
1
Physiology
Lec.(4)
--------------------------------------------------------------------------------
Arterial blood pressure
The blood pressure provides the driving force for circulation of blood, it has
been defined as the lateral pressure exerted by the blood on the wall of blood
vessels
Systolic pressure:-
It is the maximum pressure during systolic phase of the cardiac cycle and in
healthy adults it ranges from110-140mmHg.the average being 120mmHg
Diastolic pressure:-
It is the maximum pressure during ventricular diastole and its normal range is
60-90mmHg.with an average value of 80mmHg in adults
The difference between systolic and diastolic pressure is called pulse pressure
and it is about 40mmHg
Mean blood pressure=Diastolic pressure+1/3pulse pressure
Physiological variations
Blood pressure shows certain physiological variations
1-Age-blood pressure is relatively low in children and it increases with age. in
old age blood pressure rises, the systolic rise being greater than diastolic and
this is due to arteriosclerosis
2-sex-in female blood pressure is lower than males but after men a pause
this difference is abolished
3-Diurnal variation-during sleep and rest blood pressure is reduced
4-Digestion there is arise of blood pressure during digestion
5-Posture –change of posture from recumbent to erect position causes arise
of diastolic pressure due to baroreceptor mechanism
6-Exercise –muscular exercise results in arise of systolic blood pressure due
to increased venous return but there is no alteration in the diastolic blood
pressure
7-Emotion –emotional excitement activates the sympathetic nervous system
and consequently produces arise of systolic blood pressure
Factors influencing blood pressure
Blood pressure is the resultant of cardiac output and peripheral resistance
BP=CO × PR
Nervous control of circulation is exerted almost through autonomic nervous
system, sympathetic nerves innervate blood vessels and heart, sympathetic
stimulation of small arteries and arterioles increases vascular resistance and
decreases the rate of blood flow through the tissues ,innervation of the large
vessels especially the veins makes it possible for sympathetic stimulation to
decrease the volume of the vessels.
Sympathetic fibers also go to the heart and stimulate the activity of the heart
,increasing both the rate and strength of pumping , Parasympathetic
stimulation decrease heart rate and heart muscle contractility, its main role in
controlling the circulation

2
Is to markedly decrease heart rate and slightly decrease heart muscle
contractility
One of the most important functions of sympathetic nervous system is to
provide rapid control of arterial pressure by causing vasoconstriction and
stimulation of the heart. at the same time that sympathetic activity is
increased ,there is a reciprocal Inhibition of parasympathetic vagal signals to
the heart that also contribute to a greater heart rate
There are three major changes that take place to increase arterial pressure
through stimulation of autonomic nervous system
1-arterioles are constricted, causing increased total peripheral resistance and
raising blood pressure
2-the veins and large vessels of the circulation are constricted, displacing
blood from peripheral vessels toward the heart and causing the heart to
pump with greater force, which also help to raise arterial pressure
3-enhancing heart pumping an important characteristic of nervous control is
that it is very rapid, beginning within seconds ,conversely ,sudden inhibition
of nervous stimulation can decrease the arterial pressure within seconds
Reflex Mechanisms for Maintaining
Normal Arterial Pressure
Aside from the exercise and stress functions of the autonomic nervous system
to increase arterial pressure there are other control mechanisms such as.
The Baroreceptor Arterial Pressure Control
System—Baroreceptor Reflexes
, this reflex is initiated by stretch receptors, called either
baroreceptors or
press receptors, located at specific points in the walls of several large
systemic arteries. A rise in arterial pressure stretches the baroreceptors and
causes them to transmit signals into the central nervous system. “Feedback”
signals are then sent back through the autonomic nervous system to the
circulation to reduce arterial pressure downward toward the normal level.
Physiologic Anatomy of the Baroreceptors and Their Innervation.
Baroreceptors are spray-type nerve endings that lie in the walls of the
arteries; they are stimulated when stretched. A few baroreceptors are located
in the wall of almost every large artery of the thoracic and neck regions; but,
as shown in Figure baroreceptors are extremely abundant in (1) the wall of
each internal carotid artery slightly above the carotid bifurcation,
an area known as the
carotid sinus, and (2) the wall of the aortic arch.
