الدكتورة شيماء حازم الطيار
اختصاص نسائية و توليد وعقمبسم الله الرحمن الرحيم
السلام عليكم ورحمة الله
Ninevah university
Ninevah college of medicineObstetric &Gynecology department
Theoretical lectures
Lec (1)
Clinical anatomy of the female reproductive system
The anterior abdominal wall
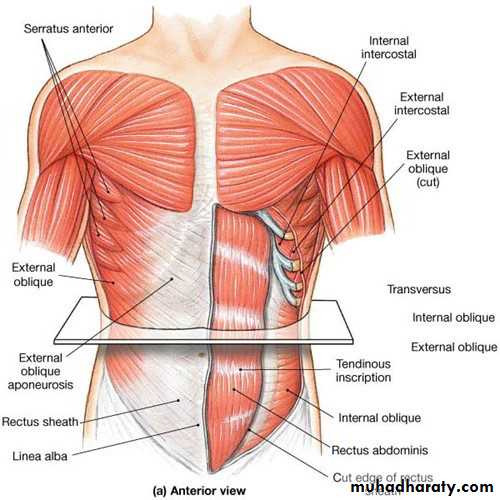
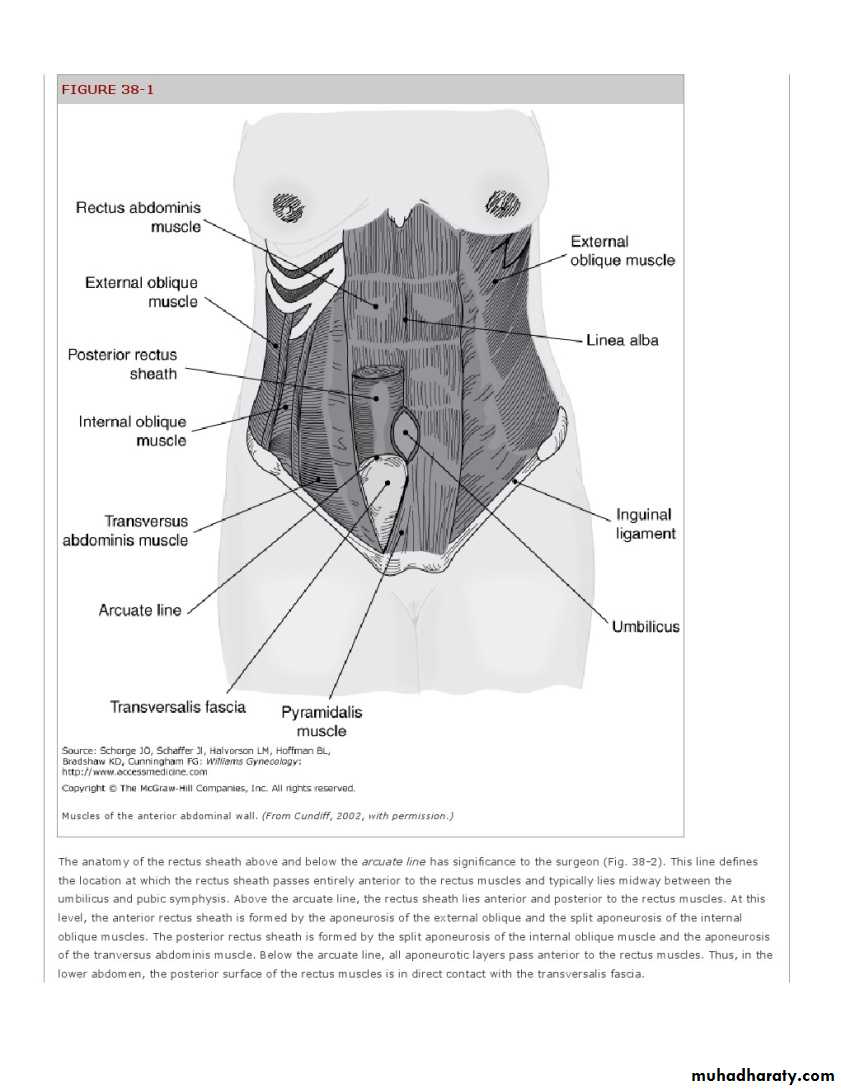
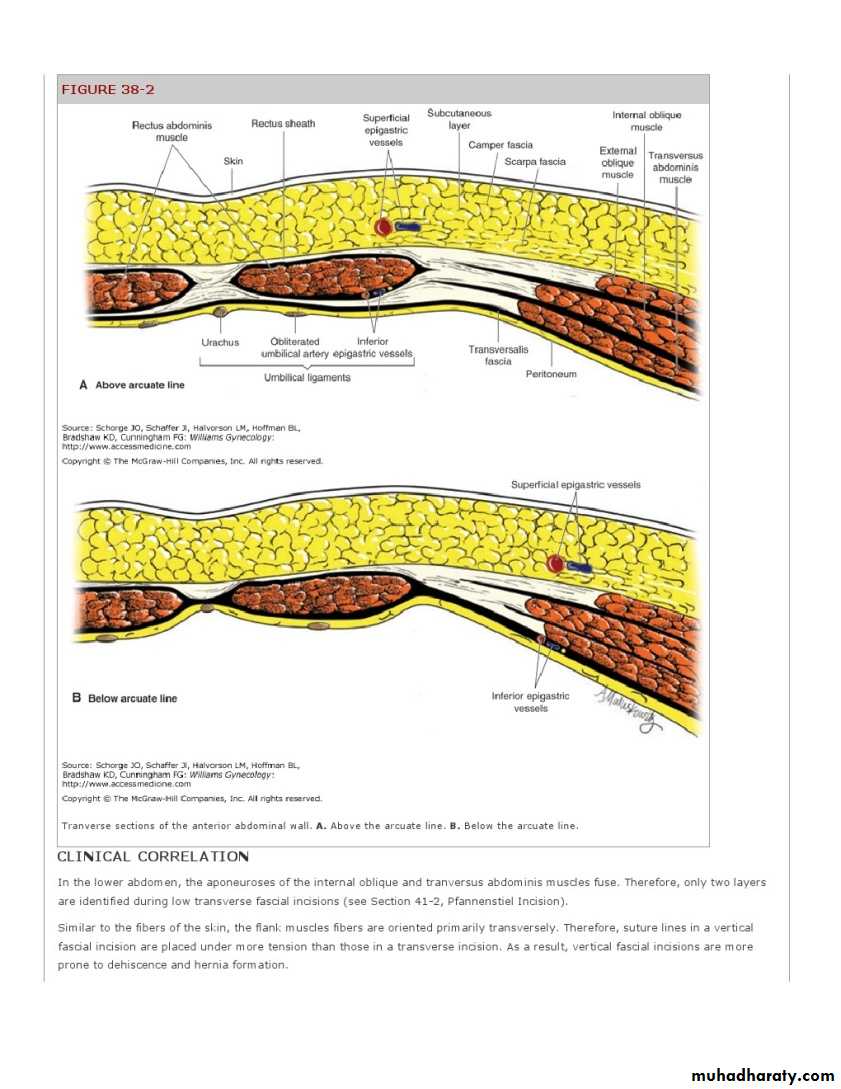
Beneath the skin and the fat of the superficial anterior abdominal wall lies a sheath and combination of musclesincluding the rectus abdominus, external and internal oblique and tranversalis muscle
The aponeuroses of the external & internal oblique, and tranversus abdominis muscles (flank muscles) conjoin to create the rectus sheath
Blood Supply
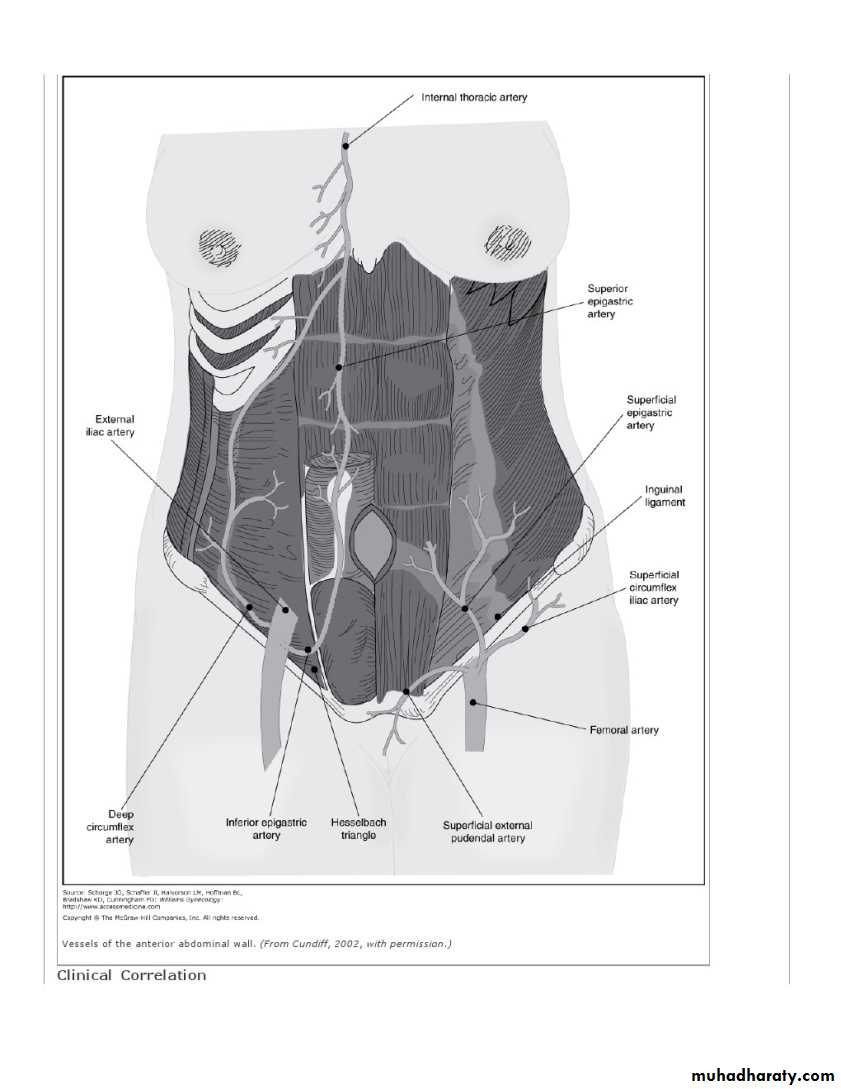
