Gynecological questions
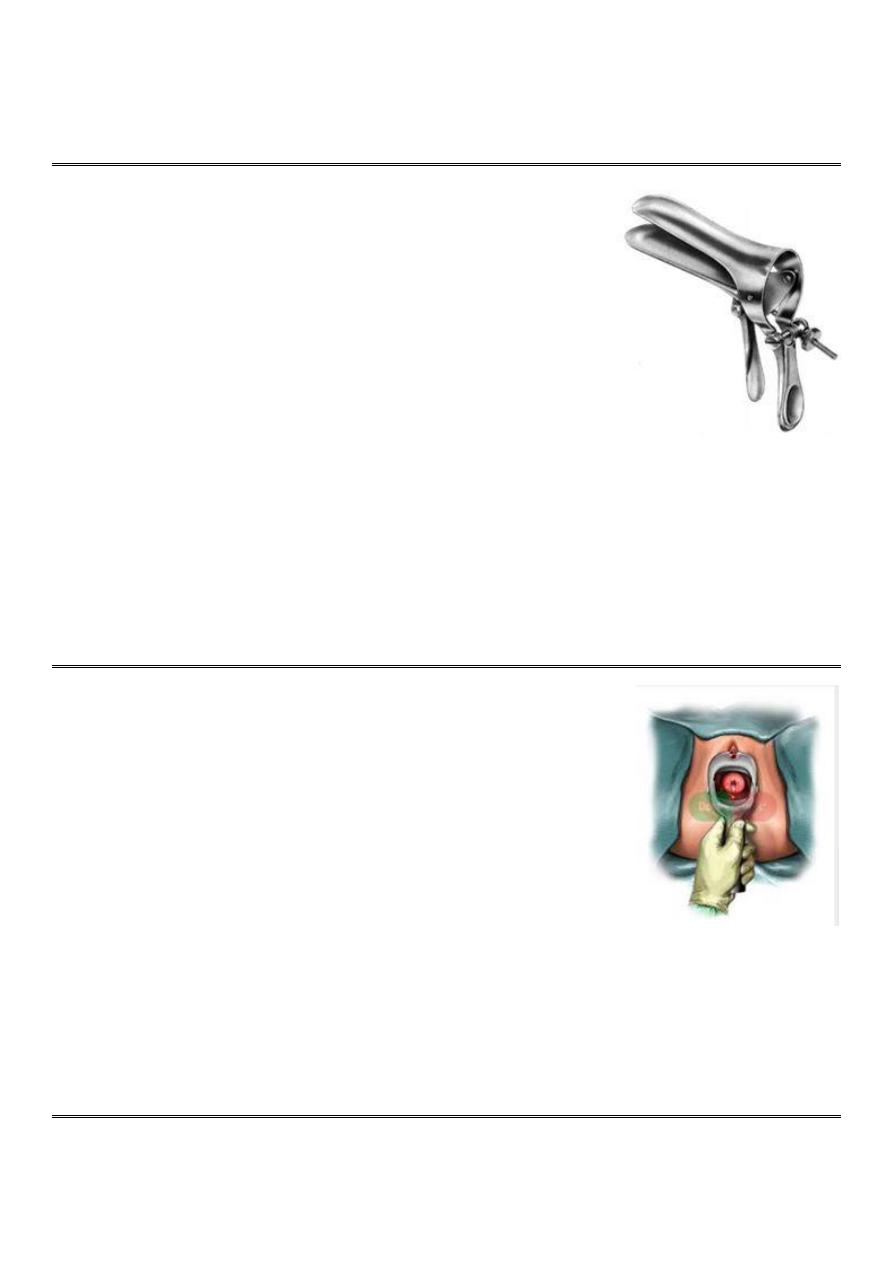
Q1: Name this instrument
Q2: Mention its uses
Q3: What are the advantages of this instrument?
===========
Answer 1 ==> Bi-
valve or Cusco’s speculum
Answer 2 ==>
1-For examination of cervix, fornices, lateral vaginal wall.
2-When the biopsy is to be taken from the cervix.
3-For cauterization of cervical erosions.
4-For insertion of IUCD.
5-For some investigations like (cotton for high vaginal swap, pap smear).
Answer 3 ==>
1-It is self-retaining speculum.
2-It is easy to use.
3-The vaginal walls can be retracted to a variable extent.
4-It gives a good exposure of the cervix.
5-Both anterior and posterior vaginal walls can be retracted with a single instrument.
6-It causes least discomfort to the patient.
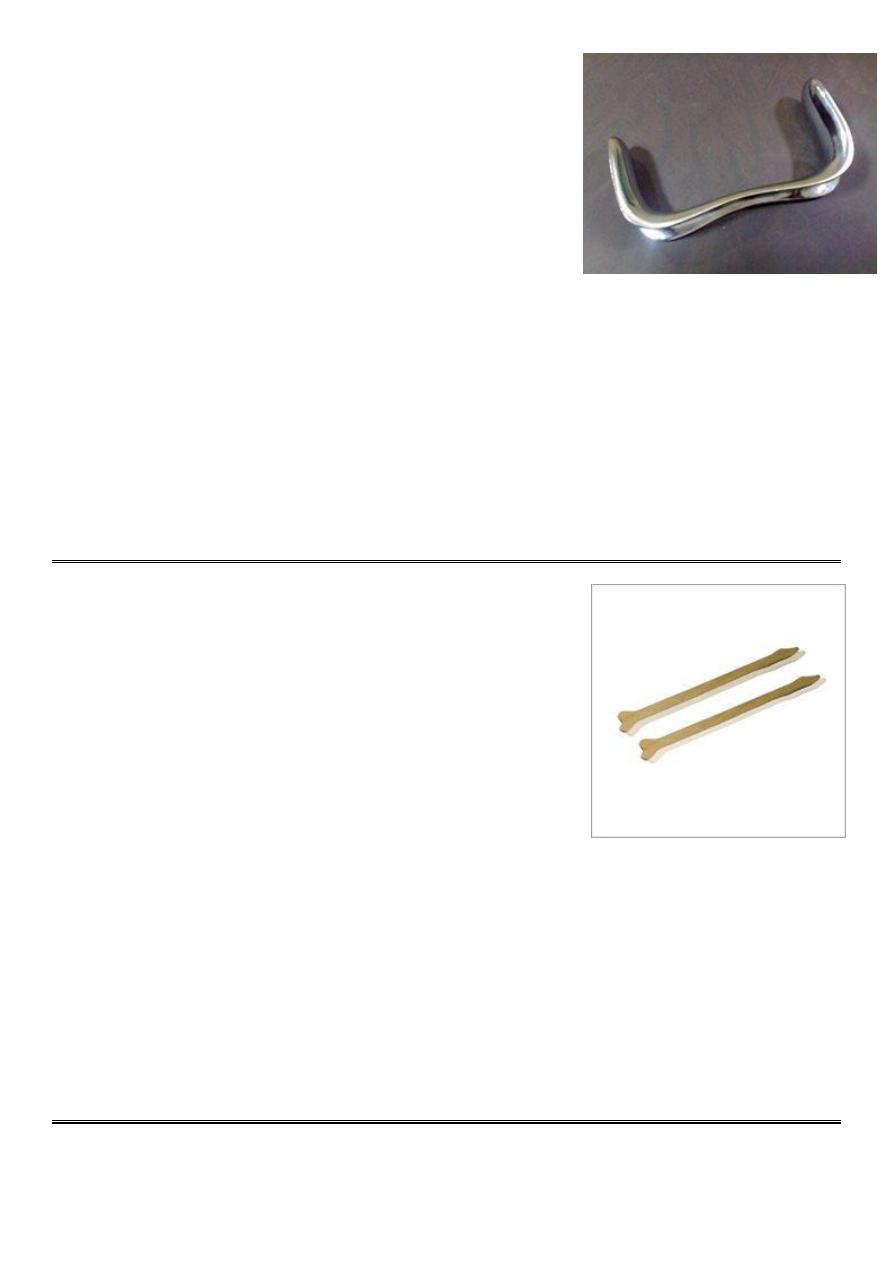
Q1: Name this procedure
Q2: How you prepare for this procedure?
Q3: How you do this procedure?
===========
Answer 1 ==> Specular examination
Answer 2 ==>
1-Take permission form the patient to do this examination
2-Do the examination in isolated place
3-Need good lightening
4-Use sterile instrument
5-Good covering of the patient
6-Use the instrument gently to avoid any trauma or pain
Answer 3 ==>
At the beginning close the speculum and put it at 9 o'clock degree, then start to enter it through the vestibule until
reach the cervix, then rotate it to 6 o'clock or 12 o'clock, then open it and fixed it by screw, complete the examination
and investigations, then start to remove the speculum, close the upper and lower plate by using the screw, rotate to 9
o'clock then remove it from the vagina.
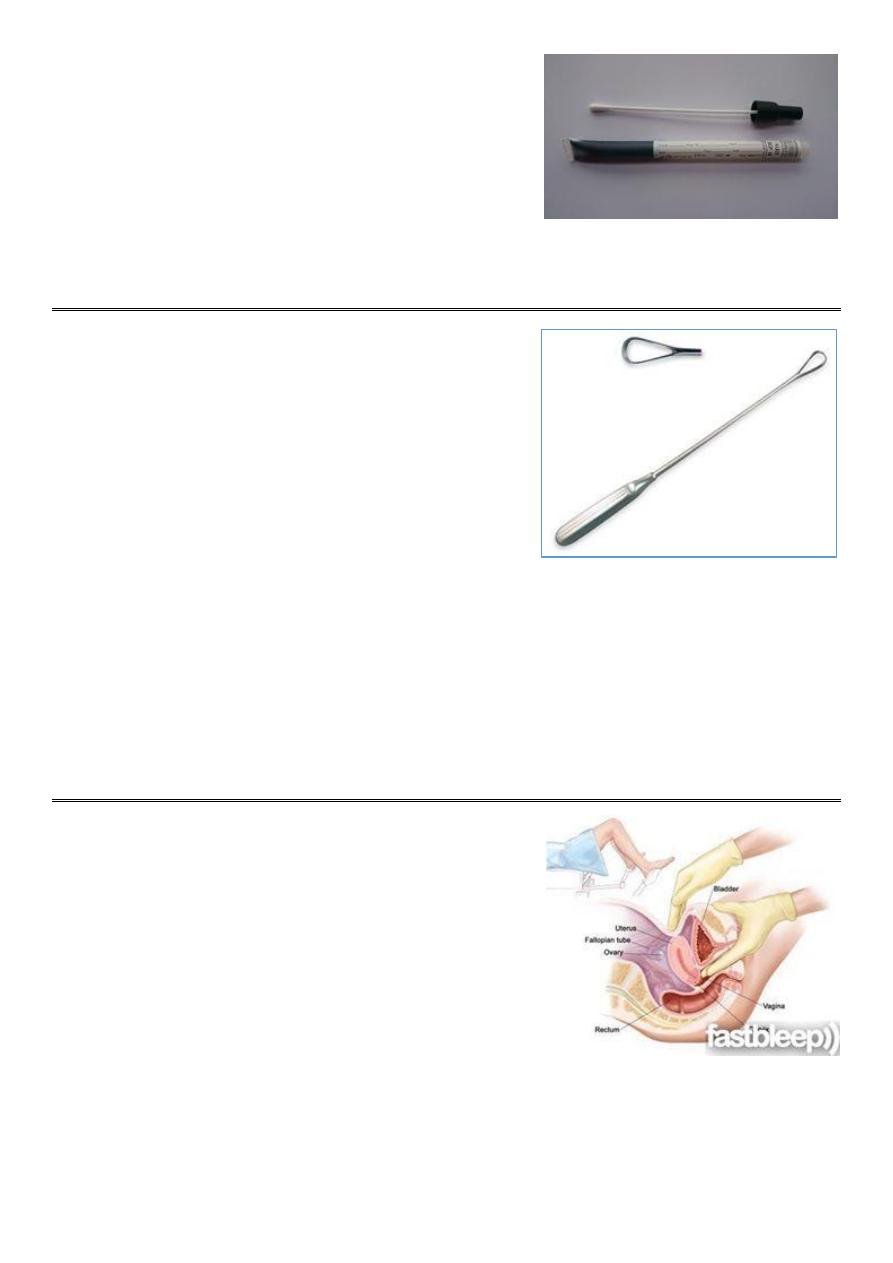
This instrument is Sim’s speculum
Q1: What are the uses of it?
Q2: What are the differences between cusco and sims speculum?
==============
Answer 1 ==>
1-See the Bulging of bladder (cystocele): due to weakness of anterior vaginal
wall, you can examine it by asking the patient to come with full bladder or ask
the patient to cough so the bulging become more obvious, and see some
fluid.
2-Bulging of the rectum (rectocele)
3-Cystorectocele.
4-Used for retracting the posterior vaginal wall during dilatation & curettage (D & C) and during dilatation & evacuation
(D & E).
5-For taking biopsy from genital tract.
6-For routine per speculum examination.
7-Outdoor cauterization of erosion.