Figure shows that signals from the “carotid baroreceptors” are transmitted
through very small
Hering’s nerves to the
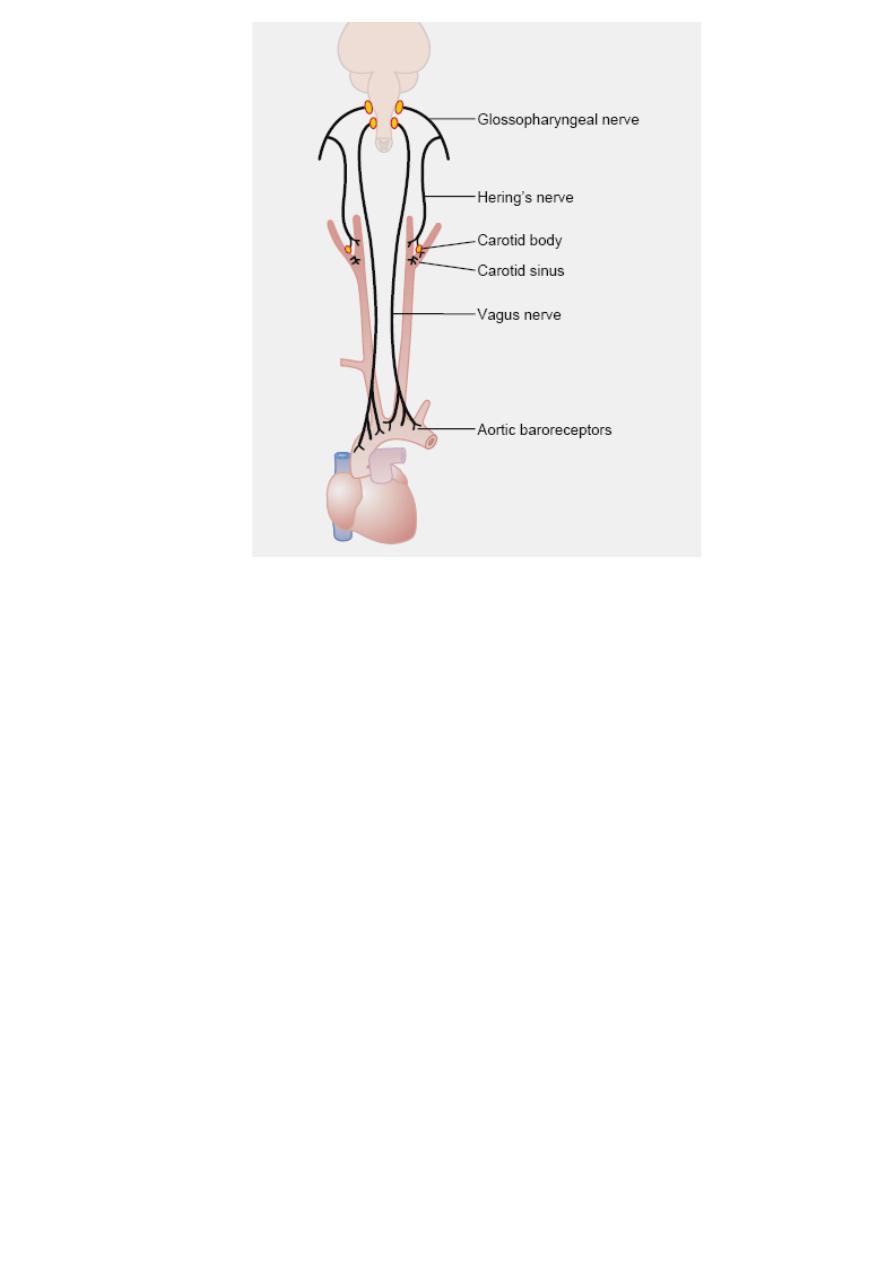
3
glossopharyngeal nerves in the high neck, and then to the tractus solitarius in
the medullary area of the brain stem. Signals from the
aortic baroreceptors” in the arch of the aorta are transmitted through the
vagus nerves also to the same tractus solitarius
.
