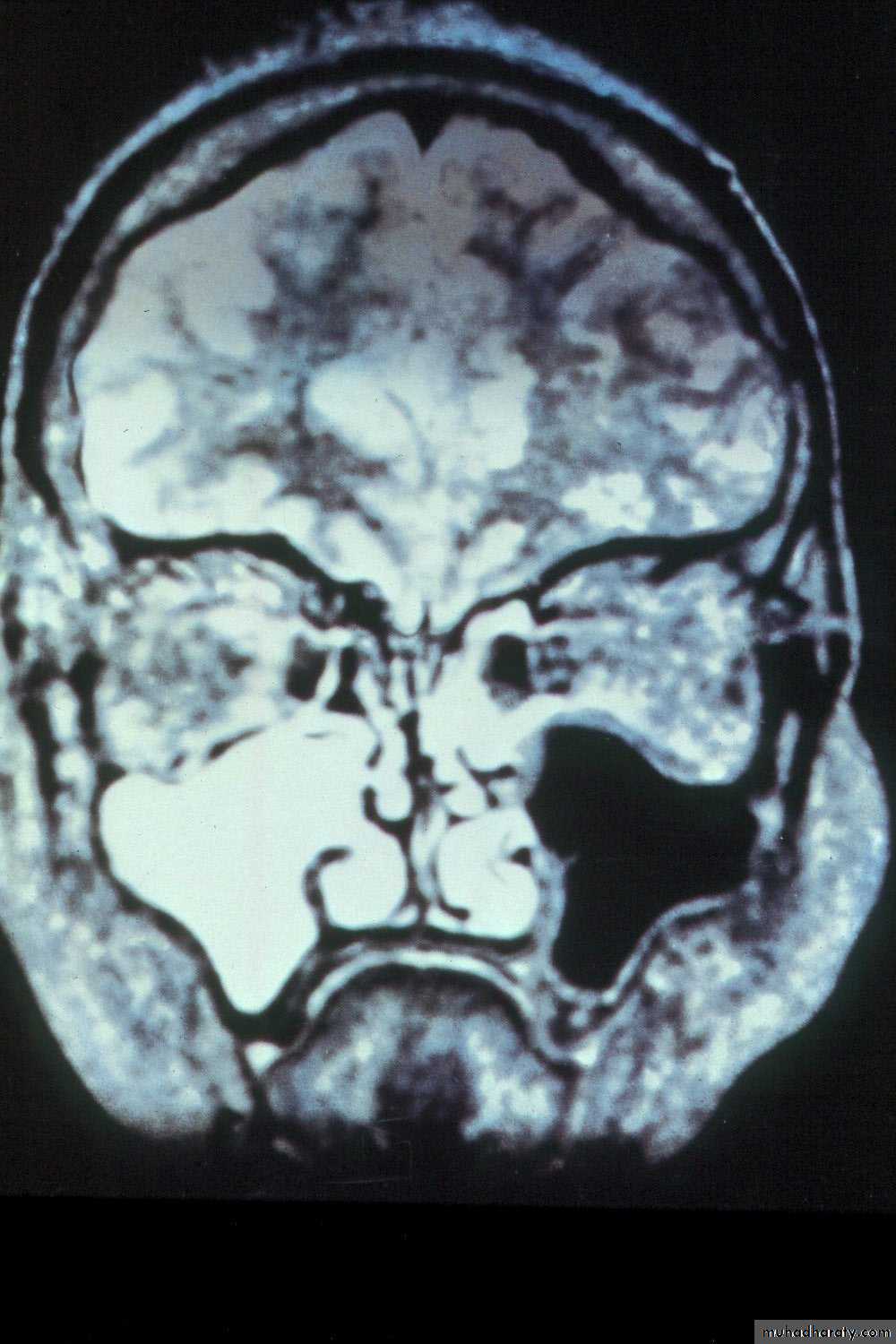
Coronal MRI scan showing maxillary sinusitis
Another diagnostic modality for sinusitis is nasal endoscopyView into left nasal cavity demonstrates a polyp (P) extending from the middle meatus.
p
Purulent discharge from the middle meatus draining into the nasopharynx adjacent to the eustachian tube orifice.