Answer 2 ==>
1-Cusco is self retaining speculum, but sims is not self retaining
2-Cusco east to use and not need assistance, but sims need assistance by another person or nurse
3-Cusco provide a good view of the cervix, but sims not provide this view
4-We need only one cusco speculum to view lateral vaginal walls, but we need sims with anterior vaginal retractor to
do the same thing
5-Cusco lead to less discomfort to the patient than the sims speculum
Q1: Name this instrument
Q2: In which test you use it?
Q3: Mention the other instrument used in this test
Q4: How you do this test?
===============
Answer 1 ==> spatula
Answer 2 ==> pap smear
Answer 3 ==>
1- Spatula or cytobrush
2- Slide
3- Cusco speculum
4- gloves
Answer 4 ==>
1- First put the Cusco's speculum, then enter the spatula to the vagina
2- At the top of the spatula there is lingual part (put it in the inner part of the cervix) and shoulder part (put it in the
ectocervix).
3- Rotate the spatula and take columnar cells (by lingual part) and squamous cells (by shoulder part).
4- Put the spatula on the slide and do fixation.
5- Send the slide to the lab for cytology.
Q1: Name this instrument
Q2: How you use it?
============
Answer 1 ==> Cotton for high vaginal swap
Answer 2 ==>
Enter the cusco speculum through the vagina, then put the cotton on
the posterior fornix (site of discharge accumulation) then remove the cotton without touching the vaginal wall, then put
it in container and write the name of the patient and the time of examination and send it to the lab swap for culture and
sensitivity.
Q1: Name this instrument
Q2: Enumerate its type
Q3: What are its uses?
Q4: What are the complications of it?
=============
Answer 1 ==> Uterine curette
Answer 2 ==>
Sim's curette, Sharp & blunt curette, Goldstein curette
Answer 3 ==>
1-To curette out the products of conception in cases of missed or incomplete conception.
2-To curette out endometrium in cases of endometrial diseases for diagnostic and therapeutic purposes (in case of
infertility, postmenopausal bleeding, endometrial cancer).
3-For checking curettage: done 1 week after evacuation of H.mole.
Answer 4 ==>
Hemorrhage, sepsis, perforation of the uterus, vigorous curettage lead to amenorrhea due to total removal of
endometrium (Asherman's syndrome).
Q1: Name this examination
Q2: How you can perform it?
===============
Answer 1 ==> Bimanual examination
Answer 2 ==>
•This is usually performed after the speculum examination and is
performed to assess the pelvic organs.
•It is customary to use the left hand to part the labia and expose the
vestibule and then insert one or two fingers of the right hand into the
vagina. The fingers are passed upwards and backwards to reach the cervix
•The cervix is palpated => any irregularity, hardness or tenderness noted.
•The left hand is now placed on the abdomen below the umbilicus and pressed down into the pelvis to palpate the
fundus of the uterus.
•The fundus => size, shape, position, mobility, consistency and tenderness are noted.
•The normal uterus is pear shaped and about 9 cm in length. It is usually anterior (antiverted) or posterior (retroverted)
and freely mobile and non-tender.
•The tips of the fingers are then placed into each lateral fornix to palpate the adenexae (tubes and ovaries) on each
side.
•The fingers are pushed backwards and upwards, while at the same time pushing down in the corresponding area with
the fingers of the abdominal hand.
•It is unusual to be able to feel normal ovaries, except in very thin women.
•Ovaries => Any swelling or tenderness is noted, although remember that normal ovaries can be very tender when
directly palpated.
•The posterior fornix should also be palpated to identify the uterosacral ligaments which may be tender or scarred in
women with endometriosis.
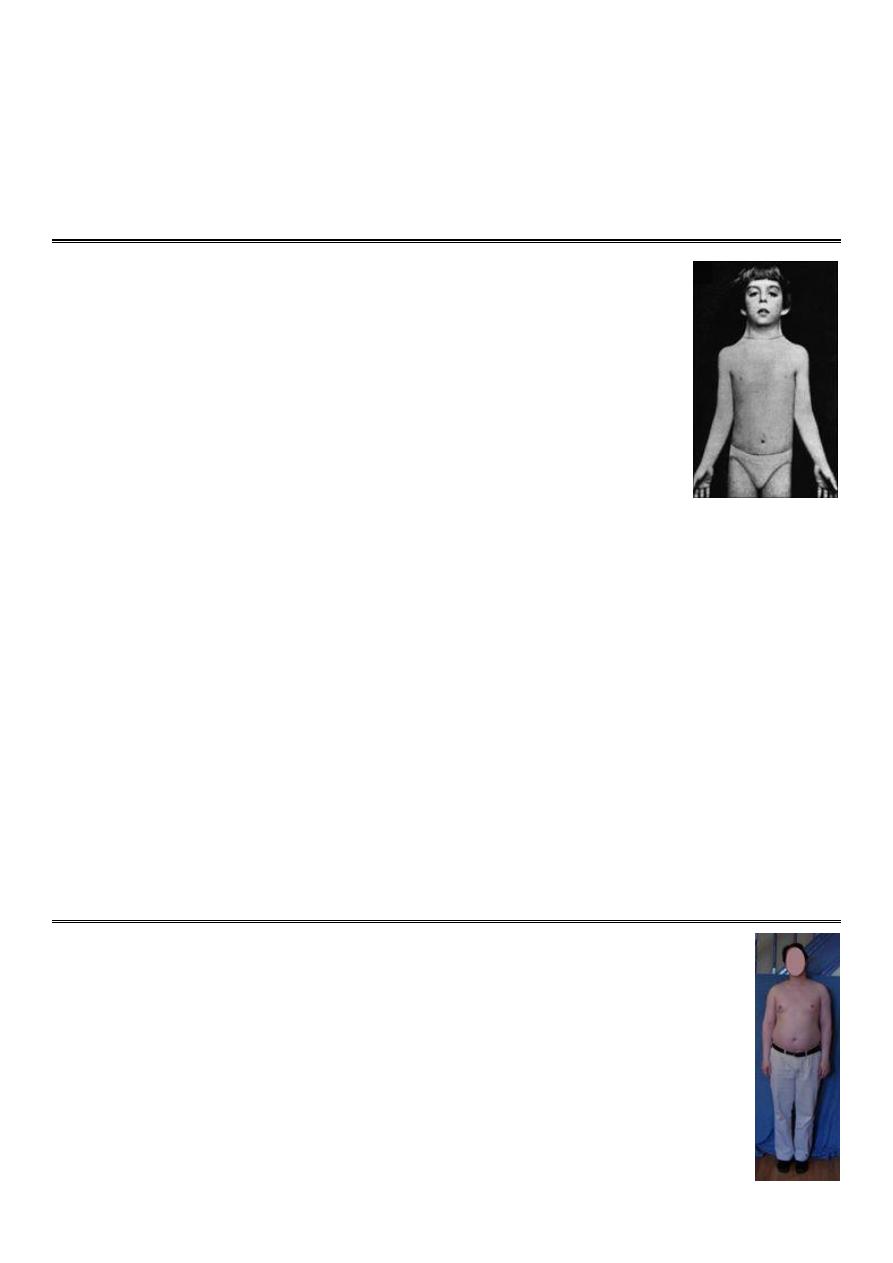
Q1: What is your diagnosis?
Q2: Write about symptoms and tests
Q3: How to treat this condition?
===========
Answer 1 ==> Bartholin's cyst
Answer 2 ==>
Symptoms of a cyst that is not infected include:
1-A painless lump in the vulva area.
2-Redness or swelling in the vulva area.
3-Discomfort when walk, sit, or have sex.
Symptoms of an infected cyst include:
1-Pain that gets worse
2-Fever and chills.
3-Swelling in the vulva area.
4-Drainage from the cyst.
Tests:
1-Ask questions about your medical history
2-Perform a pelvic exam
3-Take a sample of secretions from your vagina or cervix to test for a sexually transmitted infection
4-Recommend a test of the mass (biopsy) to check for cancerous cells if postmenopausal or over 40
Answer 3 ==>
1-pain medicine such as ibuprofen to relieve pain
2-Sitz baths
3-Surgical drainage
4-Antibiotics
5-Marsupialization
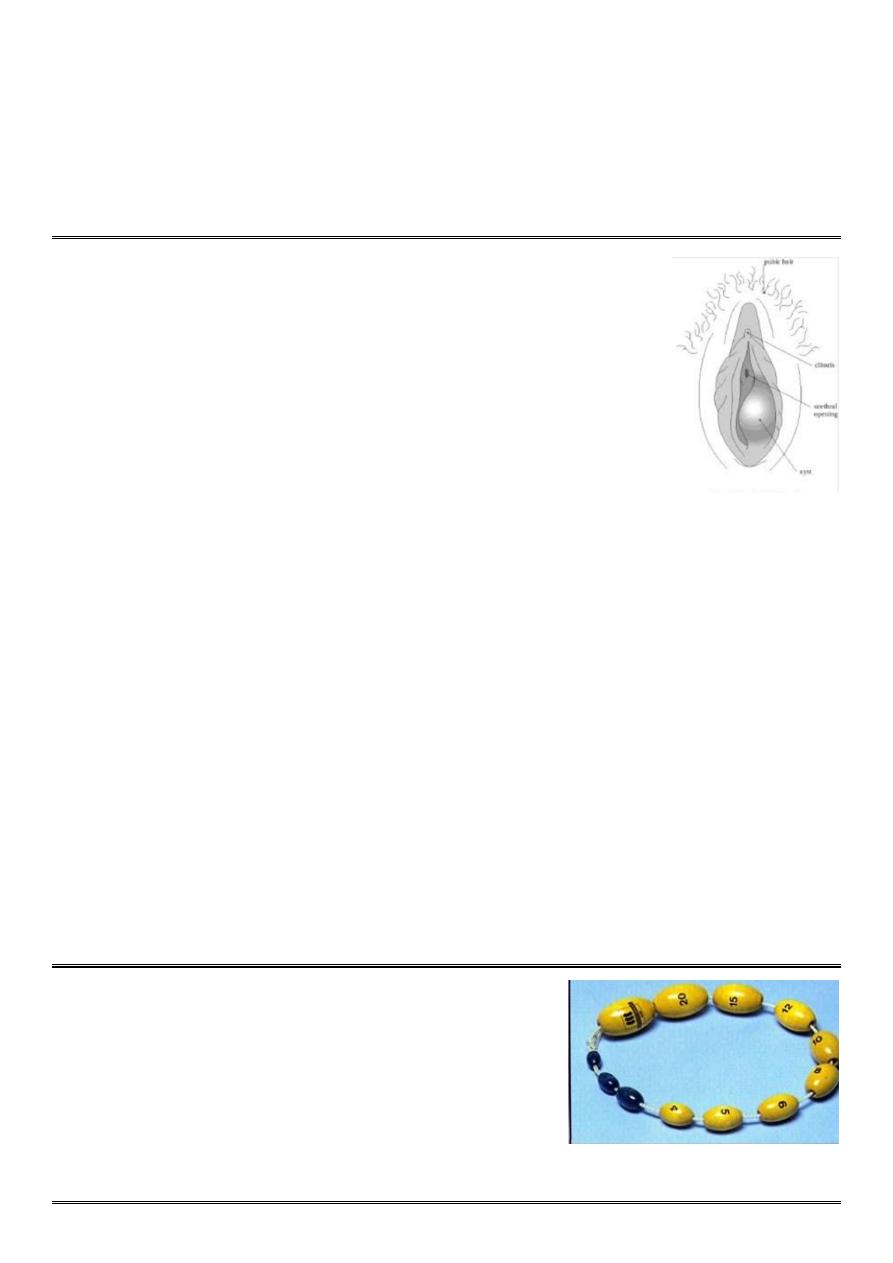
Q1: Name this instrument
Q2: What is the indication of it?
=============
Answer 1 ==> prader orchidometer
Answer 2 ==>
it is a medical instrument used to measure the volume of the testicles
during puberty.

Q1: What is your diagnosis?
Q2: What are the causes?
Q3: What are the signs?
Q4: How you treat this condition?
============
Answer 1 ==> Precocious puberty
Answer 2 ==>
1-Gonadotrophin dependent (idiopathic, congenital, irradiation, surgery, sever head
trauma, tumors)
2-Gonadotrophin independent (virilisation of female (CAH), feminisation of boy
(estrogen producing leydig tumor), adrenal tumor, ovarian tumor, exogenous
androgens, estrogen, HCG-secreting tumor (teratoma)).
Answer 3 ==>
1-developed breasts, hair in the armpits and genital areas, fast rate of growth and fully grown genitals.
2-For some children, there may be voice change due to hormone secretion and growth of hair on face and above the
upper lip.
Answer 4 ==>
1-Psychological support
2-GnRH agonist
3-Treat systemic disease
4-Surgery to remove tumor.
Q1: What is your diagnosis?
Q2: What is the cause?
Q3: What are the clinical presentation?
Q4: How you investigate for this condition?
Q5: How you treat such condition?