Circulatory Reflex Initiated by the Baroreceptors. After the
baroreceptor signals have entered the tractus solitarius
of the medulla, secondary signals
inhibit the vasoconstrictor center of the
medulla and
excite the vagal parasympathetic center. The net effects are (1)
vasodilation of the veins and arterioles throughout the peripheral circulatory
system and (2)
decreased heart rate and strength of heart contraction.
Therefore, excitation
of the baroreceptors by high pressure in the arteries
reflexly
causes the arterial pressure to decrease because of both a decrease
in peripheral resistance
and a decrease in cardiac output. Conversely, low
pressure
has opposite effects, reflexly causing the pressure to rise back
toward normal.
Function of the Baroreceptors During Changes in Body
Posture. The ability of the baroreceptors to maintain relatively constant
arterial pressure in the upper body is important when a person stands up
after having been lying down. Immediately on standing, the arterial pressure
in the head and upper part of the body tends to fall, and marked reduction of
this pressure could cause loss of consciousness. However, the falling pressure
at the baroreceptors elicits an immediate reflex, resulting in strong
sympathetic discharge throughout the body. This minimizes the decrease in
pressure in the head and upper body.

4
. Because the baroreceptor system opposes either increases or decreases in
arterial pressure, it is called a
pressure buffer system, and primary purpose
of the arterial baroreceptor system is to reduce the minute by minute
variation in arterial pressure to about one third that which would occur were
the baroreceptor system not present..
Control of Arterial Pressure by the Carotid and Aortic chemo
receptors
The
chemoreceptors are chemosensitive cells sensitive to oxygen lack,
carbon dioxide excess, and hydrogen ion excess. They are (two
carotid
bodies, one of which lies in the bifurcation of each common carotid artery,
and usually one to three
aortic bodies adjacent to the aorta).when blood
pressure falls below acritical level,the chemoreceptors become stimulated
because diminished blood flow causes decreased oxygen as well as excess
buildup of carbon dioxide and hydrogen ions the signals transmitted from
chemoreceptors excite the vasomotor center and this elevates the arterial
pressure back toward normal
