Bone graft substitutes
Formation of new bone can occur through three different processes:
osteogenesis, osteoinduction, and osteoconduction, which are regarded as the characteristics of an ideal bone graft materialOsteogenesis refers to new bone formation by predominantly existing differentiated osteoprogenitor cells or osteoblastic cells presenting within the graft material
Osteoinduction has been investigated as a possible mechanism of bone regeneration, which involves new bone formation from osteoprogenitor cells derived from mesenchymal cells under the influence of bone matrix proteins (BMP)
Osteoconduction is the most recognized process for bone repair, because the implant acts as a scaffold for bone ingrowth and is supposed to be replaced by new bone
This phenomenon is not bone formation, but provides a favourable environment for bone formation by ‘creeping substitution’
Osteoconduction refers to the ability to support the attachment of osteoblast and osteo-progenitor cells, and allow the migration and ingrowth of these cells within the three-dimensional architecture of the graft
Autologous (autogenous) bone implants May provide osteoconduction, osteoinduction and osteogenesis
Drawbacks
• Limited supply
• Donor site morbidity
To reduce or replace the harvesting of autogenous bone, various kinds of allografts, xenografts, and alloplasts ― natural or synthetic bone substitutes such as freeze-dried bone allograft (FDBA), demineralized FDBA (DFDBA), bovine derived porous bone material, and synthetic calcium phosphate ― have been developed
Characteristics of an ideal bone graft substitutes
• Has osteogenesis, osteointegration, osteoinductive, and osteoconductive properties• biocompatible
• show minimal fibrotic reaction
• undergo remodelling and support new bone formation
• have a similar strength to that of the cortical/cancellous bone being replaced
Bone Graft SubstitutesPotential Roles
• Extender for autogenous bone graft• Enhancer
To improve success of autogenous bone graft
• Substitute
To replace autogenous bone graft
Bone graft substitutes
• Most of them have osteoconductive properties• Some have osteoinductive agents mainly rhBMP-2 and rhBMP-7
Bone Graft Substitutes
• Calcium sulfate• Collagen based matrices
• Demineralized bone matrix
• Calcium phosphate
• Tricalcium phosphate
• Hydroxyapatite
• Osteoinductive proteins
Calcium Sulfate (CaSo4)
Calcium sulfate is actually plaster of Paris. Calcium sulfate is thought to act as an osteoconductive matrix for the ingrowth of blood vessels and associated fibrogenic and osteogenic cells• Rapidly resorbs (5–7 weeks )
• Calcium sulfate in its set form has a compressive strength greater than cancellous bone and a tensile strength slightly less than cancellous bone
• Calcium sulfate, however, requires a dry environment to set
• Calcium sulfate is used as an osteoconductive void filler
• A medical grade of calcium sulfate impregnated with tobramycin is commercially available
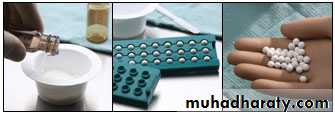
Calcium Sulfate forms
• Pellets
Pellet injectors
• Bead kits
Allows addition of antibiotics
• Injectable
Collagen Based Matrices
Highly purified Type 1 bovine dermal fibrillar collagenBone marrow is added to provide bone forming cells
• Collagraft (Zimmer)
Collagen / HA / Tricalcium phosphate
• Healos (Depuy)
Collagen / HA
Demineralized Bone Matrix
• Is a kind of highly processed allograft derivative with at least 40% of the mineral content of the bone matrix removed by mild acid, while collagens, non-collagenous proteins and growth factors remain
• Prepared from cadaveric human bone
• BMP quantity extremely low and variable
• Sterilized which may decrease the availability of BMP
Available in multiple preparations
• Gel• Putty
• Strip
• Combination products with cancellous bone and other bone graft substitute products
While they may offer some osteoinductive potential because of available growth factors, they mainly act as an osteoconductive agents
Calcium phosphates
e.g. beta-tricalcium phosphate and hydroxy apatiteThe calcium phosphate family of synthetic bone grafts has both osteointegrative and osteoconductive properties
Osteointegration results from the formation of a layer of HA shortly after implantation