===========
Answer 1 ==> ambiguous genitalia
Answer 2 ==> Congenital Adrenal Hyperplasia
Answer 3 ==>
Clinical presentation in new born female:
1-Enlargement of clitoris.
2-Excessive fusion of genital fold.
3-Thickining & rugosity of labia majora.
4-Internal genital organs are present.
5-Dangerous salt losing syndrome.
Affected male => presented at age of 1-4 weeks with failure to thrive, reccurent vomiting, dehydration, hypotension,
shock.
Answer 4 ==>
1-Karyotype
2-17a hydroxyprogesterone
3-Electrolyte abnormality
4-Pelvic US
Answer 5 ==>
1-Medical control of underlying disorder (Cortisol, correction of electrolyte disorder)
2-Surgical correction of underlying anatomical abnormality (Reduction of clitoris, Clitoroplasty, Division of the fused
labia)
Q1: What is your diagnosis?
Q2: What are the clinical feature?
Q3: How you manage this condition?
=============
Answer 1 ==> Turner's syndrome
Answer 2 ==>
1-edema of hand & feet
2-Short stature
3-Absent secondary sexual characteristics
4-Wide carrying angle of the arms
5-Webbed neck
6-Broad chest with widly spaced nipples
7-Streak ovaries
8-Normal internal genital organs
Answer 3 ==>
Investigations:
1-Do Karyotype
2-Marked elevation of LH, FSH,
3-Reduced Estrogen
4-US (Cystic hygroma).
Treatment:
1-Induction of puberty by estrogen
2-Induction of menstruation by progesterone
3-Growth hormone
Q1: What is your diagnosis?
Q2: What are the clinical feature?
Q3: How you manage this condition?
=============
Answer 1 ==> Klinefelter syndrome
Answer 2 ==>
1-Small azospermic testis
2-abnormal secondary sexual characteristics
3-Gynecomastia
4-infertile or reduced fertility.
Answer 3 ==>
Investigations:
1-Testosterone is low normal
2-raised FSH, LH, estrogen.
Treatment:
1-Androgen
2-Reduction mammoplasty.
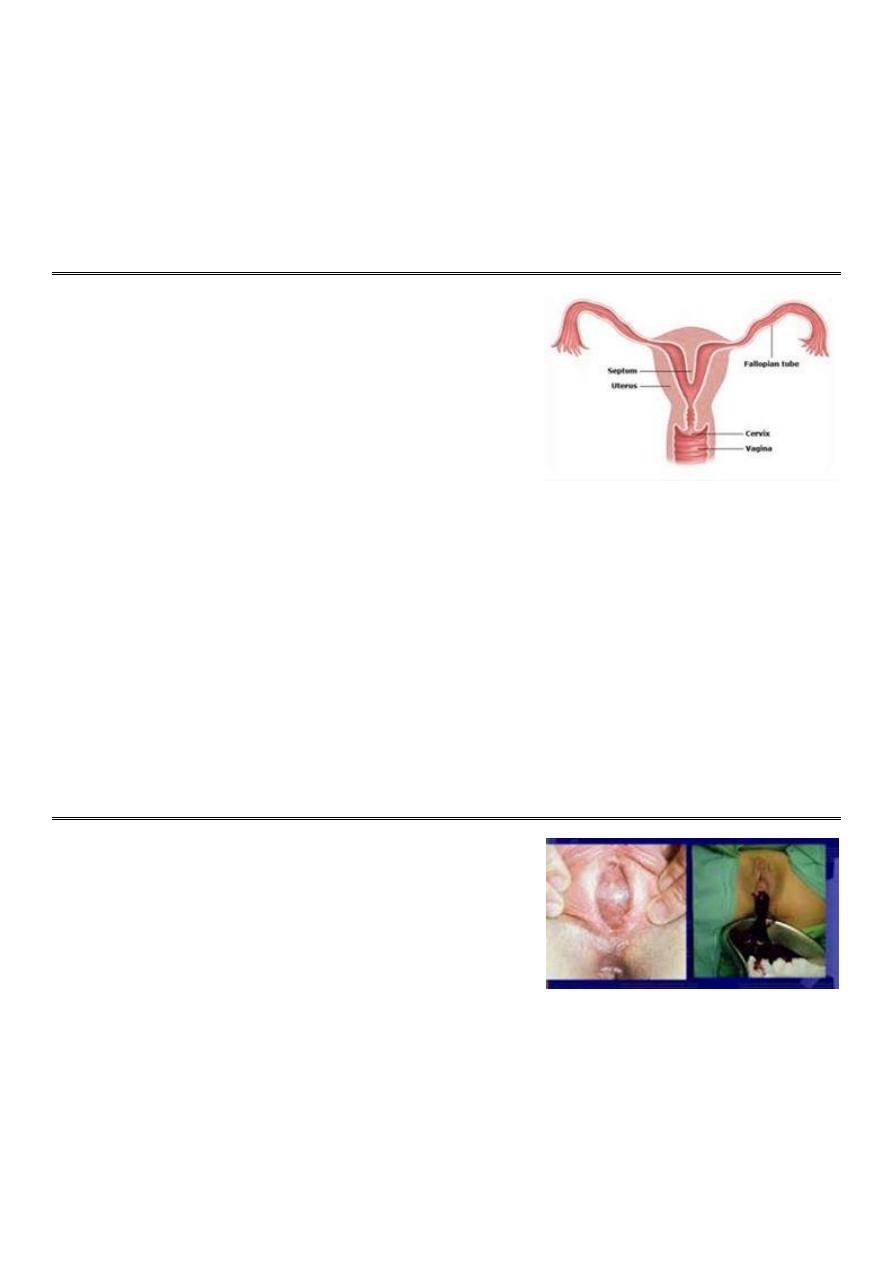
Q1: What is your diagnosis?
Q2: What are the symptoms?
Q3: How you diagnose it?
Q4: What are the treatment?
===========
Answer 1 ==> Septate uterus
Answer 2 ==>
1-Asymptomatic
2-Dysmenorrhoea
3-Dyspareunia
4-Pelvic pain
5-Infertility
6-Recurrent miscarriage
7-Malpresentation
8-Preterm labour
9-Rarely ectopic pregnancy.
Answer 3 ==>
Use pelvic US, CT, MRI, sonohistogram, HSG, hysteroscopy, laproscopy.
Answer 4 ==>
uterine septa can be excised with hysteroscopy.
Q: 16 years old female presented with primary amenorrhea, on
examination the doctor see this picture, what is your diagnosis, and how
do you manage such condition?
==============
Diagnosis: Imperforated hymen
Management:
1-History ==> primary amenorrhea, intermittent cyclical abdominal pain (dysmenorrhea), difficulty with micturition and
defecation, retention of urine in some cases.
2- Examination ==> Normal stature and have normal secondary sexual characteristic, abdominal mass, vulval
inspection (tense bluish bulging membrane), rectal examination (mass at the vagina).
3- Investigations ==> US, Laparoscopy, Laparotomy.

4- Treatment ==> After explanation of the condition and obtaining parents consent, a cruciate incision (+) in the hymen
allows drainage of the retained menstrual blood, also give antibiotics. From medico-legal point of view, the girl must be
given a report confirm that the hymen was opened by surgical operation as treatment.
Q1: What is your diagnosis?
Q2: What are the causes?
Q3: What are the clinical presentation?
Q4: What are the useful investigations?
Q5: How you treat such condition?
=============
Answer 1 ==> Hirsutism
Answer 2 ==>
1-adrenal disorder (congenital or adult onset adrenal hyperplasia, adrenal producing tumors)
2-ovarian disorders (PCOS, androgen producing tumor, chronic anovulation)
3-pituitary disorders (cushing's syndrome, acromegaly)
4-drugs (phenytoin)
5-intrinsic factors (genetic, racial, familial, idiopathic)
6-intersex problem (turner's syndrome)
Answer 3 ==>
1-male pattern of hair distribution
2-features of PCOS, thyroid disease, Cushing syndrome
3-signs of virilization
4-signs of insulin resistance
5-galactorrhea
6-pelvic mass
Answer 4 ==>
1-free testosterone
2-17 hydroxyprogesterone
3-LH:FSH ratio >3
4-5a RA
5-pelvic US, CT, MRI,
6-Dexamethasone suppression test
Answer 5 ==>
1-General => reassurance, stop smoking, weight reduction.
2-Specific => ovarian suppression (OCP), adrenal suppression (corticosteroids), anti-androgens (spironolactone),
5aRA inhibitors (Finasteride), Insulin sensitizer (Metformin).
3-Local => suppress hair growth, remove hair pigment, temporary depilation, temporary epilation, permanent removal.
4-Surgery.
Q1: What is your diagnosis?
Q2: Enumerate its types
Q3: What are the possible complications?
Q4: What are the Differential diagnosis?
Q5: How you manage such condition
=============
Answer 1 ==> Uterine Fibroid
Answer 2 ==>
1-Submucous fibroid > Located adjacent to and bulging into the endometrial cavity.
2-Intramural fibroid > Located centrally within the myometrium.
3-Subserosal fibroid > Located at the outer border of the myometrium.
4-Pedunculated fibroid > Attached to the uterus by a narrow pedicle containing blood vessels.
5-Cervical fibroids > arise from the cervix.
== Types of fibroid that interfere with pregnancy > submucus, intrameural.
Answer 3 ==>
1-Malpresentation
2-Obstruction of the birth canal
3-PPH
4-anemia
5-Urinary or bowel obstruction
6-Ureteral injury or ligation
Answer 4 ==>
1-Endometriosis
2-Uterine cancer
3-Adenomyosis
4-Myometrial hypertrophy
5-Congenital anomalies
6-Endometrial hyperplasia
7-polyp
Answer 5 ==>
History:
1-Asymptomatic when the fibroid is small.
2-History of abnormal vaginal bleeding like menorrhagia, inter-menstrual bleeding (if pediculated), dysmenorrhea.
3-Vaginal discharge if infected.
4-Pressure symptoms
5-Subfertility
6-Anemia
7-Polycythemia
8-Could lead to abortion, Pre-term labor, Placental abruption, Mal-position, mal-presentation,Obstructed labor, Post-
partum hemorrhage, Pain
Examination:
1-Abdominal mass
2-Different by pregnancy there is fundal height like pregnancy but there is no fetal heart (fetal heart = double maternal
pulse).
Investigations:
1-Hemoglobin concentration will help to indicate anemia
2-Ultrasonography => confirm the diagnosis, distinguish between a fibroid and an ovarian mass, helpful to exclude
hydronephrosis from pressure on the ureters by large fibroid.
3-HSG, Saline hysterosonography, MRI, IVP, hysterscopy.
Treatment:
1-Treat the excessive heavy cycle (Progesterone only therapy,COCP, LNG releasing IUD)
2-GnRH agonists
3-Supportive measures => PAP smear, endometrial sampling,Correct Hb,Prophylactic antibiotics,Prophylactic heparin
postoperative.
4-hysteroscopic removal
5-myomectomy with uterine conservation, or hysterectomy
6-Uterine artery embolization (UAE)
== Treatment depend on > type of fibroid, number of fibroid, symptoms, patient wish, family number.
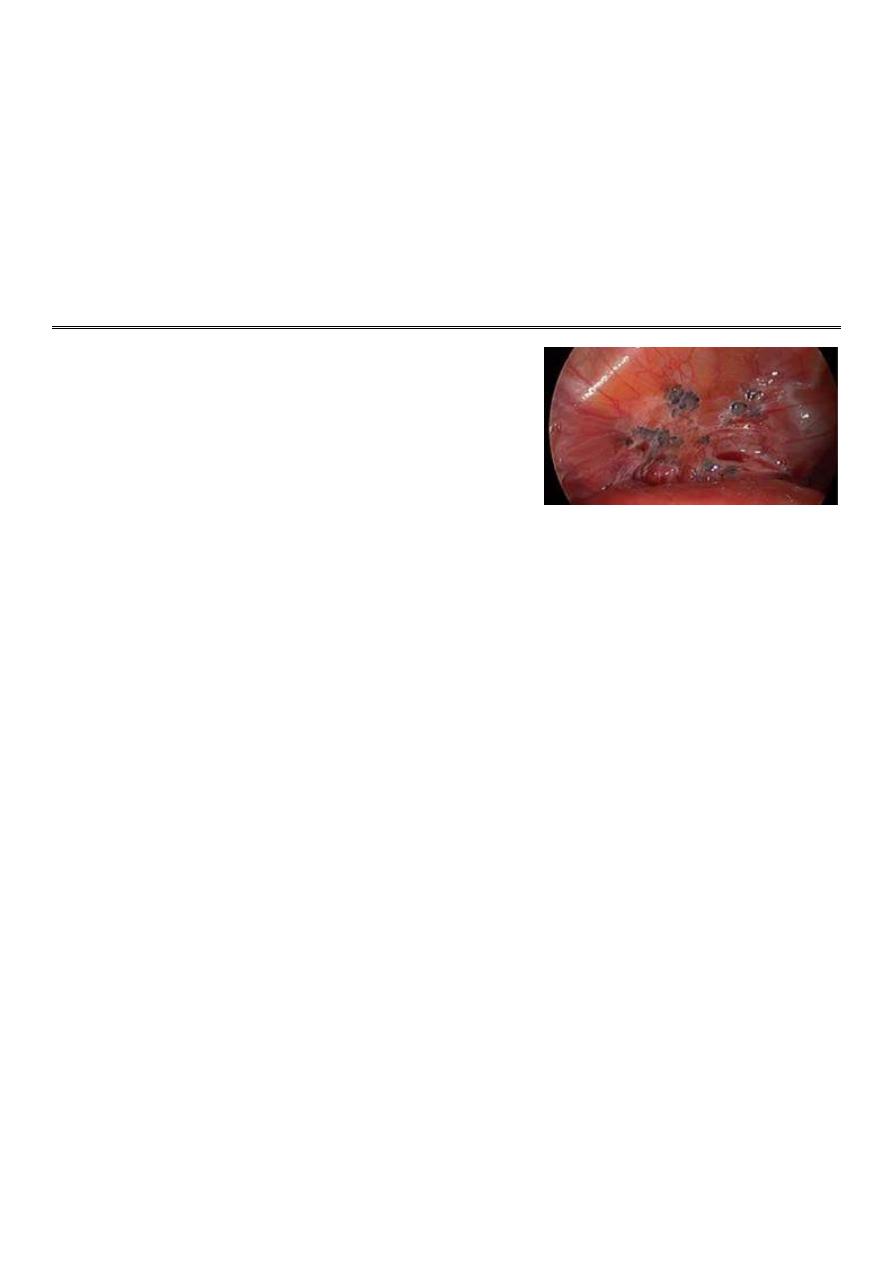
Q1: What is your diagnosis?