The central nervous system ischemic response
When blood flow to the vasomotor center in the lower brain stem becomes
sufficiently decreased to cause cerebral ischemia(I.e.,nutritional deficiency)
the neurons of the vasomotor center become strongly excited.when this
occurs,systemic arterial pressure often rises as high as the heart can
pump.this response is an emergency arterial pressure control system that acts
rapidly and powerfully to prevent further decline
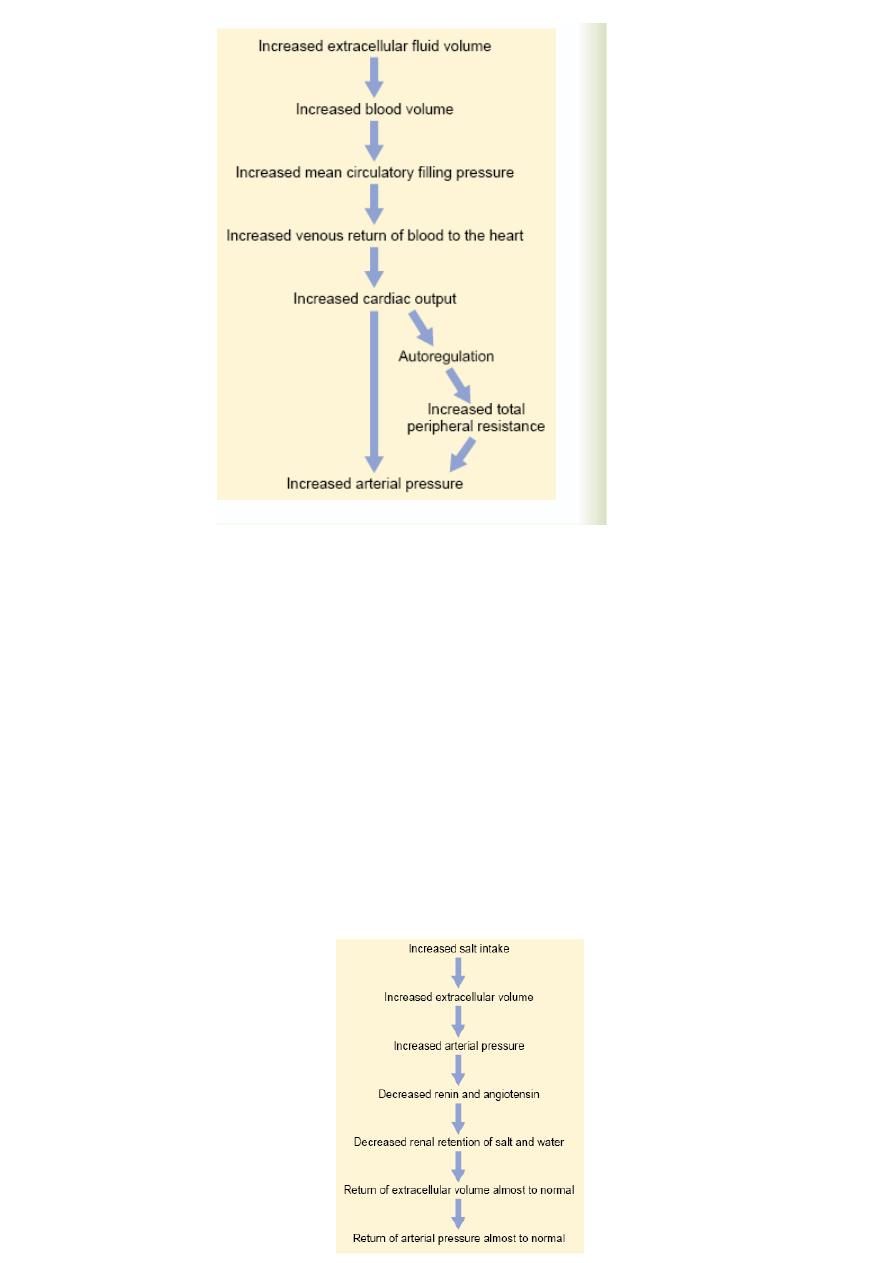
Renal–Body Fluid (long term control of arterial pressure)
the Figure . The sequential events are (1) increased extra cellular fluid
volume (2) increases the blood volume, which (3) increases the mean
circulatory filling pressure, which (4) increases venous return of blood to the
heart, which (5) increases cardiac output, which (6) increases arterial
pressure.
Note especially in this schema the two ways in which an increase in cardiac
output can increase the arterial pressure. One of these is the direct effect of
increased cardiac output to increase the pressure, and the other is an indirect
effect to raise total peripheral vascular resistance through
autoregulation of
blood flow.
5
Importance of Salt (NaCl) in the Renal–Body
Fluid Schema for Arterial Pressure Regulation
1. When there is excess salt in the extra cellular fluid, the osmolality of the
fluid increases, and this in turn stimulates the thirst center in the brain,
making the person drink extra amounts of water to return the extra cellular
salt concentration to normal. This increases the extra cellular fluid volume.
2. The increase in osmolality caused by the excess salt in the extra cellular
fluid also stimulates the –posterior
pituitary gland secretory mechanism to
secrete increased quantities of
antidiuretic hormone. The antidiuretic
hormone then causes the
kidneys to reabsorb greatly increased quantities of
water from the renal tubular fluid, thereby diminishing the excreted volume of
urine but increasing the extracellular fluid volume. Thus, for these important
reasons, the amount of salt that accumulates in the body is the main
determinant of the extracellular fluid volume. Because only small increases in
extracellular fluid and blood volume can often increase the arterial pressure
greatly, accumulation of even a small amount of extra salt in the body can
lead to considerable elevation of arterial pressure.