Aspergillus fungal balls of the maxillary sinus. Note the fungal debris and mucosal edema.
Goals of Medical Therapyfor Acute Sinusitis
• Control Infection
• Facilitate sinus ostial patency and drainage
• Provide relief of symptoms
• Evaluate and treat any predisposing conditions to prevent recurrences
General Treatment for
Acute Sinusitis
• Oral antibiotic (Amoxicillin, Augmentin, Azithromycin)
• Topical and systemic decongestants as nasal drops or sprays e.g. Ephedrine sulphate
• Mucolytic agents: These are used to reduce the viscosity
to produce thin mucous secretion e.g.Tinc.benzoin, camphor, menthol, chlorbutol.
• Non-steroidal anti-inflammatory analgesic agents
(i) Aspirin (ii) Paracetamol (iii) Ibuprofen.
• Other medication:
warm nasal saline irrigations
Antihistamine orally : only in the small % of patients with true allergic component
• Oral steroid therapy can be used intermittently in patients with chronic sinusitis to manage acute exacerbations.
. Prednisone or methylprednisolone is used. Doses usually
begin at 30 mg daily are tapered over 2 to 3 weeks
Surgery (maxillary antrostomy, and Caldwell-Luc operation)
Indications for surgery include
(1) acute sinusitis with a pending or evolving complication,
(2) chronic sinusitis that has failed maximum medical management including at least 3 weeks of broadspectrum
Antibiotics.
(3) most forms of fungal sinusitis.
Surgery is performed under the visualization of endoscopes. The goals of surgery are to remove chronically inflamed tissue and to restore sinus ventilation, drainage, and mucociliary clearance.
Major complications specific to sinus surgery occur in 0 to 5% and include bleeding, CSF leak and visual problems..
Definition
Odontogenic sinusitis is the inflammation of mucosa of any of the paranasal sinuses. Inflammation of most or all of the paranasal
air sinuses simultaneously is known as pansinusitis.
Radiographs will reveal, either a totally opaque sinus or a fluid level.
Odontogenic Sinusitis
Management
• The extraction of the offending teeth carries a risk of perforation and a persistent fistula.
• Antibiotic prophylaxis and taken for at least five days postoperatively
• Decongestants: in the forms of nasal inhalations and drops.
Oroantral Communication and Fistula
Definitiona. An oroantral perforation is an unnatural communication between the oral cavity and maxillary sinus.
b. An oroantral fistula is an epithelialized, pathological, unnatural communication between these two cavities.
The close proximity is usually observed when the maxillary sinus is pneumatized into the alveolar process between the root tips of molars and especially when there are periapical lesions that are in contact with the lower surface of the maxillary sinus.
Aetiology
Oroantral fistula can result from several causes:.1. Extraction of teeth. The root apices of canines, premolars and molars may be also in close proximity to the floor of sinus. Also a conical maxillary third molar, which when grasped with the forceps during extraction, slips into the maxillary antrum along with fracture of the tuberosity. Also forceps
extraction of solitary isolated posterior teeth in an edentulous arch
2. Destruction of the portion of the floor of the sinus by periapical lesions.
3. Perforation of the floor of the sinus and sinus membrane with improper use of instruments.
4. Forcing a tooth or a root into the sinus during attempted removal.
5. Extensive trauma to face.
6. Surgery of maxillary sinus; removal of large cystic lesions encroaching on the sinus cavity.
7. Chronic infection of maxillary sinus, such as osteomyelitis.
8. Teratomatous destruction of maxilla, such as gumma involving palate.
9. Infected maxillary implant dentures, and
10. Malignant diseases such as malignant granuloma
Symptoms: Fresh Oroantral Communication:
• Escape of fluids: From mouth to the nose on the side of extraction.
