DENTAL IMPLANTS
Dr. Atalla FathiB D S, M Sc, F I B M F
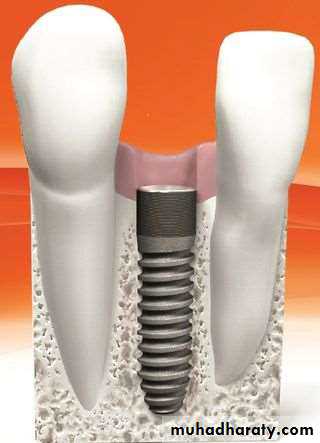
A dental implant is an artificial alloplastic material placed into the jaw bone to support a dental prosthesis
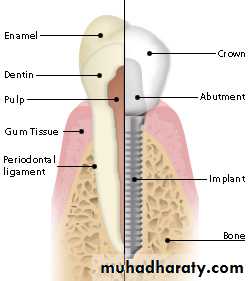
Anatomy of a Dental Implant
• A dental implant designed to replace a single tooth is composed of three parts:• The titanium implant that fuses with the jawbone ( fixture).
• The abutment, which fits over the portion of the implant that protrudes from the gum line
• Crown, which is fitted onto the abutment for a natural appearance.
Since the introduction of the Osseointegration concept and the Titanium Screw by Dr. Branemark, endosteal root-form implantsimplants have become the most popular implants in the world today
Endosteal root-form implants
osseointegration
A direct structural and functional connection between living alveolar bone and the surface of load carrying dental implantFibro-osseous integration -soft tissue(fibres)interposed between the implant surface & bone
Factors affecting osseointegration
• Implant biocompatibility• Implant design
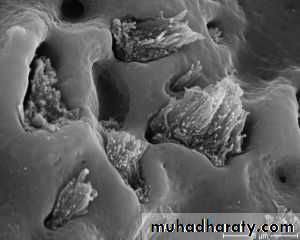
• Implant surface
• Implant bed
• Surgical technique
• Loading condition
Why osseointegration Fails
Poor surgical techniqueInexperienced operator
Poor surgical site
Infection
Heavy tobacco smoking
Uncontrolled diabetes
Primary stability
Primary stability is the initial mechanical lock between the screw implant and the bone. It depends on :
1- the length of the implant .
2- the diameter of the implant .
3- the thread design: number and thickness of the grooves.
4- the quality of the bone site : cortical versus spongy bone
5- the preparation of the surgical site, heat generation, torque, and speed of the hand piece burs.
Secondary stability
Is the stability when the osseointegration takes place . Usually after 3-6 months.Loading conditions
Delayed loading:3-6 months after implant insertion
Immediate loading:
1- Immediate occlusal loading (prosthesis is placed within 48 hours postsurgery)
2- Early loading (prosthetic function within two months)
Most commonly used biomaterials for implants:1- Commercially pure (CP) titanium2- Titanium-aluminum-vanadium alloy (Ti-6Al-4V)3- Cobalt-chromium-molydenum (Co-Cr-Mo) alloy is most used for subperiosteal implants.4- Calcium phosphate ceramics, Hydroxyapatite (HA), used for augmentation material or coating on surface.• Made of a titanium screw either having a rough or smooth surface
• Usually made of titanium from grade 1-4, but sometimes 5
• Titanium is used because it is strong and bio-inert
• The need for a strong metal is necessary to support the restoration after the procedure
• Titanium grades 1-4 are commercially pure, meaning made of just titanium unlike grade 5As the grade goes up, the stronger the titaniumGrade 5 contains aluminum and vanadium along with titanium, making it stronger than grades 1-4
Classification of dental implant prostheses
The four groups of implants prostheses are :1- over denture .
2- Single tooth replacement.
3- fixed prosthesis for the partially edentulous arch.
4- fixed prosthesis for the completely edentulous arch.
Dr,salah hegazy
Two-Implant Bar Overdenture
Single tooth prosthesisThe single tooth prosthesis is used to replace missing single tooth. Prosthesis support and retention come from the implant. Retention may be achieved through screws and cement.