6
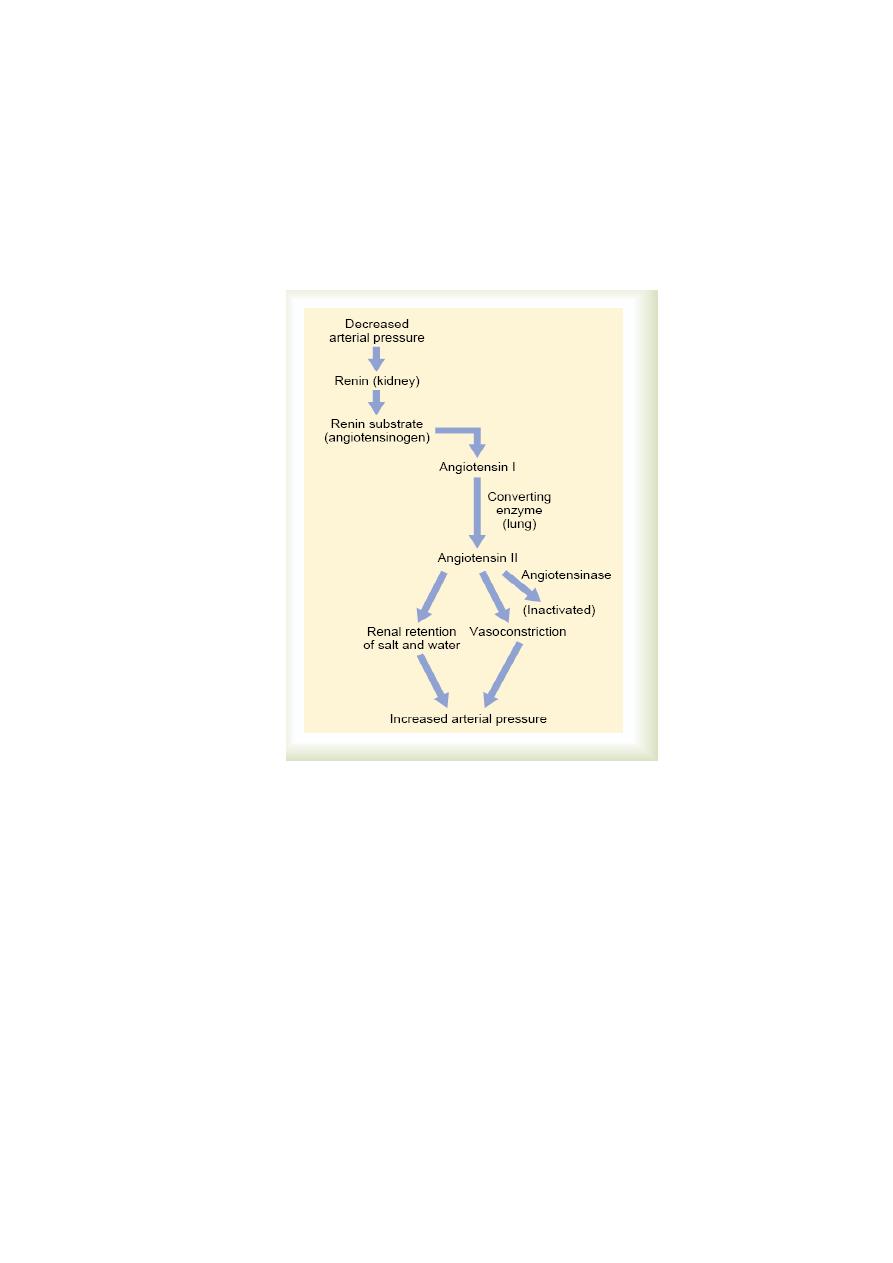
The Renin-Angiotensin System: Its Role in Pressure Control and in
Hypertension Aside from the capability of the kidneys to control arterial
pressure through changes in extra cellular fluid volume, the kidneys also have
another powerful mechanism for controlling pressure. It is the renin
angiotensin system.