• Unilateral epistaxis : It is due to blood in the sinus escaping through osteum into the nostril.
• Escape of air from mouth into the nose, on sucking, inhaling or drawing on a cigarette, or puffing the cheeks (Inability to blow cheeks.Passage of air into mouth on sucking).
• Enhanced column of air: Causes alteration in vocal resonance and subsequently change in the voice.
• Excruciating pain: In and around the region of the affected sinus, as the local anaesthesia begins to wear off.
Symptoms of Established Oroantral Fistula:
In late Stage• Pain
• Persistent, purulent or mucopurulent, foul, unilateral nasal discharge from the affected nostril, especially when head is lowered down.
• Postnasal drip : The trickling of the nasal discharge from the posterior nares, down the pharynx.
• Foul or foetid taste and smell.
• Possible sequelae of general systemic toxaemic condition : Fever, malaise, morning anorexia, frontal and parietal headaches and in extreme cases anosmia and cacosmia
• Popping out of an antral polyp : The persistent infection in the antrum may lead to long-standing oroantral fistula, which may be occluded by an antral polyp establishment of chronic
Managment of Recently Created Communication
If the extraction demanded more force, however, the extraction was straight forward, and the examination of roots of the tooth revealed that a part of bony floor of antrum is seen adherent to the tooth, then the operator must examine the socket to establish any tear in the lining of sinus.If the fistula is large, it can be assessed from inspection;
In case, its patency is not obvious, the nose blowing test is useful. Compression of anterior nares, followed by gentle blowing of nose (with mouth open). Escape of air. bubbles, blood or pus, etc. may appear at the oral orifice. The site of recent extraction, should not be explored with an instrument, which lead to breakdown of the blood clot and the seal.
Treatment of Early Cases
Ideal treatment (i) is immediate surgery repair to achieve primary closure, and
(ii) simultaneous antibiotic prophylaxis to prevent sinus infection: Penicillin
and its derivatives until symptoms begin to subside.
(iii) Nasal decongestants: to encourage the drainage of pus and secretions.
(iv) Analgesics: Non-steroidal anti-inflammatory agents.
The immediate primary closure is done by a simple reduction of the buccal and palatal socket walls, to allow coaptation of buccal and palatal soft tissue flaps to close over the defect. A protective acrylic denture or splint can be used to provide a barrier to the inadvertent entry of food particles.
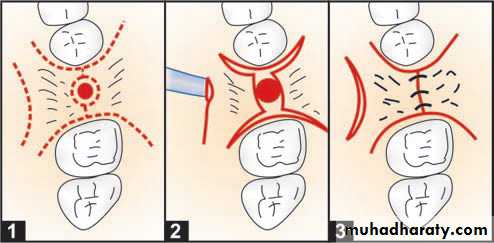
Closure of accidental oro-antral communication in the dentulous arch (1) Incisions are made around the teeth and antral opening. A relaxing incision is made on the palate (2) Mucoperiosteal flaps raised and the buccal and palatal alveolar walls are reduced with rongeur, (3) Interrupte suturing done
Treatment of cases seen more than 24 hours after accident
When a period of 24 hours has elapsed, the soft tissue margins of fistula often get infected. It is preferable to defer the surgical closure until gingival edges show sound healing, i.e. approximately three weeks.Management
The drainage of maxillary sinus is established through the fistula by enlarging it surgically, and the sinus should be gently irrigated daily with normal saline until it is clear.
Supportive medical treatment is instituted. When the acute condition subsides, surgical repair is undertaken.
Surgical Procedures Used in Closure of Oroantral Fistula
(i) Buccal advancement flap
(ii) Palatal rotational flap
(iii) Combination of both.