FEMORAL BRANCHESThe superficial epigastric, superficial circumflex iliac, and external pudendal arteries arise from the femoral artery just below the inguinal ligament in the region of the femoral triangle. These vessels supply the skin and subcutaneous layers of the anterior abdominal wall and mons pubis.
The superficial epigastric vessels course diagonally toward the umbilicus similar to the :-
inferior "deep" epigastric vessels , which are EXTERNAL ILIAC BRANCHES
Nerve Supply
• The iliohypogastric nerve provides sensation to the skin over the suprapubic area.• The ilioinguinal nerve supplies the skin of the lower abdominal wall and upper portion of the labia majora and medial portion of the thigh
Epithelium of the genital tract
The anterior abdominal wall including the vulva, vagina and perineal areas are lined with squamous epithelium.The epithelium lining the endocervix and uterine cavity is columnar and the squamocolumnar junction usually arises at the ectocervix in women of reproductive age.
This is an important site as it is the area from which cervical intraepithelial neoplasia (CIN) and eventually cervical malignancy arises.
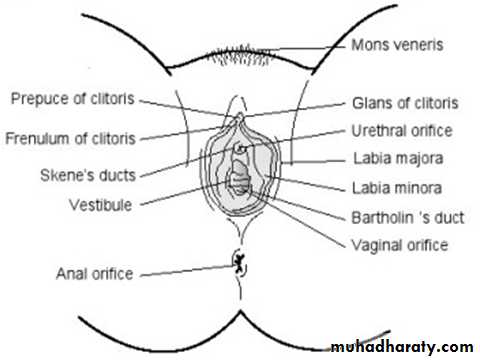
Vulva
Is the area of the perineum including the Mons pubis, labia majora and minora and the opening into both the vagina and urethra .the labia majora are areas of skin with underlying fat pads which bound the vagina. Medial to these are the labia minora. Anteriorly they come together to form the prepuce of the clitoris and posteriorly they form the forchette.
escutcheon
The hymenis a fold of vaginal mucosa at the entrance to this organ. It usually has a small opening in virgins and is only seen as an irregular remnant after marriage .