Q2: What are the risk factors?
Q3: What are other possible deferential diagnosis?
Q4: How do you manage such condition?
===========
Answer 1 ==> Endometriosis
Answer 2 ==>
1-Family history of endometriosis
2-Early age of menarche
3-Heavy bleeding during menses
4-Inverse relationship to parity
5-Delayed childbearing
6-Defects in the uterus or fallopian tubes
Answer 3 ==>
1-Chronic salpingo-oopheritis
2-Ovarian cyst
3-malignant ovarian tumours
4-Small myoma
5-Acute abdomen
Answer 4 ==>
History:
1- Dysmenorrhea, Heavy or irregular bleeding
2-Pelvic pain, Lower abdominal or back pain
3-infertility, Dyschezia, Bloating, nausea, vomiting
4-Pain on micturition and/or urinary frequency
Physical examination:
1-nonspecific pelvic tenderness
2-Ovarian involvement may present with adnexal tenderness or masses
3-fixed uterine retroversion
Investigation:
Laparoscopy with biopsy is the only definitive way to diagnose endometriosis.
Treatment:
1-NSAID, Oral contraceptive pills, Danazol, Gestrinone, Progestagens, Gonadotrophine releasing hormone agonists.
2-conservative surgery (LASER, Co2 diathermy, Drainage of endometriotic cyst),
3-Definitive surgery (TAH + BSO)
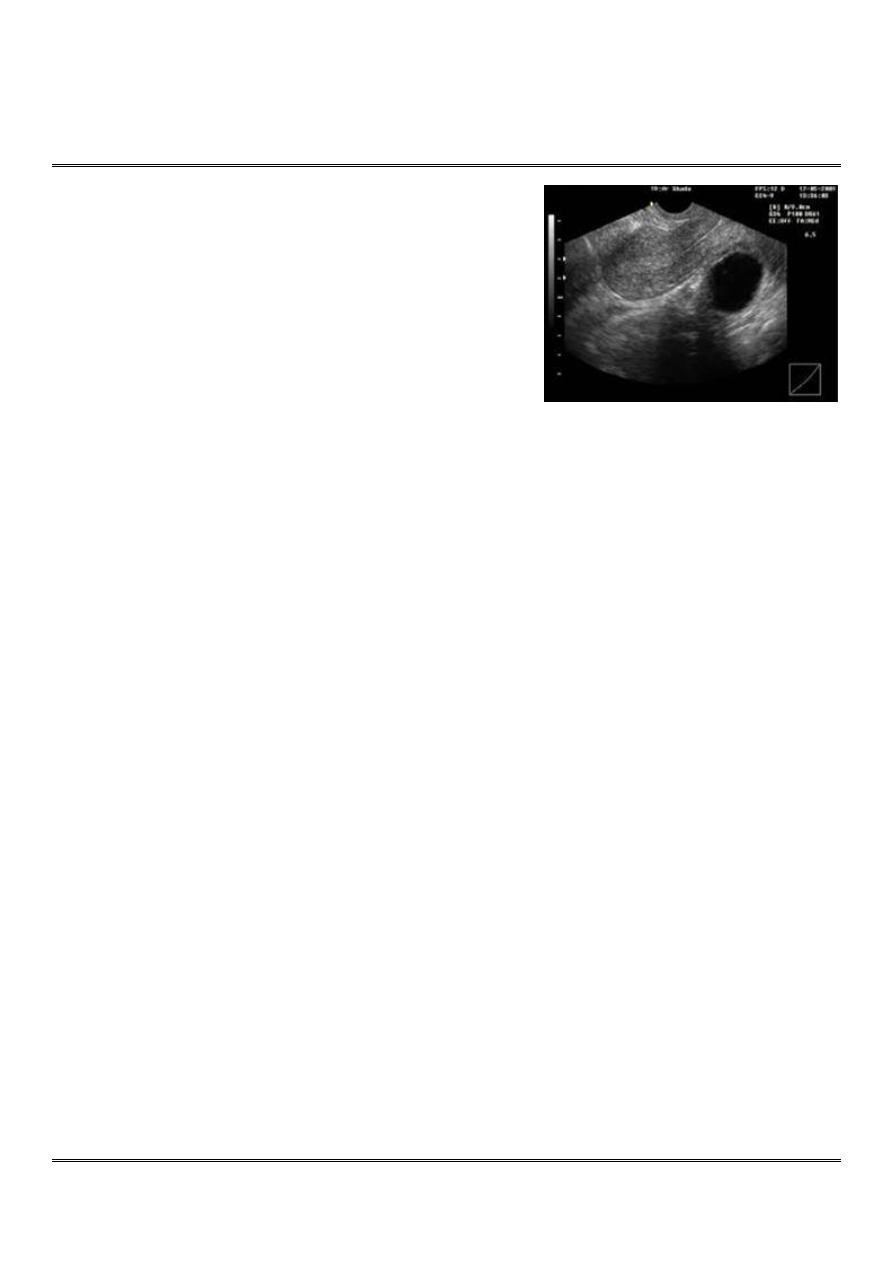
Q1: Describe the US features
Q2: What is your diagnosis?
Q3: What are other differential diagnosis?
Q4: How to manage such condition?
===========
Answer 1 ==>
regular outline, smooth, no sepitation, no nucleation, no hemorrhage,
no calcifications, thin wall, contain homogenous radiolucent fluid.
Answer 2 ==> Simple ovarian cyst
Answer 3 ==>
1-graafian follicular cyst
2-corpus luteal cyst
3-Hemorrhagic cyst
4-ovarian carcinoma
5-polycystic ovarian syndrome
Answer 4 ==>
History and examination:
1-Small cyst is asymptomatic.
2-Gradual abdominal distention.
3-Lower abdominal pain.
4-Irregular cycles
5-Breast tenderness
6-Frequency.
7-Altered bowel habits.
8-Hirsutism.
9-Easily fatigability.
10-Weight gain.
Investigations:
1-Hb level, Blood group and Rh.
2-Ultrasound of the abdomen
3-CT / MRI
4-LH and FSH level.
5-Cancer markers (CA-125)
Treatment:
1-Less than 3 cm => resolve spontaneously during 2-3 months (cycles).
2-Persistent for 2-3 months => use combined oral contraceptive pills (COCP)
3-Cyst with symptoms => like pain, give pain killer and COCP.
4-Large symptomatic cyst => surgical removal by laparotomy and take biopsy to exclude malignancy.
5-Malignant cyst => surgery with radiotherapy or chemotherapy.
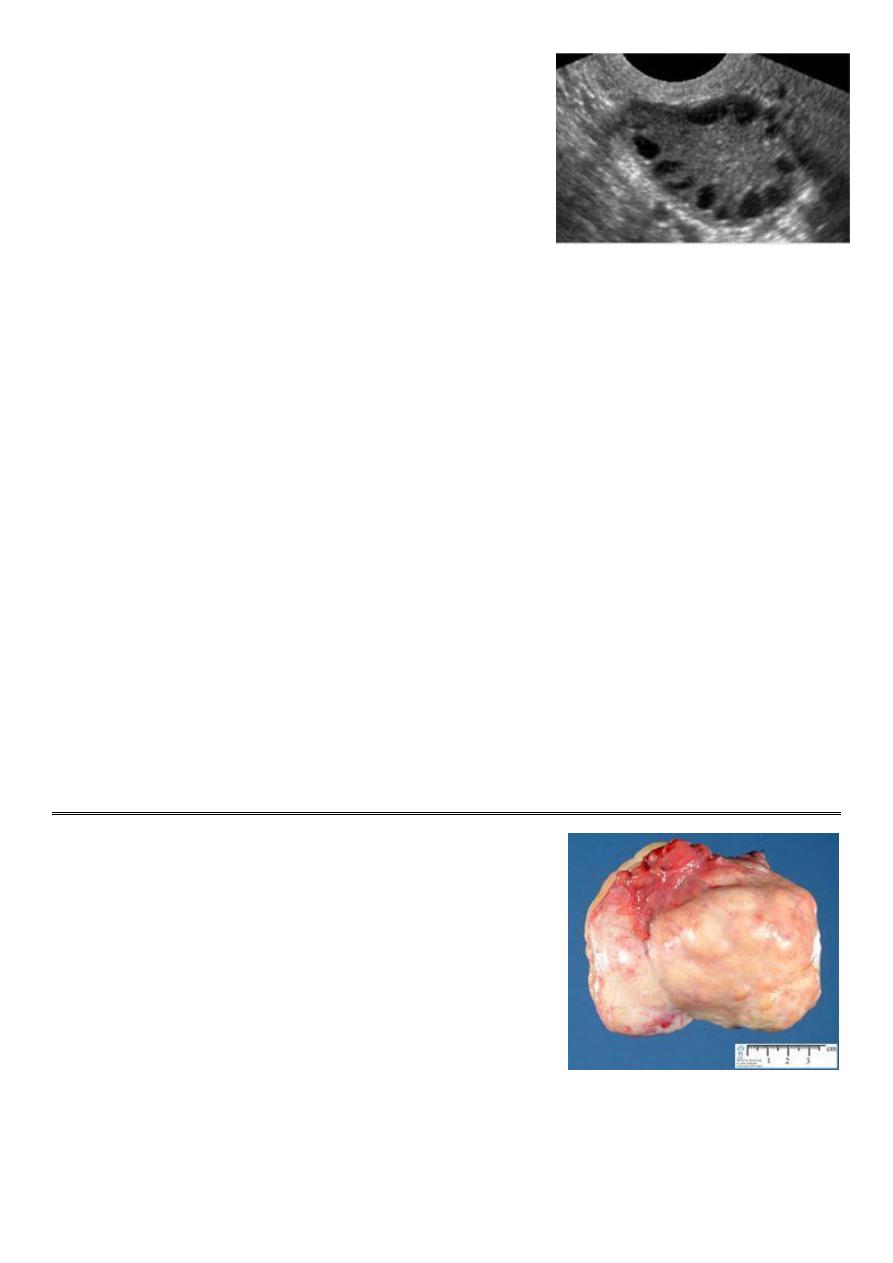
Patient presented with irregular bleeding and have this sonography.
Q1: Describe this sonography.
Q2: What is your diagnosis?
Q3: Write other symotms
Q4: What are the menstural abnormality with this condition?
Q5: What are the investigations you need?
Q6: How to treat such condition?
============
Answer 1 ==>
bliateral ovaries contain more than 10 follicles each measure 2-5 mm arranged in necklace apperance, and there is
increased ovarian stroma with or without increased of ovarian volume more than 10 cm3.
Answer 2 ==> polycyctic ovarian syndome.
Answer 3 ==>
1-hirsutism, acne.
2-Subfertility
3-Weight gain and Obesity.
4-Recurrent miscarriage.