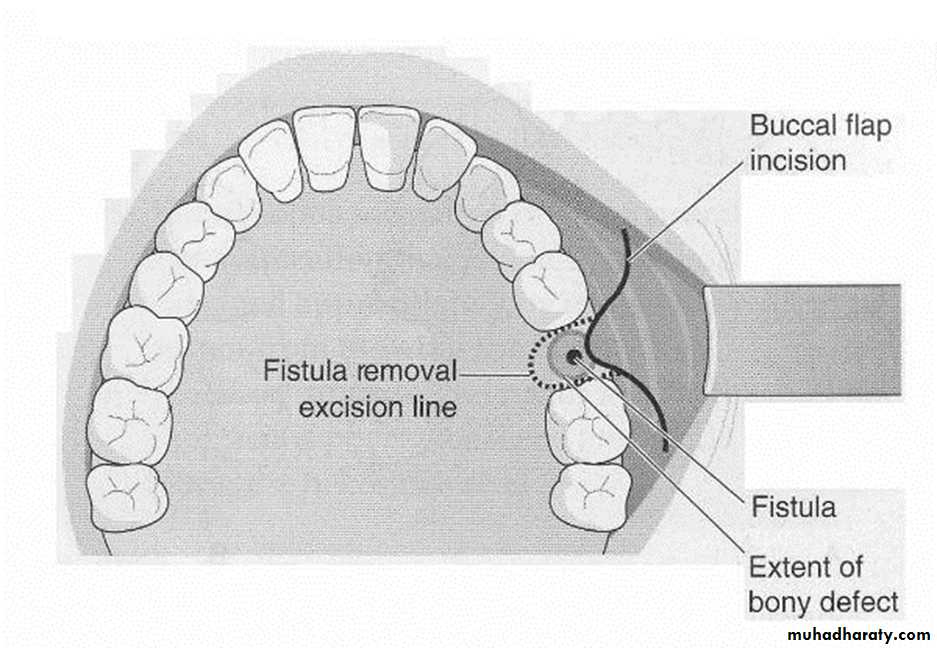
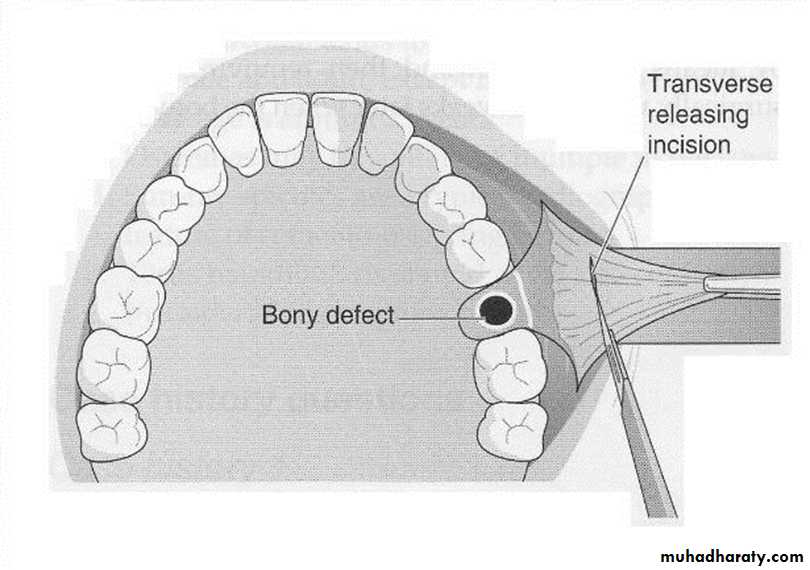
Advancement of buccal flap
General principle of flap design:• The free end of the flap should have an adequate blood supply.
• The buccal flap is so designed, that the base should be wider than the apex; to ensure adequate vascularization at the apex.
• Suture line is well-supported by sound bone.
• Mobilization of either buccal or palatal flap should be done in such a manner that there is no tension on the suture line.
Advancement of buccal flap
The buccal mucoperiosteal flap falls short of covering the fistula; the flap can be advanced. A horizontal incision is made in the periosteum, as high as possible. This will allow advancement of buccal flap.