To each side of the introitus are the ducts of the vestibular glands commonly known as Bartholin’s glands
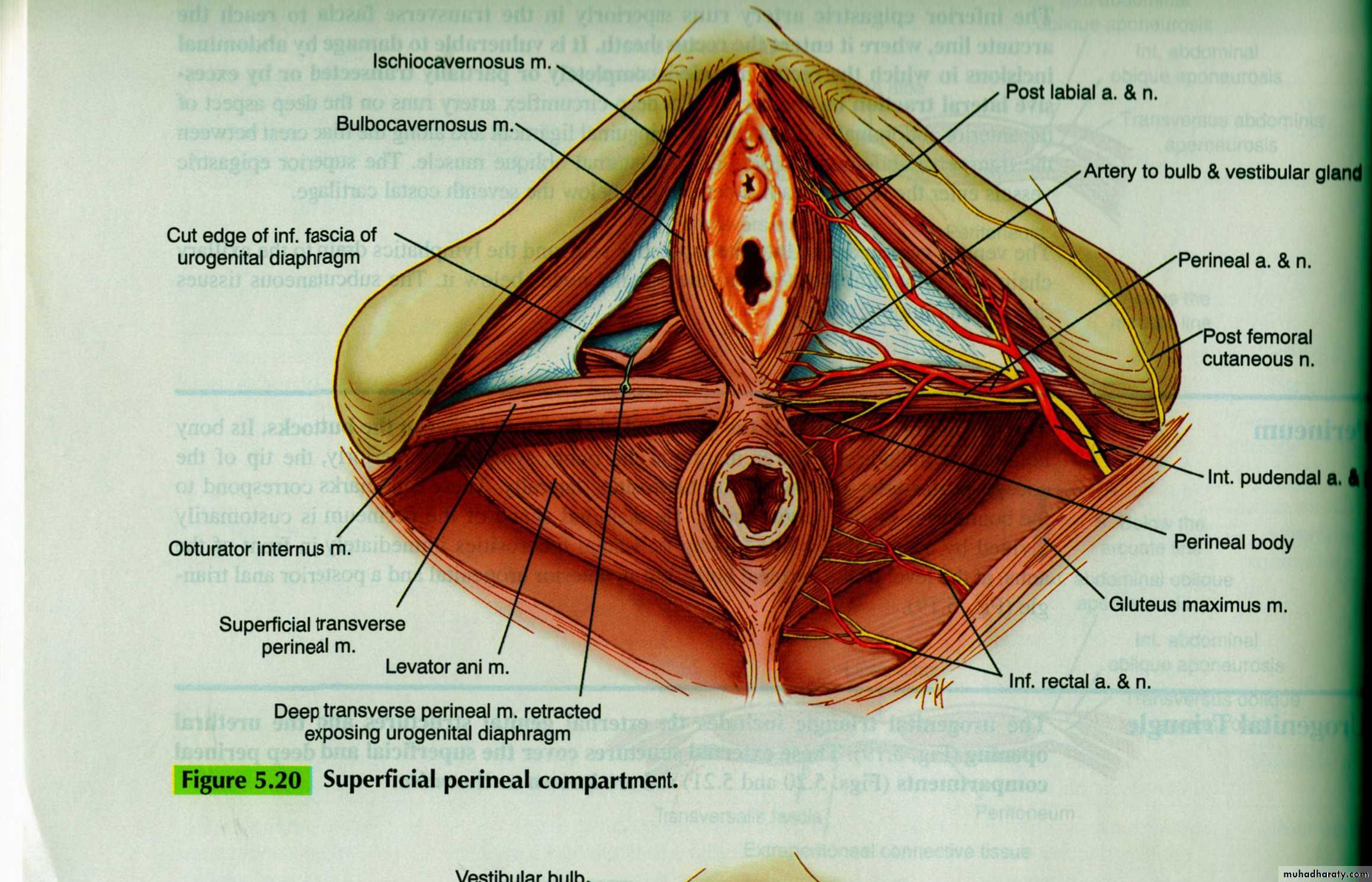
Perineum
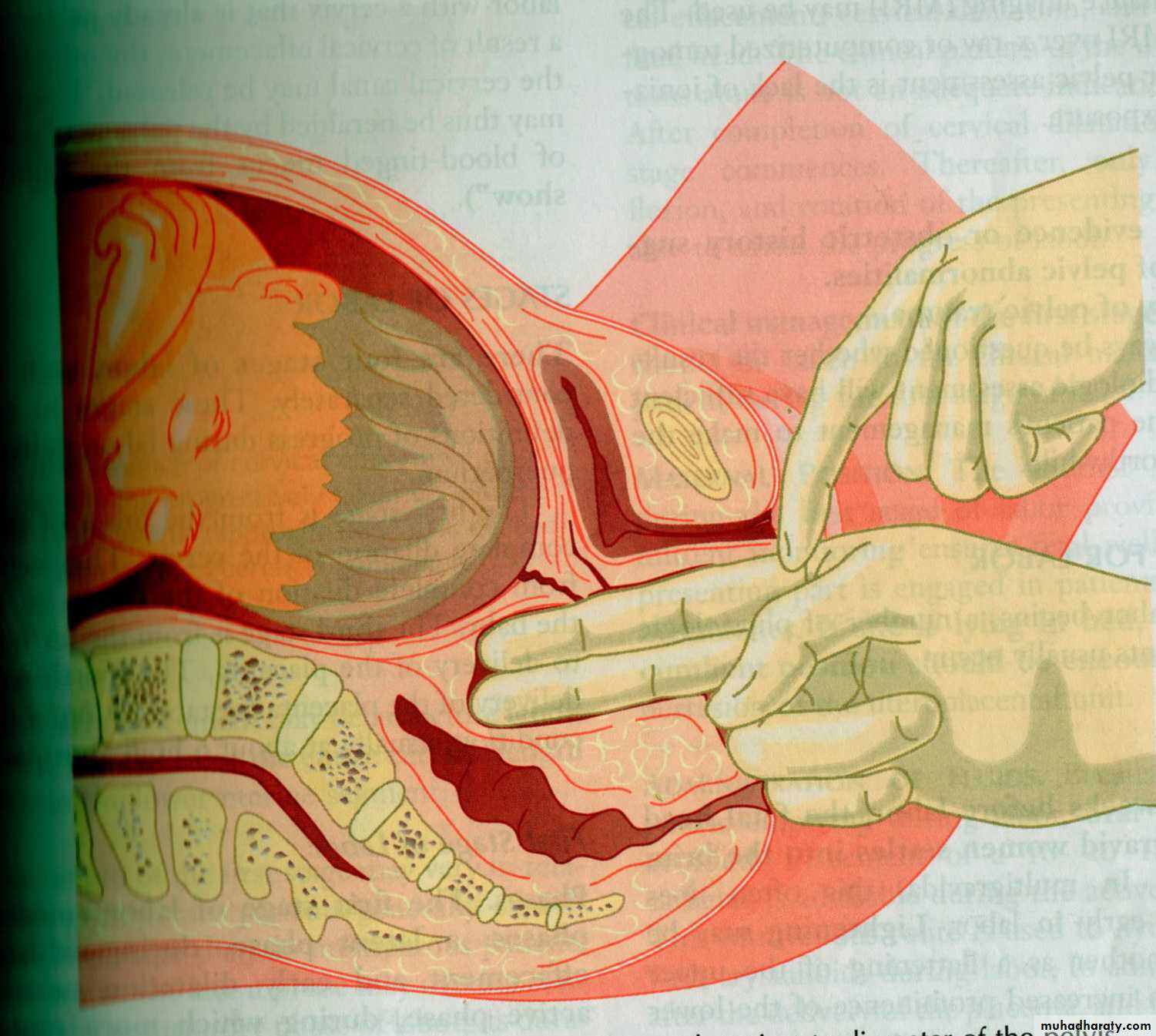
The area of the perineum is outlined by the vaginal fourchette anteriorly . Deep to it, is perineal body which lies between the anal canal and the lower one-third of the posterior vaginal wall .It is this area that is incised in the operation of episiotomy, where the introitus is enlarged to facilitate the birth of the baby or where lacerations can occur during labour
The vulval blood supply comes from the pudendal artery and