5-Acanthosis nigricans
Answer 4 ==> oligomenorrhea or amenorrhea
Answer 5 ==>
1-Increased free testosterone, LH/FSH more than 3 (reversed ratio)
2-Increase insulin (impaired glucose tolerance)
3-Decrease level of sex hormone binding globulin
Answer 6 ==>
1- medical (COCP, ovulation induction)
2-Metformin: for D.M
3-Symptomatic relieve by anti-androgens
4-surgical (wedge resection, IVF)
5-weight reduction
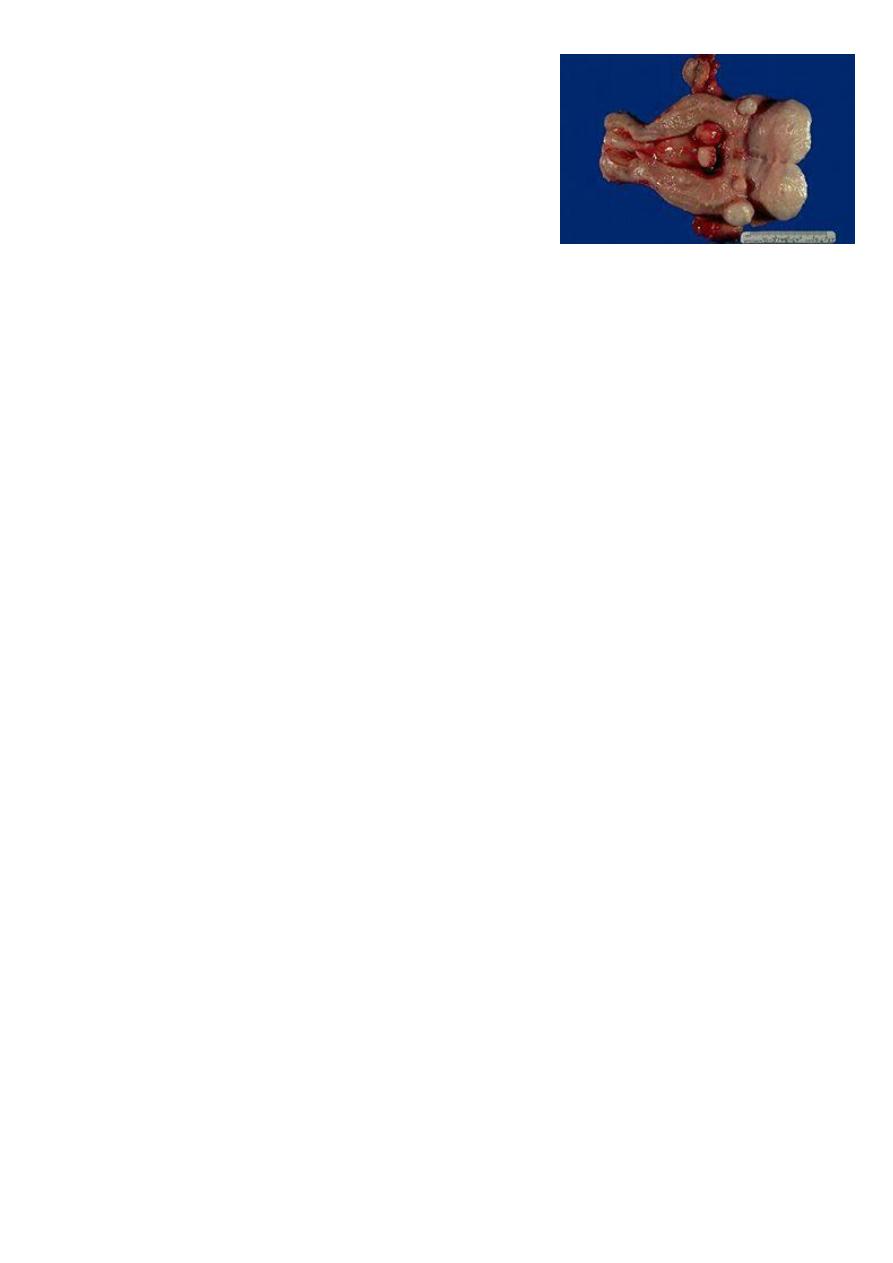
The organ in the photo is ovary,
Q1: What is your diagnosis?
Q2: What are the risk factors?
Q3: What are the clinical presentation?
Q4: Write some useful investigations
Q5: How you can treat this disease?
================
Answer 1 ==> ovarian neoplasm
Answer 2 ==>
1-Nuliparaty
2-Intrauterine device
3-Endometriosis
4-Cigarette smoking
5-Obesity
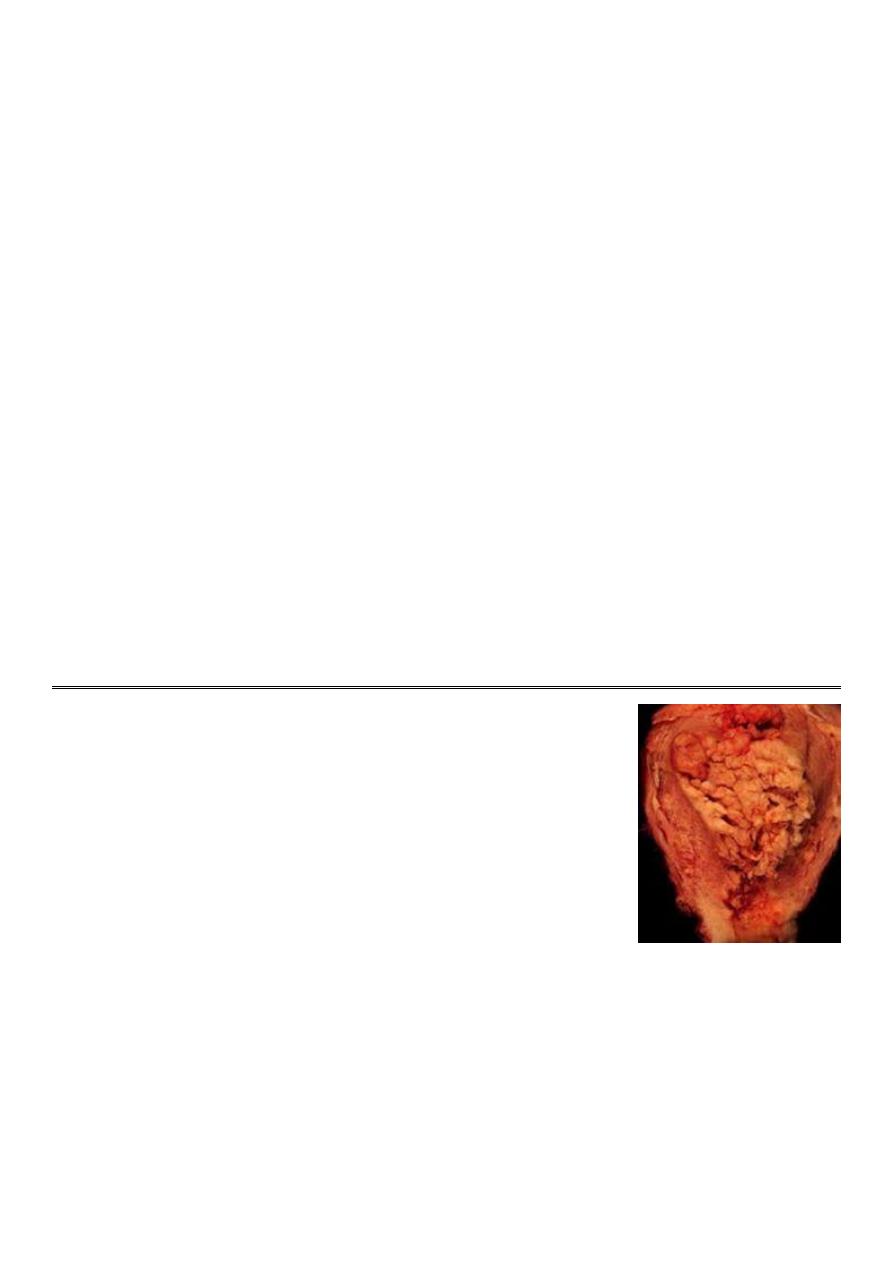
Answer 3 ==>
Symptoms:
1-Functioning tumors.
2-Nonfunctioning tumors swelling, pressure symptoms, pain, menstrual disturbances, ovarian cachexia
The following suggest malignancy:
1-age: mostly postmenopausal
2-pain: chronic and persistent
3-rapid course
4-bilaterality
5-Solidity ( variegated consistency )
6-fixity
7-metastases :nodules in DP, lymph nodes
8-ascitis
9-edema LL
10-cachexia
Answer 4 ==>
1-TVS
–masses
2- Tumor markers
– CA-125, LPA
3-CT
– assess spread to LN, pelvic and abdominal structures
4-MRI
– best for distinguishing malignant from benign tumors
Answer 5 ==>
1-Depends on => Staging, Tumor type, Age, Desire for future fertility
2- stage Ia =>Complete surgery: TAH/BSO + omentectomy + lymphadenectomy:
3- Stage Ib,c =>Conservative surgery: unilateral adnexectomy
4- for all other stages => Cytoreductive surgery: TAH/BSO + omentectomy + lymphadenectomy + may be bowel
resection & anastomosis:
5-Chemotherapy.
6-Radiotherapy.
Q1: What is your diagnosis?
Q2: What are the risk factors?
Q3: How this condition is spread?
Q4: Manage this condition.
============
Answer 1 ==> Endometrial carcinoma
Answer 2 ==>
1-high levels of estrogen
2-endometrial hyperplasia
3-obesity, hypertension
4-nulliparity, infertility, early menarche, late menopause
5- diabetes, Tamoxifen
6-pelvic radiation therapy
7-breast cancer, ovarian cancer
8-heavy daily alcohol consumption
Answer 3 ==>
1-Direct extension
2-Transtubal
3-Lymphatic
4-Hematogenous (Lung most common, Liver, brain, bone)

Answer 4 ==>
History and examination:
1-Post-menopausal bleeding, Intermenstrual bleeding, menorrhagia,
2-Watery or purulent vaginal discharge (blood stained)
3-Pain
4-Abnormal screening test.
Investigations:
1-Pap smear
2-Endometrial curettage, dilation and curettage (D&C),
3-Hysteroscopy, Endometrial biopsy or aspiration,
4-Transvaginal ultrasound, Sonohysterography
5-Pipelle biopsy curettage
6-TruTest
7-Magnetic resonance imaging (MRI).
Treatment:
1-Stage IB or less: total hyst/BSO/PPALND, cytology
2-Stage IC to IIB: total hyst/BSO/PPALND, cytology, adjuvant pelvic XRT
3-Stage III: total hyst/BSO/PPALND, cytology, adjuvant chemotherapy
4-Stage IV: palliative XRT and chemotherapy
Q1: Name the procedure
Q2: At which age you can start to do it?
Q3: What is the purpose of this test?
Q4: How many times are needed to do this test?
Q5: Which women not need to do this test?
Q6: What are the preparation needed for this test?
Q7: What are the methods for this test?
Q8: What are the indications for this test?
Q9: Which tools you need for this test?
============
Answer 1 ==> pap smear
Answer 2 ==>
should begin at age 21 years and not before age 21 because it may lead to unnecessary and harmful evaluation and
treatment in women at very low risk of cancer.
Answer 3 ==>
Is a screening test for asymptomatic Women to detect treatable pre-invasive squamous abnormalities of the Cervix, it
is not diagnostic-rather screening test to detect early changes on the cervix.
Answer 4 ==>
1-Annual cervical cytology screening is recommended for women aged 21
–29 years.
2-Women aged 30 years and older who have had three consecutive cervical cytology test results that are negative for
intraepithelial lesions and malignancy may be screened every 2-3 years.
3-women with any of the following risk factors may still require more frequent cervical cytology screening =>human
immunodeficiency virus, immunosuppressed, exposed to diethylstilbestrol in utero, previously treated for CIN 2, CIN 3,
or cancer
Answer5 ==>
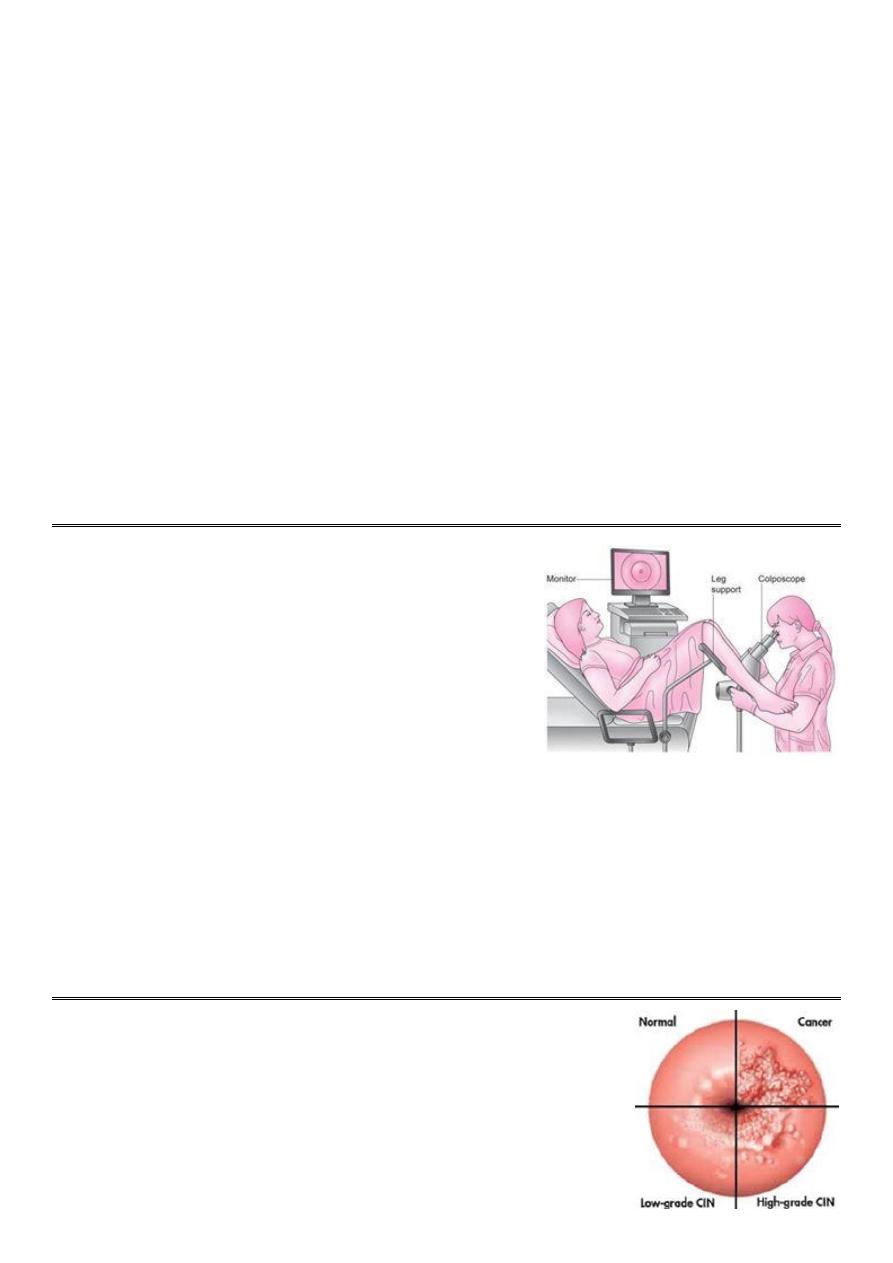
1-Virgin patient.