Fixed prosthesis for the partially edentulous arch
The fixed -fixed bridge for the free end or bounded saddle area is a porcelain to metal restoration .it gains both its support and retention completely from the implants .The retention may be in the form of screw retention or cement.
Fixed prosthesis for the completely edentulous arch
It can be made in a style similar to conventional crown and bridge .It gains it support and retention from the implants.
Retention may be gained through the screws or cement.
Surgical operation
PATIENT EVALUATION
cooperation of the patient
the patient must be informed about the time necessary to complete the functional and aesthetic rehabilitation
the importance of maintaining good oral hygiene
The patient must also be informed of the possibility, during the post treatment period, of discomfort or pain caused by edema, haematoma, bleeding
Not to be ignored is also the patient psychological aspect and his/her expectations.
PRE – OPERATION EVALUATIONSThe general health state of the patient .
The clinical examination of the oral cavity must be made with particular attention for what concerns the quantity and quality of the present adherent mucosa, periodontal status and also the degree of the oral hygiene.
The clinical examination must also foresee the analysis of the bone base and that of the alveolar margins to verify their quality and adequacy for the implant treatment.
Evaluate the thickness of the bone
Determine the inter-occlusal distance both in the mouth and with study models mounted on an articulator.
Bone QualityAccording to Lekholm and Zarb.,1985
• Quality I• Bone is composed of homogenous compact bone, usually found in the anterior lower jaw.
• Quality II
• Bone is composed of a thick layer of cortical bone surrounding dense trabecular bone, usually found in the posterior lower jaw.
• Quality III
• Bone is composed of a thin layer of cortical bone surrounding dense trabecular bone, normally found in the anterior upper jaw but can also be seen in the posterior lower jaw and the posterior upper jaw.
• Quality IV
• Bone is composed of a very thin layer of cortical bone surrounding a core of low-density trabecular bone. It is very soft bone and normally found in the posterior upper jaw. It can also be seen in the anterior upper jaw.
PRE – SURGICAL PLANNING Radiographic examinations