lymphatic drainage inguinal lymph N.nerve supply :
the pudendal nerve and
pelvic plexus with branches of the
Perineal nerves and
posterior cutaneous nerve of the thigh
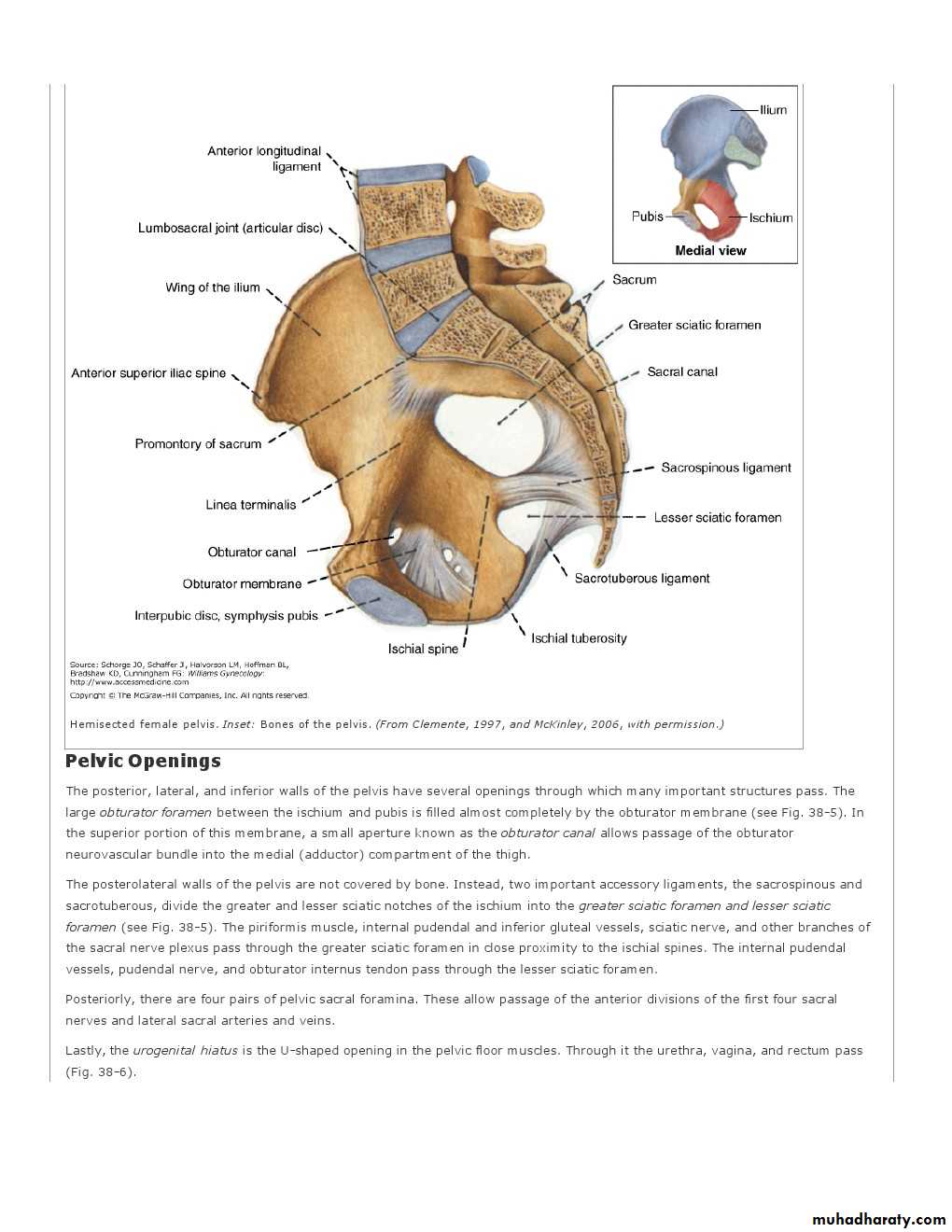
Bony Pelvis and Pelvic Joints
The bony pelvis is comprised of
(1) the two hip bones, termed the inominate bones;
(2) the sacrum; and
(3) the coccyx
The innominate bones consist of the ilium, ischium, and pubis, which fuse at the acetabulum, a cup-shaped structure that articulates with the femoral head. The ilium articulates with the sacrum posteriorly at the sacroiliac joint, and the pubic bones articulate with each other anteriorly at the symphysis pubis.
The sacroiliac joint is a synovial joint that connects the articular surfaces of the sacrum and ilium.
symphysis pubis is a cartilaginous joint that connects the articular surfaces of the pubic bones by way of a fibrocartilaginous disk.
The ischial spines are clinically important bony prominences
A plane drawn between the Sacral promontory and the superior aspect of the symphysis pubis marks the pelvic inlet and a similar plane drawn from the tip of S5 to the inferior aspect of the symphysis
pubis marks the pelvic outlet.