2-Total Hysterectomy for benign disease.
3-Recent result of pap smear.
4-Age over 65 and over 10 benign Pap Smears.
Answer 6 ==>
1-To prepare for the Pap test, for two days before the test ,women should avoid =>Vaginal Douching, using tampons,
sexual intercourse, Using birth control foams, creams, or jellies or vaginal medications or creams.
2-The ideal time for a woman to have a Pap Smear is five days after her menstrual period has ended.
3-Exfoliated cells are collected from the transformation zone of the cervix by Use spatula of different size or brush.
Answer 7 ==>
1-Conventional cervical (Pap) smear test
2-Liquid based cytology (LBC) test
Answer 8 ==>
1-For screening of malignant and premalignant conditions.
2-For checking degree of infection (HPV- 16-18-31-35).
Answer 9 ==>
spatula or cytobrush, slide, cusco speculum, gloves
Q1: What is this device?
Q2: Why you use this device?
Q3: What are the methods of this exam?
==========
Answer 1 ==> Colposcopy
Answer 2 ==>
1-It is a binocular operating microscope with magnification of 5-20
times.
2-Indicated for further investigation of smear abnormalities.
3-It has been used to examine the cervix in detail to:
*Identify dysplastic abnormalities on the ectocervix.
*Detect changes in the cellular pattern and vascularity of the covering epithelium.
*Allow the accurate localization of the abnormal epithelium.
*Exclude an invasive process.
Answer 3 ==>
1-Saline method.
2-Classical or extended method.
3-Iodine test method.
Q1: What is your diagnosis?
Q2: What are the causes of such condition?
Q3: What are the risk factors?
Q4: What are the differential diagnosis?
Q5: How you can manage this condition?
=============
Answer 1 ==> Cervical cancer

Answer 2 ==>
1-human papillomavirus (HPV) infection,
2-HIV infection.
3-chlamydia infection.
4-stress and stress-related disorders.
5-dietary factors.
6-hormonal contraception.
7-multiple pregnancies.
8-exposure to the hormonal drug diethylstilbestrol (DES) .
Answer 3 ==>
1-Young age at first coitus(20years)
2-Multiple sexual partners.
3-Young age at first pregnancy.
4-High parity .
5-Low socioeconomic state.
6-Smoking.
Answer 4 ==>
1-Cervicitis.
2-Cervical ectropion.
3-Endometrial carcinoma.
4-Pelvic inflammatory disease (PID).
5-Vaginal cancer.
6-Metastatic cancer to cervix (rare).
7-Tuberculosis.
8-Syphilitic chancre.
9-Choriocarcinoma.
Answer 5 ==>
History and examination:
1-Asymptomatic.
2-Vaginal bleeding, contact bleeding.
3-Profuse vaginal discharge.
4-Cervical mass.
5-Moderate pain.
6-Fistula formation
7-Symptoms of distant metastases may be present as enlarged inguinal and supraclavicular L.N. metastases in the
abdomen, lungs or else where in case of advanced disease.
8-Systemic manifestation of advanced malignancy as: loss of appetite, weight loss, fatigue, pelvic pain, back pain, leg
pain, single swollen leg, heavy bleeding from the vagina, leaking of urine or feces from the vagina, and bone fractures.
Investigations:
1-Complete blood cell count
2-Renal functions test
3-Hepatic functions test
4-Chest radiograph
5-CT scan of the abdomen and pelvis
6-Barium enema
7-Intravenous urogram.
Treatment:
1-Conization or simple hysterectomy
2-Radical hysterectomy
3-Chemoradiation therapy
*Surgery > should only be considered an option for early disease (stage 1 and stage 11a).
*Early cervical cancers (stage I and IIA) may be treated by either procedure.
*Radiotherapy is the treatment of choice once the disease has spread beyond the confines of the cervix and vaginal
fornices, when surgery is not effective. Stage Ib2-IVa
Q1: What is your diagnosis?
Q2: What is the classification of this condition?
Q3: What are the symptoms?
Q4: Which investigations you need?
Q5: How to treat such condition?
=============
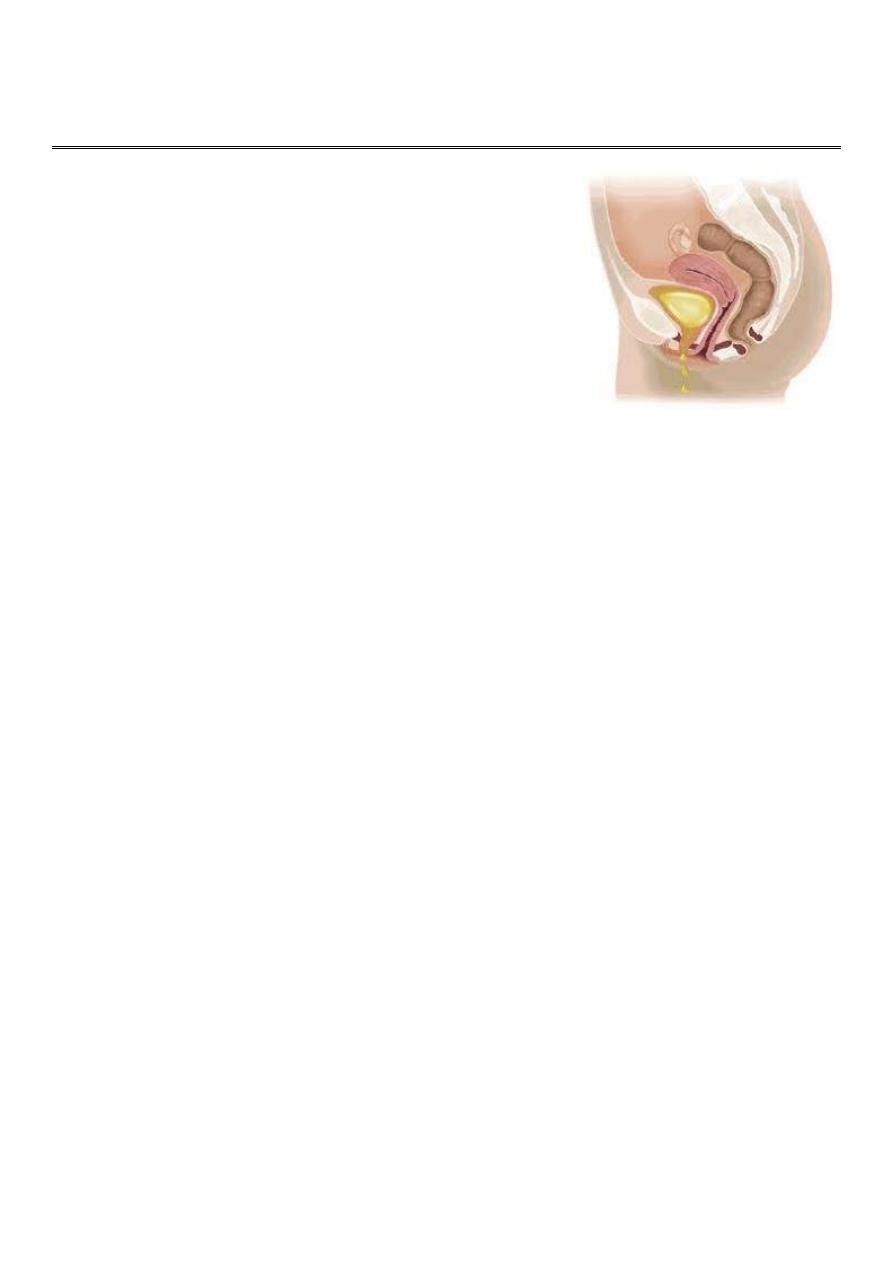
Answer 1 ==> Urinary incontinence
Answer 2 ==>
1-Stress incontinence (most common)
2-Urge incontinence
3-Overflow incontinence
4-Continuous incontinence
Answer 3 ==>
Symptoms before voiding (storage phase):
1-Stress incontinence.
2-Urge incontinence.
3-Urgency: intense desire to void.
4-Frequency: urination more than usual voiding rate.
5-Decrease or increase bladder sensation of fullness.
Symptoms during voiding (void phase):
1-Poor stream (voiding difficulty).
2-Intermittent stream.
3-Hesitancy.
Symptoms after voiding (post voiding phase):
1-Post voiding drippling of urine
2-Feeling of incomplete emptying.
3-Dysuria, hematuria, pyuria.
Answer 4 ==>
1-Mid-stream urine examination
2-Urinary diary test
3-Pad test
4-Three swab test:
5-Flowmetery:
6-Vedio-cystourethrography
7-Radiological tests: US, MRI, IVU
8-Tests for sphincter = > Nerve conduction study, Urethral pressure profiometery.
Answer 5 ==>
Overflow insentience:
1-Treated by urologist and neurologist.
2-End by continuous catheter.
Stress incontinence:
1-Pelvic floor exercise.
2-Pelvic floor muscle stimulation.
3-Vaginal cone.
4-Drugs: SSRI (lead to nausea and vomiting).
5-Surgery (Colpo suspension, TPT, Artificial sphincter).
6-Local injection of strengthening materials like collagen.
Detrusor overactivity:
1-Bladder training:
2-Drugs (Selective anticholinergic, TCA, Anti-diuretics, Gabapentin)
3-Surgery (Sacral nerve stimulation, Tibial nerve stimulation)
4-Use pat or catheterization (suprapubic or self).
Q1: What is your diagnosis?
Q2: What are the causes?
Q3: What are the types of this condition?
Q4: What are the grades of this condition?
Q5: What are the differential diagnosis?
Q6: How you manage this condition?