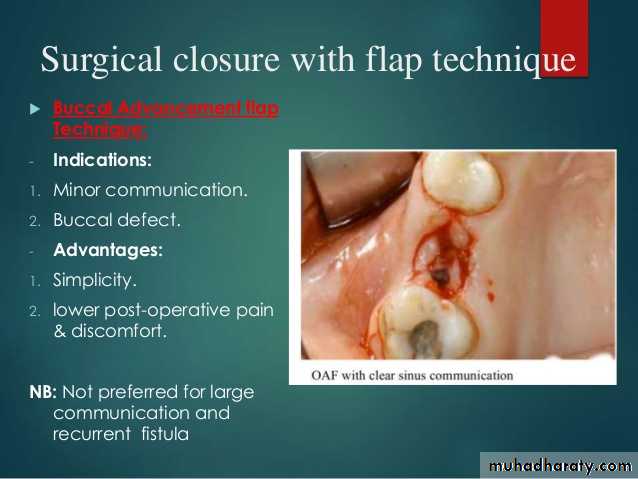
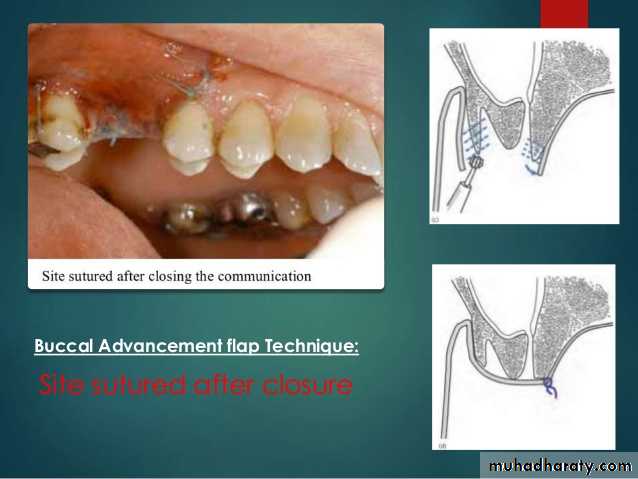
Buccal Advancement flap Technique: -
Indications:
• Minor communication.• Buccal defect.
Advantages:
1. Simplicity.
2. lower post-operative pain & discomfort.NB: Not preferred for large communication and recurrent fistula
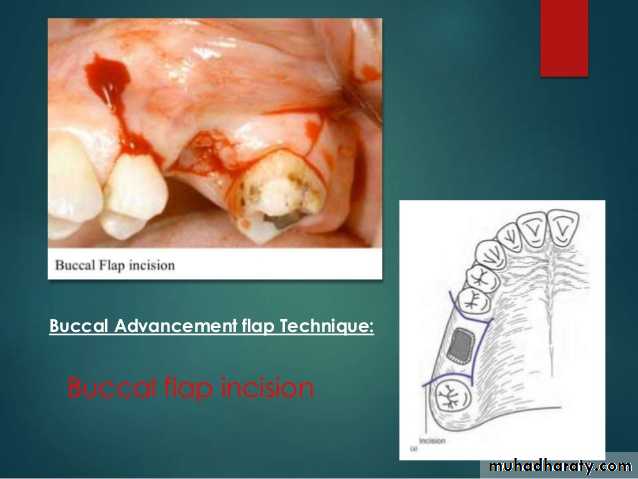
Buccal Advancement flap Technique: -
Disadvantages:• Thin flap dehiscense.
• 2. limited extent.• 3. loss of vestibular depth.
• 4. scaring may cause impaired mobility.