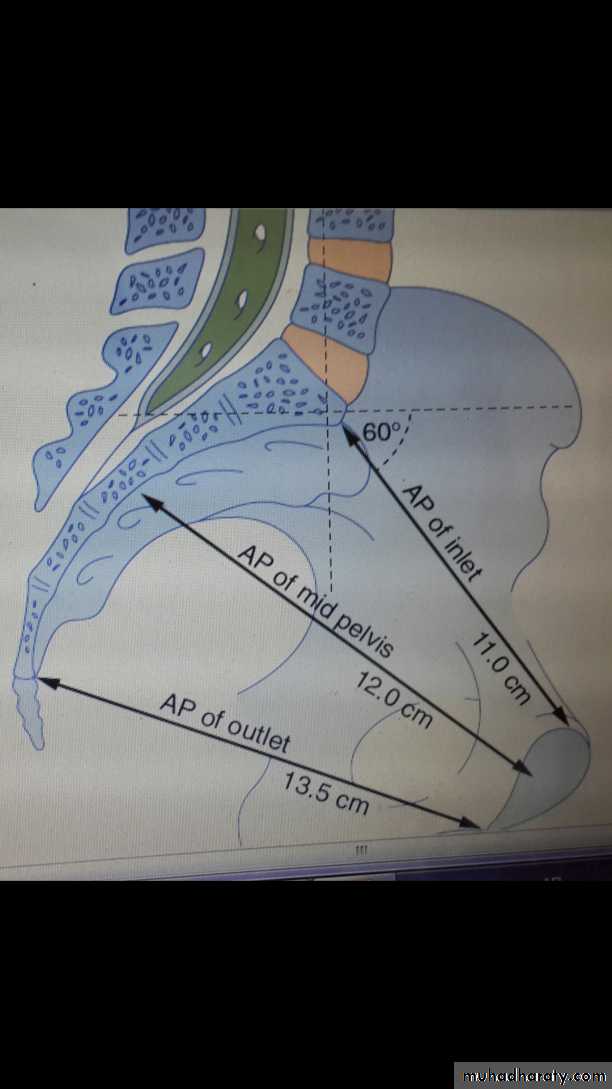
The pelvic brim or inlet
The pelvic brim is the inlet of the pelvis and isbounded in front by the symphysis pubis,
on each side by the upper margin of the pubic bone, the ileopectineal line and the ala of the sacrum, and posteriorly by the promontory of the sacrum.
transverse diameter in this plane is 13.5 cm and is
wider than the anterior–posterior (AP) diameter which is normally 11 cm
The pelvic mid-cavity
An area bounded infront by the middle of the symphysis pubis, laterally by the pubic bones, the obturator fascia and the inner aspect of the ischial bone and spines, and
posteriorly by the junction of the second and third sections of the sacrum.
The midpelvis is almost round, as the transverse and anterior diameters are similar at 12 cm. The ischial spines are palpable vaginally
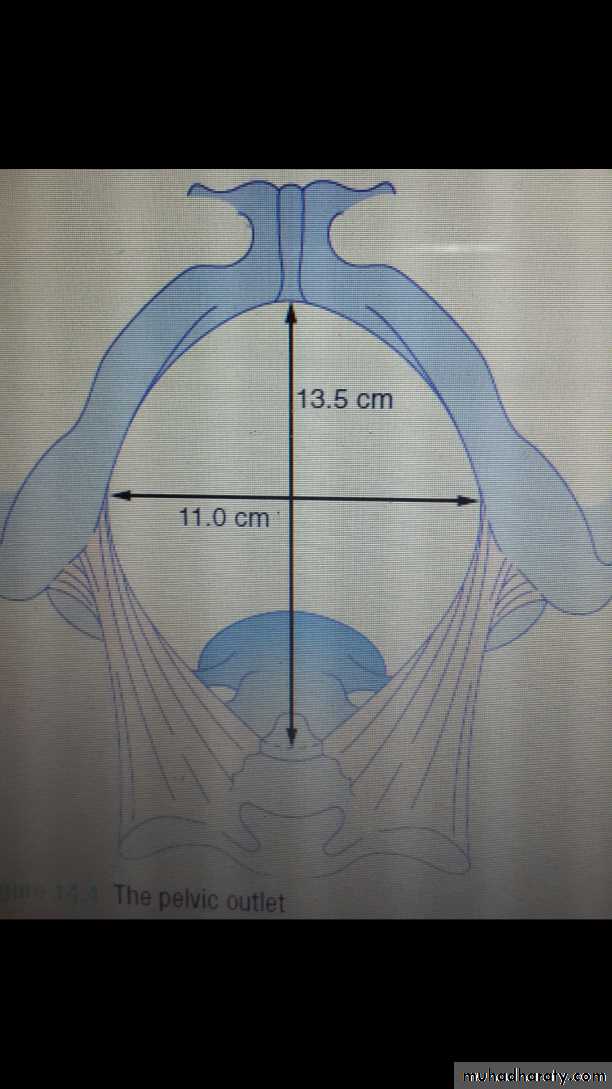
The pelvic outlet
The pelvic outlet is bounded
anteriorly by the lower margin of the symphysis pubis,
laterally by the descending ramus of the pubic bone, the ischial tuberosity and the sacrotuberous ligament, and
posteriorly by the last piece of the sacrum.