===============
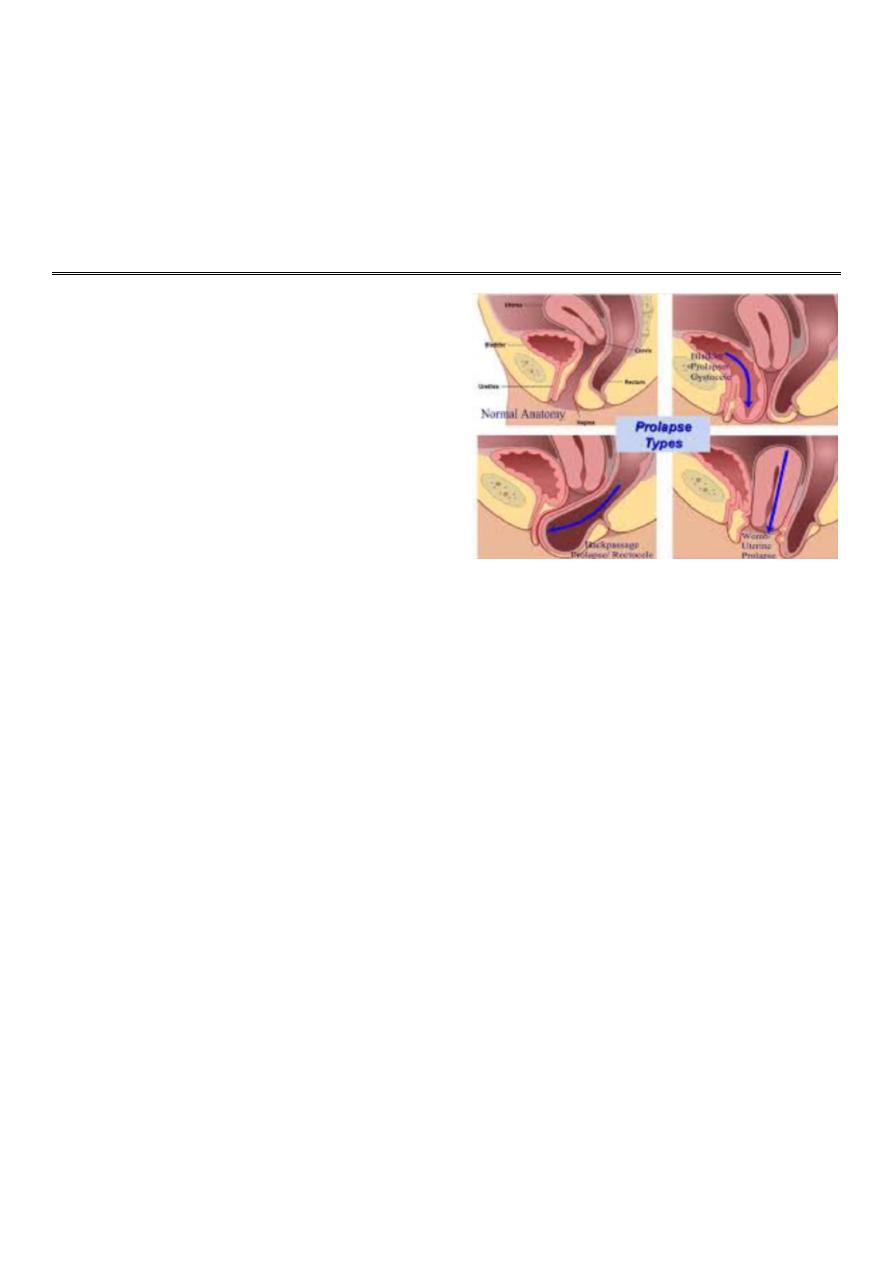
Answer 1 ==> Prolapse
Answer 2 ==>
1-Childbirth and raised intra-abdominal pressure
2-Aging
3-Multiple parity
4-Obstructed labor
5-Congenital (connective tissue defects)
6-Lack of estrogen
7-After hysterectomy
Answer 3 ==>
1-Cystocele > prolapse of the urinary bladder.
2-Urethrocele > prolapse of the urethra.
3-Rectocele > prolapse of the rectum.
4-Enterocele > prolapse of the part of the small intestine.
5-Uterine prolapse > prolapse of the uterus.
Answer 4 ==>
1-Grade1: the uterus reach the vagina.
2-Grade2: the uterus reach the introitus.
3-Grade3: uterus and cervix outside the vagina.
4-Procidentia = complete prolapse = Grade3
Answer 5 ==>
1-Anterior wall prolapse > congenital or inclusion dermoid vaginal cyst, urethral diverticulum.
2-Uterovaginal prolapse > large uterine polyp.
Answer 6 ==>
History and examination:
1-Lump, local discomfort, backache, bleeding/ infection if ulcerated, dyspareunia or apareunia.
2-Rarely, in extremely severe cystourethrocele, uterovaginal or vault prolapse, renal failure may occur as a result of
ureteric kinking.
3-Cystourethrocele
– urinary frequency and urgency, voiding difficulty, urinary tract infection, stress incontinence.
4-Rectocele: incomplete bowel emptying, digitation, splinting, passive anal incontinence.
Investigations:
1-Cystocele > general urine examination, urine microscopy, cystometry, cystoscopy, urethroscopy, urodynamic study.
2-Rectocele > sigmoidoscopy (DDx tumor like fibroma), anoscopy.
3-Uterine prolapse > ulcer swab.
Treatment:
1- Hormonal replacement therapy
2- Treat the infection.
3- Electrical stimulation of the pelvic floor
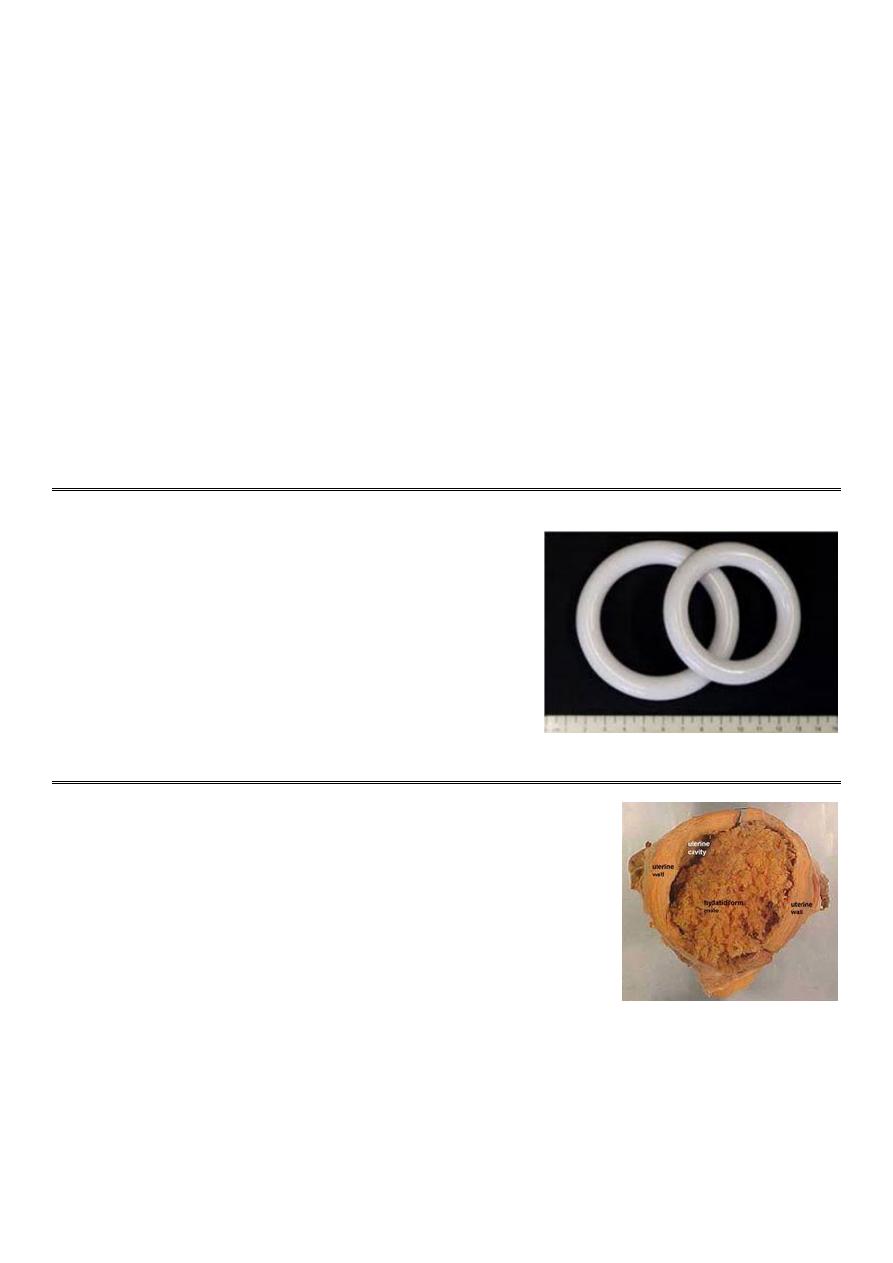
4- Pessary (ring pessary):
5- Vaginal or abdominal hysterectomy
6- Repair of wall like anterior or posterior colporaphy or both.
7- fixing the ligament by uterosacral fixing (use mish between sacrum and uterus).
Prophylaxis:
1-Exercise after delivery (pelvic flow examination).
2-Avoid prolongation of labor especially during second stage of labor.
3-Reduce the number of traumatic delivery.
Pessary (ring pessary):
1-There are multiple types and shapes color and sizes of pessary.
2-Used if patient above 60 years and not fit for anesthesia or have
multiple diseases.
3-Push the uterus to its normal site then fit the ring between the anterior
and posterior vaginal wall.
4-The ring pessary still 3-6 months then take it off and clean and
sterilize it and put it again.
5-Prolonged period of pessary lead to infection, ulcer, pressure.
Patient presented with abnormal vaginal bleeding, and abortion, the hysterectomy
some pathology.
Q1: Name this condition
Q2: Which investigations can detect it?
Q3: How to manage this condition?
Q4: Write about the scoring system of this condition
===========
Answer 1 ==> Gestational trophoblastic disease
Answer 2 ==>
1-Histopathological study
2-US > snow storm appearance due to excessive cystic lesions
Answer 3 ==>
1-Preparation: prepare blood, investigation (CBC, Hb, blood group, cross match, B-hCG).
2-General ansthesia.
3-Suction method for evacuation.
4-If bleeding occur > not use oxytocin but use ergometrine at the end of evacuation.
5-Follow up: Twice weekly for 6 months.
6-Avoid pregnancy to avoid confusion: Best method is condom.
7-Chemotherapy.
Answer 4 ==> Figo scoring or staging:
1-Age of patient > less than 40 years is low risk, more than 40 years is high risk.
2-Previous pregnancy before the mole > H.mole (low risk), abortion (moderate risk), normal pregnancy (high risk).
3-Duration between H.mole and pregnancy > less than 3 months (low risk), more than 1 year (high risk).
4-Level of B-hCG > 1000 (low risk), 1000000 (high risk).
5-Site of metastasis > lung (low risk), brain (high risk).
6-Number of metastasis > large number (high risk), low number (low risk).
7-Size of metastasis > small size (low risk), large size (high risk).
8-Previous chemotherapy > if not take (low risk), if take (high risk).
=== Figo scoring: less than 6 (give one chemotherapy), more than 6 (give multiple chemotherapy).
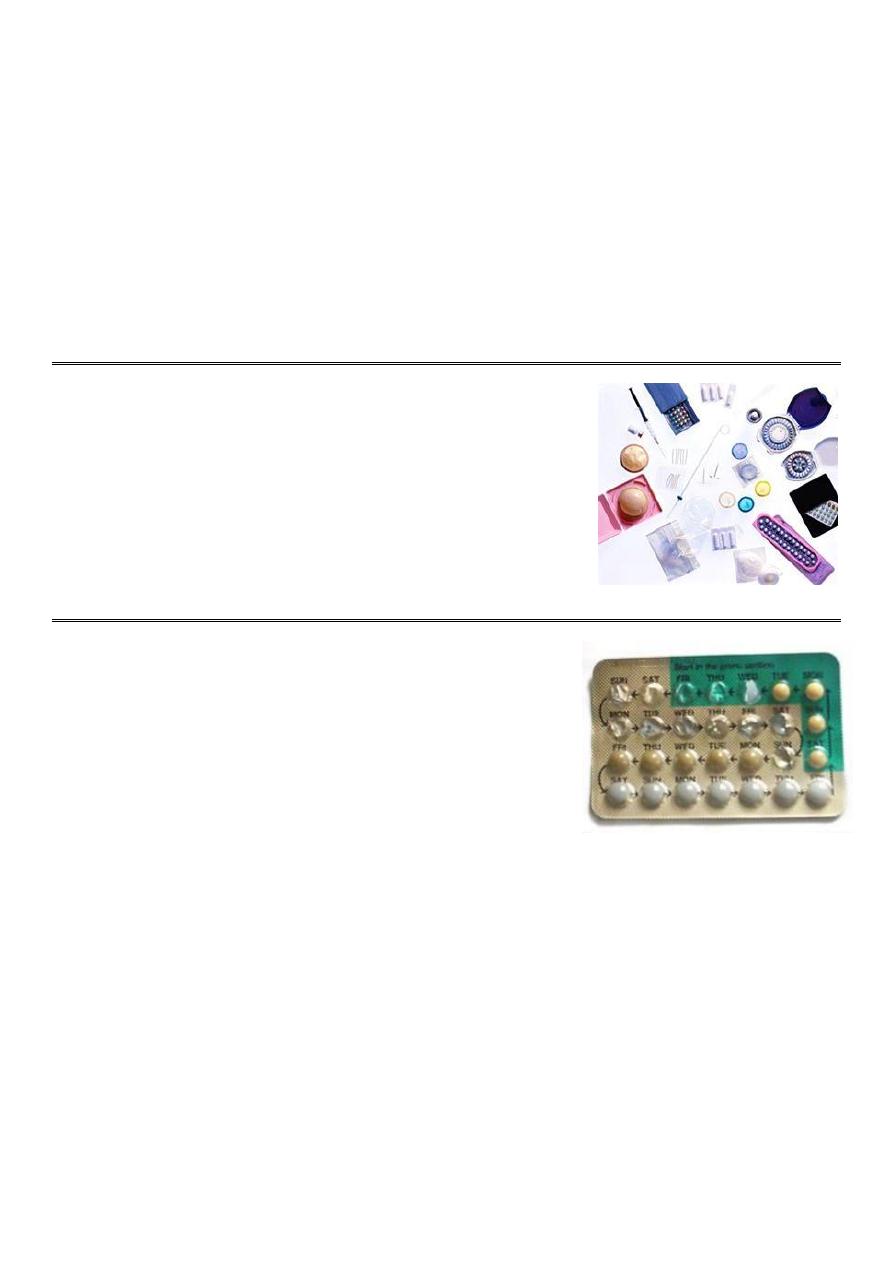
Q: What are the features of the ideal contraceptive method?