They have an excellent record of bio-compatibility with no reports of systemic toxicity or foreign body reactions
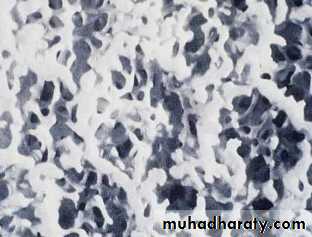
Beta Tricalcium Phosphate (β-TCP)
• Beta tricalcium phosphate undergoes reabsorption over a 6–18-month period
• Has a compressive strength and tensile strength similar to cancellous bone
• Available in porous or solid form as either granules or blocks
Unfortunately the replacement of βTCP by bone does not occur in an equitable way. That is, there is always less bone volume produced than the volume of βTCP reabsorbed. For this reason the clinical use of βTCP has been as an adjunctive with other less reabsorbable bone graft substitutes or as an expander for autogenous bone graft
Hydroxyapatite
Synthetic hydroxyapatiteCoralline hydroxyapatite
Synthetic hydroxyapatite
Hydroxyapatite C10(PO4)6(OH)2 forms the principal mineral component of boneSynthetic HA comes in ceramic or non-ceramic form as porous or solid, blocks or granules
Synthetic HA have good compressive strengths but are weak in tension and shear
They are brittle and are fracture prone on shock loading
Synthetic HA in solid block form is difficult to shape, does not permit fibro-osseous ingrowth
Synthetic HA has been successfully used to coat metal implants to enhance their osteointegration.
In porous granular form it has been used alone or with bone graft to fill voids
Coralline hydroxyapatite
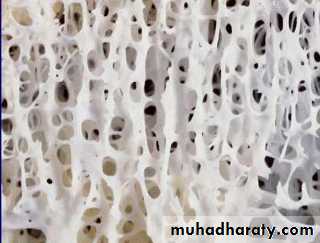
Coralline HA was developed with the aim to create a HA implant with a consistent pore size and improved interconnectivity
With synthetic HA it has been difficult to control pore size and pore interconnectivity
Interconnectivity is essential because constrictions between pores or dead-end pockets limit vascular support to ingrowing tissue
Coralline HA utilizes the genetically determined highly regular and permeable structure of marine coral which closely resembles that of cancellous bone
cancellous bone
HydroxyapatiteCoralline HA is Bioresobable (slow resorption) and biocopatible
Coralline HA is only slightly greater in compressive strength than cancellous bone, it is weak in tension, brittle and difficult to shape Coralline HA initially does not possess the strength of trabecular bone nor the plastic properties because it lacks a collagen matrix but with completion of fibro-osseous ingrowth the coralline HA becomes stronger than cancellous boneCoralline HA has been successfully used in non-weight bearing applications such as maxillofacial, periodontal augmentation its use in weight bearing defects has also been successful, but due to its initial mechanical weakness it must be supported by internal fixation until completion of fibroosseous ingrowth
Biphasic calcium phosphate (BCP)
Is another widely used commercial ceramic obtained by mixing hydroxyapatite and tricalcium phosphate in different concentrations for the purpose of combining the advantages of both calcium salts. By adjusting the formulation, the dissolution rate and mechanical properties can be controlled within ranges
Bone Morphogenetic Proteins
• Bone morphogenetic proteins are a group of nine known proteins which represent factors of growth and differentiation with the ability of inducing new bone (osteoinduction)
• They are a subgroup of transforming growth factor
• studies have demonstrated that in order for proteins to release their clinical function they need carriers. So far absorbable collagen sponge has been most frequently used as a carrier
• Non-immunogenic and non-species specific
• Produced by recombinant technology
• Two most extensively studied and commercially available are:
BMP-2 and BMP-7
Other growth factors
Growth factors are proteins which regulate the complex processes of wound healing.Growth factors play a main role on cell migration, cell proliferation and angiogenesis in tissue regeneration phase
These growth factors are mainly located in blood plasma and platelets TGF, PDGF,AGF(autologous growth factor) FGF
Concentrated GF is well known to accelerate new bone formation
The venous blood sample is taken without anticoagulants in sterile 10mL tube and immediately centrifuged in special centrifuge device for 12 minutes