The measurement of the bone vertical height must be performed through a radiographic examination. This will supply also indispensable information about the anatomy of the patient, facilitating the selection of the implant to be used and its correct positioning, taking into consideration the inviolable anatomic structures.
Intraoral radiographyPanoramic radiography
It allows to have a view of the dental arches and bone structures, maxillary sinus and nasal cavity, of the existing conservative and prosthetic restorations.Moreover, it allows to evaluate the general conditions of the periodontium and to put in evidence eventual pathologies or anatomical anomalies.
When evaluating a panoramic radiography, it is necessary to consider its distortion factor.
1:1.25 magnification ratio.
CBCT cone beam computed tomography
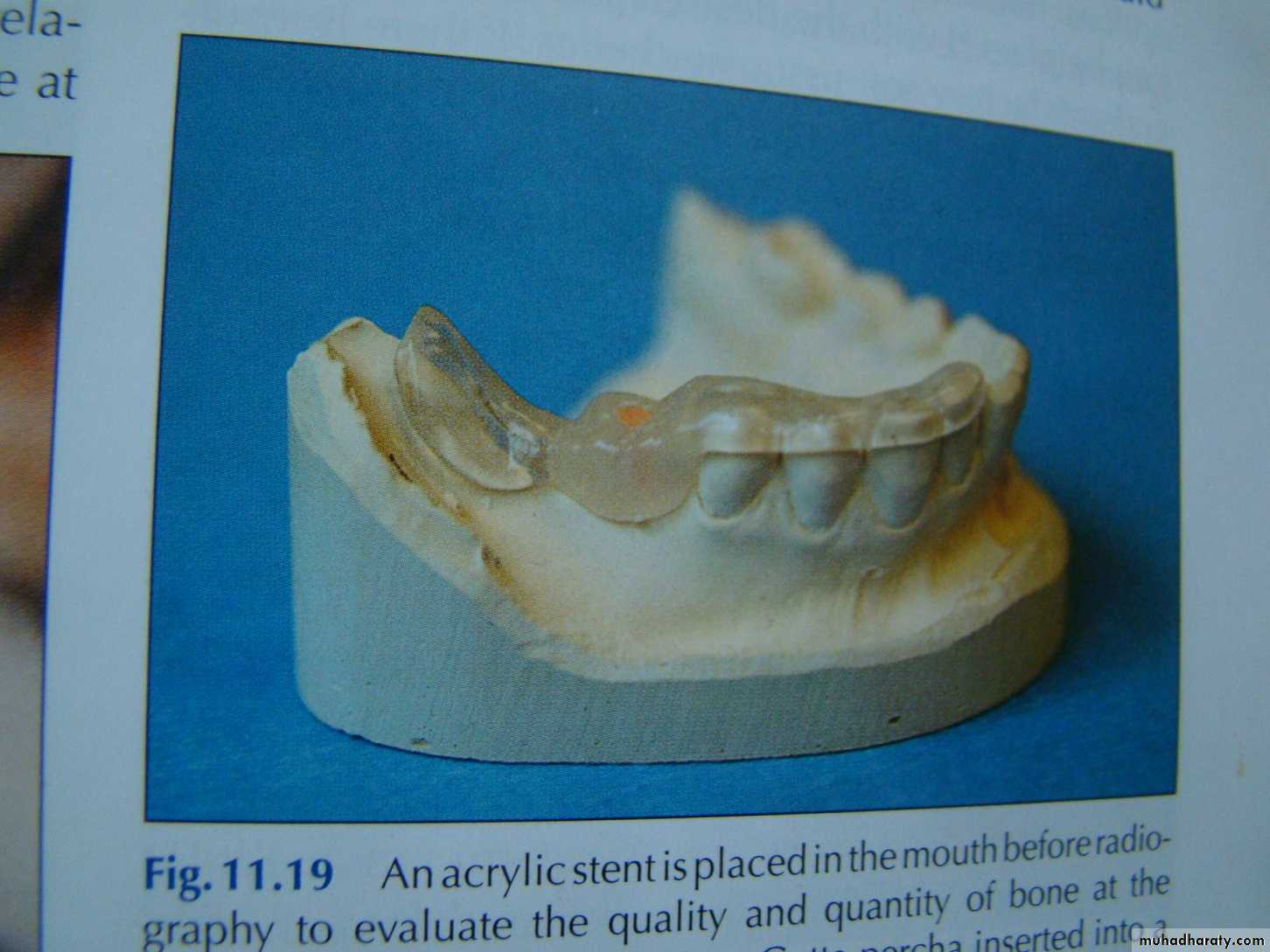
Cone Beam Computed Tomography (CBCT) uses 3D images from different planes like axial, coronal, and sagittal views. It provides a stream of data which helps a dental surgeon to reconstruct images when needed, while exposing patients to less amount of Radiation. This technology uses a conical beam of radiations. It reconstructs the image using special software. All information of a Computed Tomography are obtained with 1/8th of radiation exposure relative to conventional CT scan and at minimal cost.Surgical stent
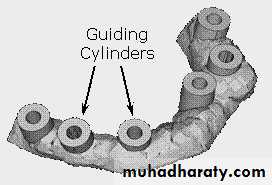
Once the position of the implants is determined by clinical, radiographical, and diagnostic cast examinations, a surgical stent is then fabricated.The surgical stent should seat on the occlusal surfaces of the remaining dentition, and the ridge should be clearly visible through the occlusal surfaces where the wax-up has been removed.
Surgical technique
• Minimal tissue violence at surgery is essential for proper osseointegration.• Careful cooling while surgical drilling is performed at low rotatory rates.
• Use of sharp drills.
• Use of graded series of drills.
• Use of intermittent drilling.
• The insertion torque should be of a moderate level because strong insertion torques may result in stress concentrations around the implant, with subsequent bone resorption.
• Holes are drilled through the temporary stent. This is done ensuring that the drill used is held vertical to the crest of the ridge and parallel from one hole to the other.