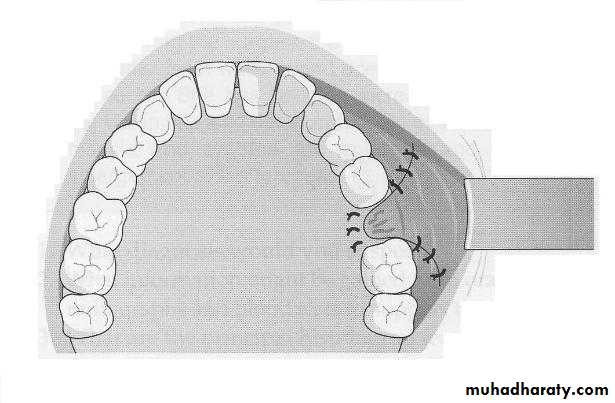
• Then maxillary sinus should be carefully inspected for evidence of infection, either through fistula or by illumination, or with a fiberoptic light. Any polypoidal masses or other diseased tissue should be removed. Antrum gently irrigated with warm normal saline.
• In case, if antral pathology is present, Caldwell-Luc procedure should be carried out before the final closure of fistula.
• After that closure of wound: The mucoperiosteal flap is sutured into position across fistula with interrupted sutures.
• Postoperative medications: (i) Antibiotics, (ii) Analgesics, and (iii)Nasal decongestants and inhalations.
• Restriction to soft diet.
• Instructions to patients: (i) to avoid sneezing, (ii) to explore the wound with tongue, or deliberately sucking air or fluid through it.
• Removal of sutures 7 to 10 days postoperatively.
• Patient is reviewed regularly to observe progress, clinically and radiologically.
Diagramatic illustration of advancement buccal flap
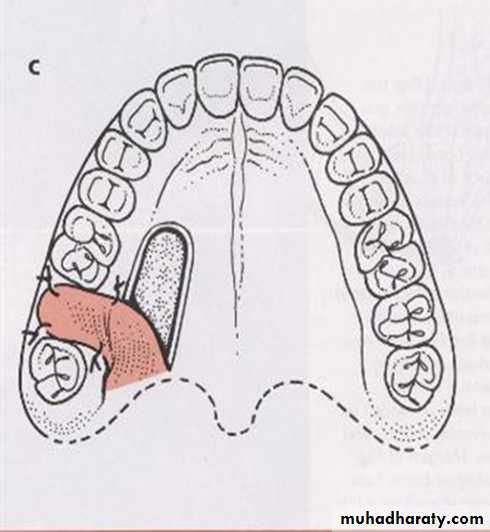
Palatal Pedicled Flap: Rotational Advancement Flap Operation
Advantage:• The palate gets its blood supply from greater palatine arteries.
• Palatal flap is rotated across fistula so that the suture line rests on sound bone on buccal side of the orifice.
• The abundant blood supply in the palatal tissue promotes satisfactory healing.
• Firmer and more resistant to trauma.
• Provides adequate mobility and tissue bulk to the flap.
• Do not affect the buccal vestibular height.
Palatal Pedicled Rotational Flap technique
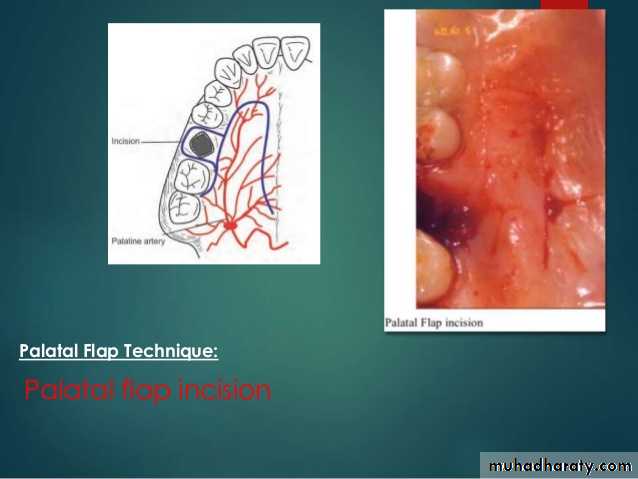
Palatal flap incisionPalatal Pedicled Rotational Flap technique
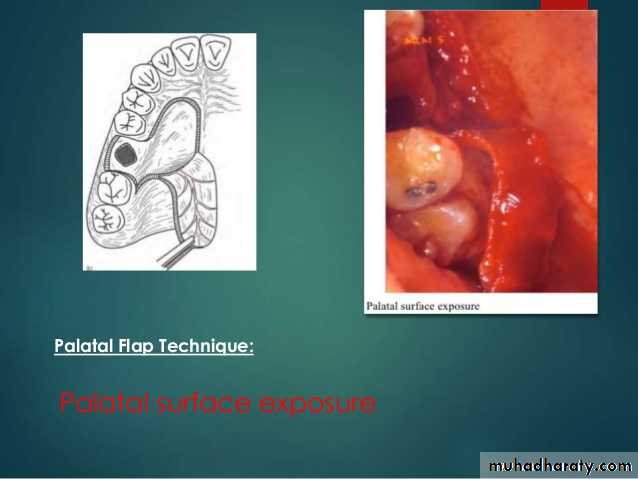
Palatal surface exposure
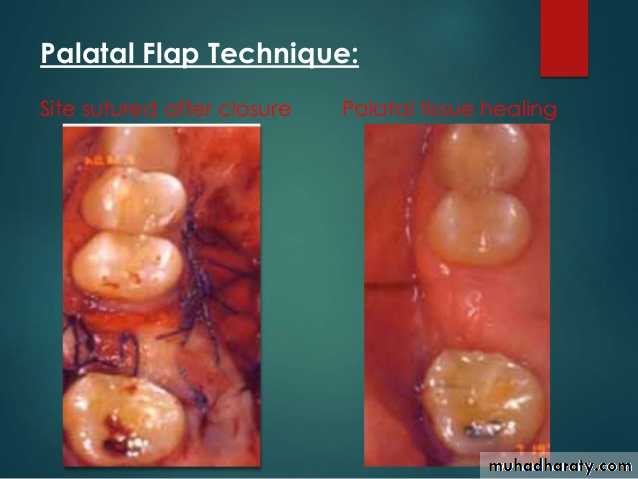
Site of suture after closure
Palatal tissue healingPalatal Pedicled Rotational Flap technique
Disadvantage
1- Denudation of palatal surface .2- Greater post-operative pain.