Renin is a protein enzyme released by the kidneys when the arterial pressure
falls too low. In turn, it raises the arterial pressure in several ways, thus
helping to correct the initial fall in pressure
Hypertension in Preeclampsia (Toxemia of Pregnancy).
Approximately 5 to 10 per cent of expectant mothers develop a syndrome
called
preeclampsia (also called toxemia of pregnancy). One of the
manifestations of preeclampsia is hypertension that usually subsides after
delivery of the baby. Although the precise causes of preeclampsia are not
completely understood, ischemia of the placenta and subsequent release by
the placenta of toxic factors are believed to play a role in causing many of the
manifestations of this disorder, including hypertension in the mother.
Substances released by the ischemic placenta, in turn, cause dysfunction of
vascular endothelial cells throughout the body, including the blood vessels of
the kidneys. This
endothelial dysfunction decreases release of nitric oxide and
other vasodilator substances, causing vasoconstriction, decreased rate of fluid
filtration from the glomeruli into the renal tubules, impaired renal pressure
natriuresis, and development of hypertension. Another pathological
abnormality that may contribute to hypertension in preeclampsia is thickening
of the kidney glomerular membranes (perhaps caused by an autoimmune
process), which also reduces the rate of glomerular fluid filtration. For obvious

7
reasons, the arterial pressure level required to cause normal fo rmation of
urine becomes elevated, and the long-term level of arterial pressure becomes
correspondingly elevated. These patients are especially prone to extra
degrees of hypertension when they have excess salt intake.
Neurogenic Hypertension.
Acute neurogenic hypertension
can be caused by strong
stimulation of the sympathetic nervous system. For
instance, when a person becomes
excited for any reason or at times during
states of
anxiety, the sympathetic system becomes excessively stimulated,
peripheral vasoconstriction occurs everywhere
in the body, and acute
hypertension ensues.
―Primary (Essential) Hypertension‖
About 90 to 95 per cent of all people who have hypertension are said to have
“primary hypertension,” also widely known as “essential hypertension” by
many clinicians. These terms mean simply that
the hypertension is of
unknown origin, in contrast to those forms of
hypertension that are
secondary to known causes, such as renal artery
stenosis. In some patients with primary hypertension, there is a strong
hereditary tendency
In most patients,
excess weight gain and sedentary lifestyle appear to play a
major role in causing hypertension.
The majority of patients with
hypertension
are overweight, and studies of different populations suggest
that excess weight gain and obesity may
account for as much as 65 to 70
percent of the risk
for developing primary hypertension. Clinical studies have
clearly shown the value of weight loss for reducing
blood pressure in most
patients with hypertension.
In fact, new clinical guidelines for treating
hypertension
recommend increased physical activity and weight loss as a first
step in treating most patients with
hypertension. Some of the characteristics
of primary hypertension
caused by excess weight gain and obesity include:
1.
Cardiac output is increased due, in part, to the additional blood flow
required for the extra adipose tissue. However, blood flow in the heart,
kidneys, gastrointestinal tract, and skeletal muscle also increases with weight
gain due to increased metabolic rate and growth of the organs and tissues in
response to their increased metabolic demand
2.
Sympathetic nerve activity, especially in the kidneys, is increased
in overweight patients. The causes of increased sympathetic activity in
obesity are not fully understood, but recent studies suggest that hormones,
such as
leptin, released from fat cells may directly stimulate multiple regions
of the hypothalamus, which, in turn, have an excitatory influence on the
vasomotor centers of the brain medulla.
3.
Angiotensin II and aldosterone levels are increased two- to
threefold in many obese patients. This may be caused partly by increased
sympathetic nerve
stimulation, which increases renin release by the kidneys
and therefore formation of angiotensin II,
which, in turn, stimulates the
adrenal gland to
secrete aldosterone.
4.
The renal-pressure natriuresis mechanism is impaired, and the
kidneys will not excrete adequate amounts of salt and water unless

8
the arterial pressure is high or unless kidney function is somehow
improved.