1-Highly effective
2-No side effects
3-Cheap
4-Rapidly reversible
5-Widespread availability
6-Acceptable to all cultures and religions
7-Easily distributed
8-Can be administrated by non- health care personnel.
Q1: What is this drug?
Q2: What is the formulation?
Q3: How may pills it contain?
Q4: What is the method of use?
Q5: What are the mode of action?
Q6: What are the contraindications?
Q7: What are the side effects?
Q8: What to do if pills are missed?
Q9: What are other health benefits?
Q10: What are the important questions during history taking?
Q11: What are the causes of failure?
===========
Answer 1 ==> Combined oral contraceptive pills (COCP):
Answer 2 ==>
Synthetic Estrogen (Ethinyl estradiol) + Synthetic progestogens (norethindrone, levonorgestrel, gestodene).
Answer 3 ==>
COCP contain 21 pills that contain the active ingredient, one pill to be taken daily, followed by a 7 placebo pills.
Answer 4 ==>
The patient begins taking the pills on the first day of menstrual cycle then in the next cycles they are administered in
fifth day of the cycle and continue for 21 days, each day at the same time, then discontinued for 7 days to allow for
withdrawal bleeding that mimics the normal menstrual cycle which occur after 3-5 days from stopping pills.
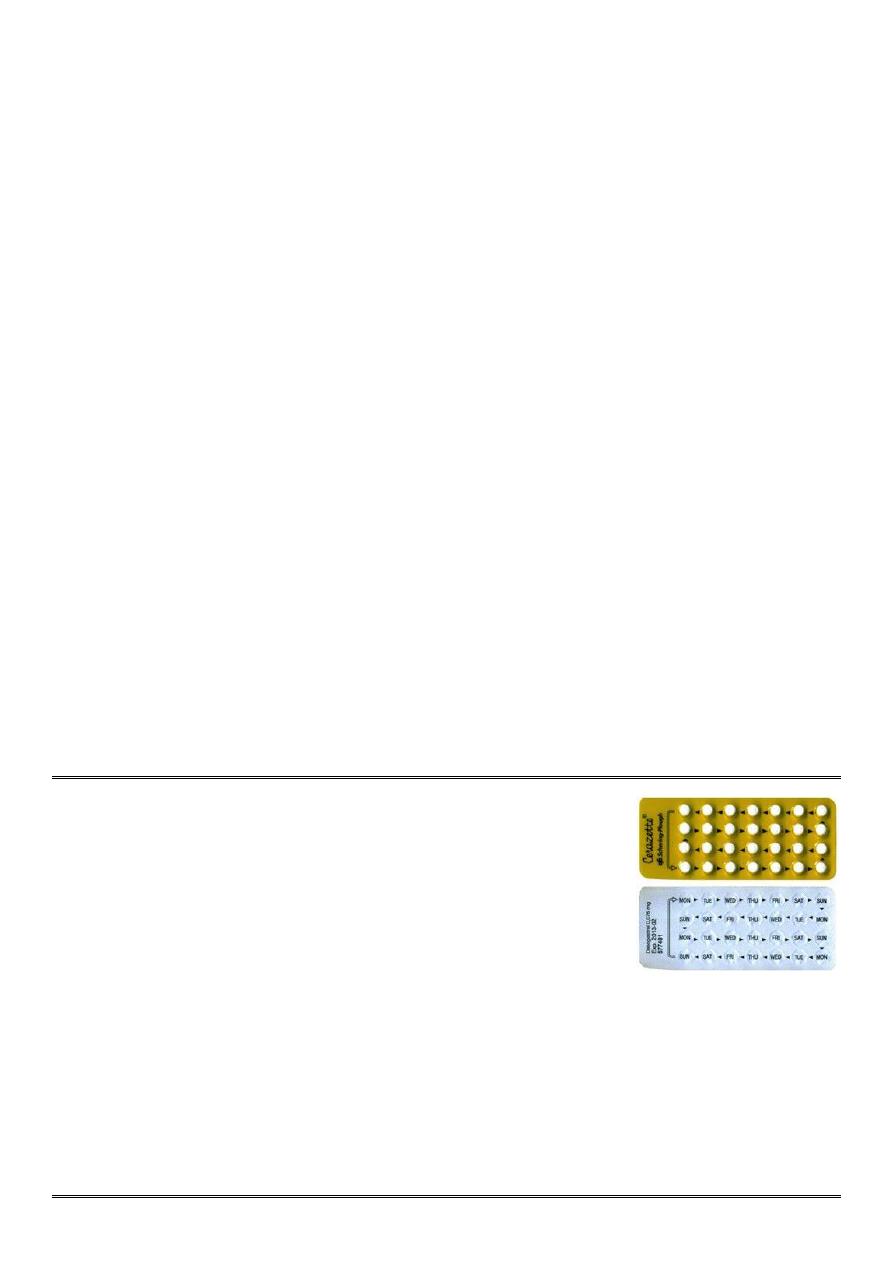
Answer 5 ==>
centrally inhibition of ovulation, Peripheral effects (Making endomtrium atrophic and hostile to an implanting embryo,
altering cervical mucus to prevent sperm ascending into the uterine cavity).
Answer 6 ==>
1-Absolute Contraindication => Circulatory diseases (IHD, CVA, HT, arterial or venous thrombosis), Acute or severe
liver disease, Oestrogen-dependent neoplasms (breast cancer), Breastfeeding <6 weeks post-
partum, Smoking ≥15
cigarettes/day and age ≥35, Focal migraine.
2-Relative contraindications => Generalized migraine, Long-term immobilization, Irregular vaglinal bleeding, Less
severe risk factors for cardiovascular disease (obesity, heavy smoking, diabetes).
Answer 7 ==>
Venous thromboembolism, Arterial disease (hypertention, myocardial infarction and thrombotic stroke), Mortality,
Carcinogenic effect (Breast cancer, Cervical cancer, Liver cancer), CNS (Depression, Headaches, Loss of libido),
Gastrointestinal, Genitourinary system, Chloasma, Leg cramps.
Answer 8 ==>
Less than 12 hours late (Don't worry. Just take the delayed pill at once, and further pills as usual), More than 12 hours
late (Take the most recently delayed pill now + Use extra precautions (condom, for instance) for the next 7 days(.
Answer 9 ==>
treat heavy or painful periods, improve premenstrual syndrome(PMS), reduce the risk of pelvic inflammatory
disease(PID), decreased incidence of benign breast lump, decrease number of functional ovarian cyst, *less
endometriosis, against both ovarian and endometrial cancers, treatment for acne.
Answer 10 ==>
parity, family history, menstrual history, any medical disease.
Answer 11 ==>
missing pills, low dose of active ingredient, irregular taking of pills or different time of administration, taking another
drug like ampicillin, gastroenteritis (defect in absorption).
Q1: What is this drug?
Q2: What are the mode of action?
Q3: What are the indications?
Q4: What are the side effects?
=========
Answer 1 ==> Progesterone only pills (mini-pills)
Answer 2 ==>
central effects (inhibit ovulation) peripheral effects (local effect on cervical mucus making it hostile to ascending
sperm, Local effect on the endometrium making it thin & atrophic thereby preventing implantation, cause decreased
tubal and endometrial motility).
Answer 3:
breastfeeding, older age, cardiovascular risk factors, diabetes.
Answer 4:
Menstrual disturbances, Functional ovarian cyst, ectopic pregnancy.

Q1: What is this drug?
Q2: What are the indications?
Q3: What are the side effects?
=================
Answer 1 ==> Injectable progestogens (Depo-Provera)
Answer 2 ==>
1-contraindication to estrogen
2-Following rubella vaccination in puerperium,
3-Husband waiting for effect of vasectomy
4-Mental retarded women
Answer 3 ==>
weight gain, delay in return of fertility, persistent menstrual irregularity, irregular vaginal bleeding or amenorrhea, risk
of osteoporosis.
Subdermal implants:
1-Implanon consists of a single silastic rod that is inserted subdermally
under local anaesthetic into the upper arm.
2-It releases the progestogen etonogestrel 25-70 Mg daily.
3-Norplant, which is withdrawn from the market It lasts for 3 years and
thereafter can be easily removed or a further implant inserted.
4-Implanon is particularly useful for women who have difficulty
remembering to take a pill and who want highly effective long-term
contraception.
5-There is a rapid return of fertility when it is removed.
6-It works for 1 year.
Q1: What is this instrument?
Q2: What is the mechanism of action?
Q3: What are the complications?
Q4: What are the contraindications?
==============
Answer 1 ==> Copper Intrauterine device
Answer 2 ==>
Induce inflammatory reaction within the endometrium, toxic to the sperm and oocyte and the embryo, interfere with the
fertilization, interfere with sperm motility and oocyte capability of fertilization and implantation.
Answer 3 ==>
1-Bleeding and pain
2-Infection(PID)
3-Perforation
4-Expulsion
5-Intrauterine pregnancy
6-Ectopic pregnancy.

Answer 4 ==>
1-Nulliparity and infertility
2-Active infection
3-Uterine anomalies increase risk of expulsion and perforation
4-gynecologic malignancy,
5-genital bleeding of unknown cause
6-gestational trophoblastic disease
Q1: What is this device?
Q2: What id the mechanism of action?
Q3: What are the side effects?
Q4: What are the characteristics of it?
Q5: What are the time of insertion?
=================
Answer 1 ==> Levonorgestrel releasing IUD "mirena"
Answer 2 ==>
Thickens cervical mucus, Inhibits sperm function in uterus, Reduces
monthly growth of the lining of the uterus, lessen menstrual blood loss in women who have heavy menstrual flow.
Answer 3 ==>
1- 10+ in every 100 women are likely to experience the following => Headache, Abdominal/ pelvic pain, Bleeding
changes, Vulvovaginitis, Genital discharge.
2- 1 to 10 in every 100 women are likely to experience the following => Depression, Migraine, Nausea, Acne,
Hirsutism, Back pain.
Answer 4 ==>
available, expensive, white color, larger, not metallic.
Answer 5 ==>
Time of insertion of both types of IUD > day 3-5 of the cycle because there is no pregnancy and the cervix is patulous
during this period.
Q1: What is this procedure?
Q2: How to check that the device is in the uterus?
Q3: What are the causes of thread not in place?
Q4: What are the complications at time of insertion?
Q5: How long this method is still?
=============
Answer 1 ==> Method of insertion of ICD
Answer 2 ==>
Thread in place, by US
Answer 3 ==>
expulsion, perforation in myometrium, thread is coiled in => so you can localize it by examination or US or abdominal
X-ray.
Answer 4 ==>
infection, pain, bleeding, trauma (perforation).
Answer 5 ==>
Copper still for 10 years, Merina still for 5 years
Bilateral tubal ligation:
1-Should ligate both uterine tubes.
2-Types => removal, clips, band, essure.
3-Essure => screw in the uterine tube lead to local inflammatory ration and block
the tube.
4-If the female want to become pregnant again =? do IVF.
Bilateral male vasiectomy:
1-Incision in the scrotum.
2-Cut the vas deferens.
3-The male become infertile after 3 months.
4-Should do semen analysis for at least 3 times to confirm the success of the operation.
Amsel's criteria:
for diagnosis of bacterial vaginosis in which at least three out of four should be present and these are:
1-Thin, gray, homogenous discharge.
2-Clue cell on microscope (vaginal epithelial cells so heavily coated with bacteria that the border is obscured).
3-PH of vagina> 4.5 (usually between 4.7-5.7).
4-
The addition of KOH to the vaginal secretions (the “whiff” test) releases a fishy, amine like odor.

Female presented with failure to get pregnant after 1-2 years with regular unprotected sexual activity,
Q1: What is your diagnosis?
Q2: What are the possible causes?
Q3: How you can manage her?
===========
Answer 1 ==> Infertility
Answer 2 ==>
1-Ovulatory factor (PCOS).
2-Tubal factor (Obstruction).
3-Endometrial factor.
4-Unexplained.
5-Testicular factor.
Answer 3 ==>
!- Take full history
2- Do physical examination
3- Do some investigations => Ultrasound, Hormonal assay, Laparoscope, Histosalpingography, In male seminal
analysis
4-Treatment:
•If there is ovulatory cause > stimulate the ovulation by clomiphene citrate > give it at day2 of the cycle and continue
for 5 days, start by low dose, follow up by US.
•If the cause is ovulatory > use pregnin > lead to LH surge, called
ابرة مفجرة
, lead to rapture of follicles, give it when
follicles are well-developed, its action begin after 48 hours.
•Life style modification > nutrition, weight, exercise.