3- More difficult than buccal flap
4- Appearance of roughness at doner site (epithilization)
5- Possible flap necrosis.
6- Interfer with wearing partial denture for covering the hard palate.
Combination of Buccal and Palatal Flaps
To close larger defects by local flaps often leads to failure.
When there is a history of earlier repair with failure.
It helps to have two layered closure to improves the strength of the flaps, also to minimizes contraction and risk of infection
Caldwell-Luc Operation
George Caldwell in 1893 described a method of gaining entry into the maxillary sinus via canine fossa with nasal antrostomy.Intranasal Antrostomy
It is performed to facilitate the drainage at the end of an operation performed (i) to close an oro-antral fistula,
(ii) to remove a tooth or a root from sinus.
Surgical procedure:
• A small sized osteotome is pushed through the inferior meatus in the nasal cavity, into the maxillary sinus.
• It performed by removing approximately 1 cm of the medial wall of the antrum, which bulges into the sinus below the level of the inferior turbinate.
• Then ribbon gauze is used to systematically pack the maxillary sinus cavity in multiple folds, to achieving proper haemostasis (after Caldwell-Luc operation).
Indications
1. Open procedure for removal of root fragments, teeth or foreign body or an antrolith (stone) from the maxillary sinus.2. To treat chronic maxillary sinusitis with hyperplastic lining and polypoid degeneration of the mucosa.
3. Removal of cysts or benign growths from the maxillary sinus.
4. Management of haematoma in the maxillary sinus and to control post-traumatic haemorrhage in the sinus.
5. Zygomaticomaxillary complex fractures involving floor of the orbit and anterior wall of the maxillary sinus.
6. Removal of impacted canine or impacted third molar.
7. Along with closure of chronic oroantral fistula, associated with chronic maxillary sinusitis