The AP diameter of the pelvic outlet is 13.5 cm and the transverse diameter is 11cm
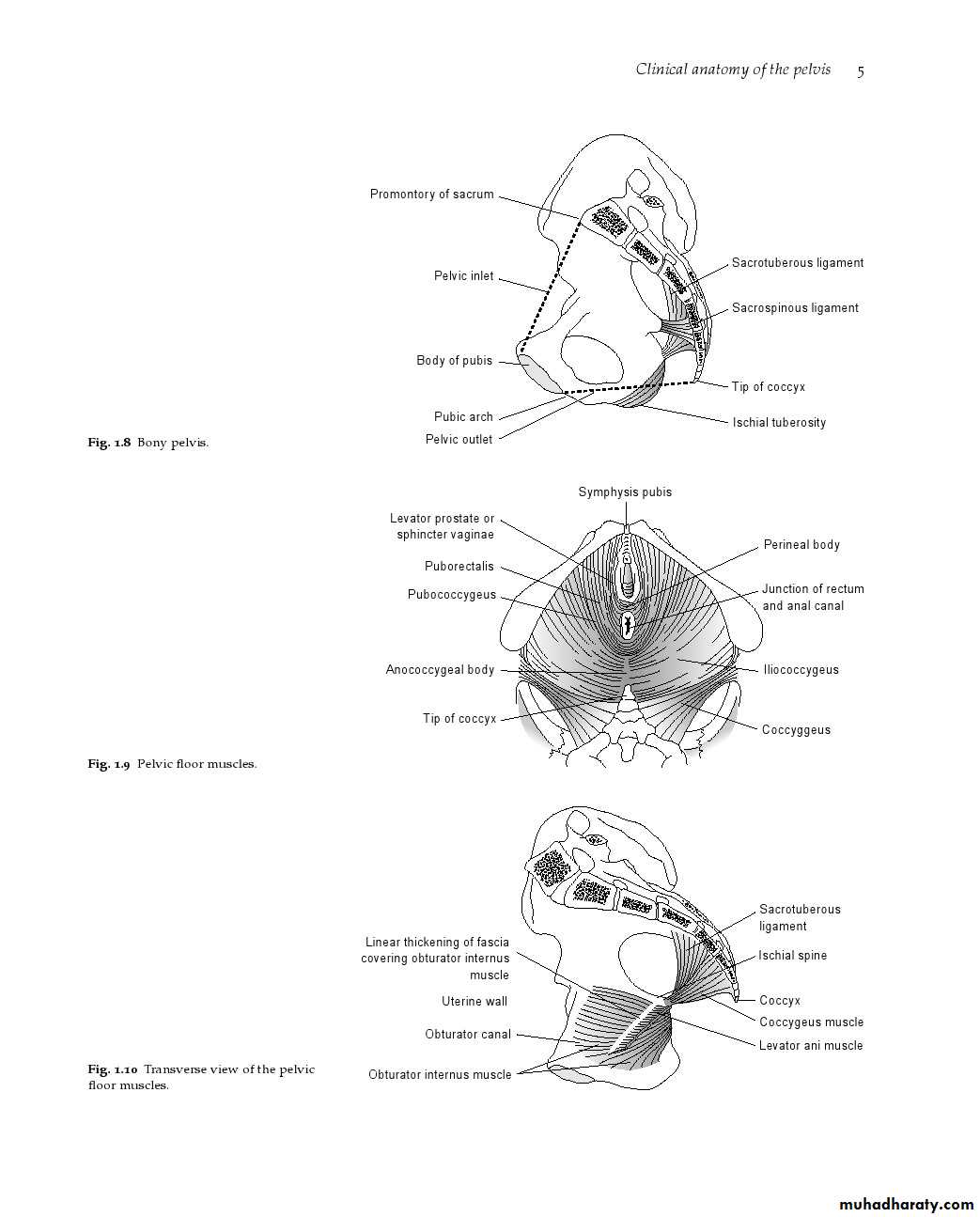
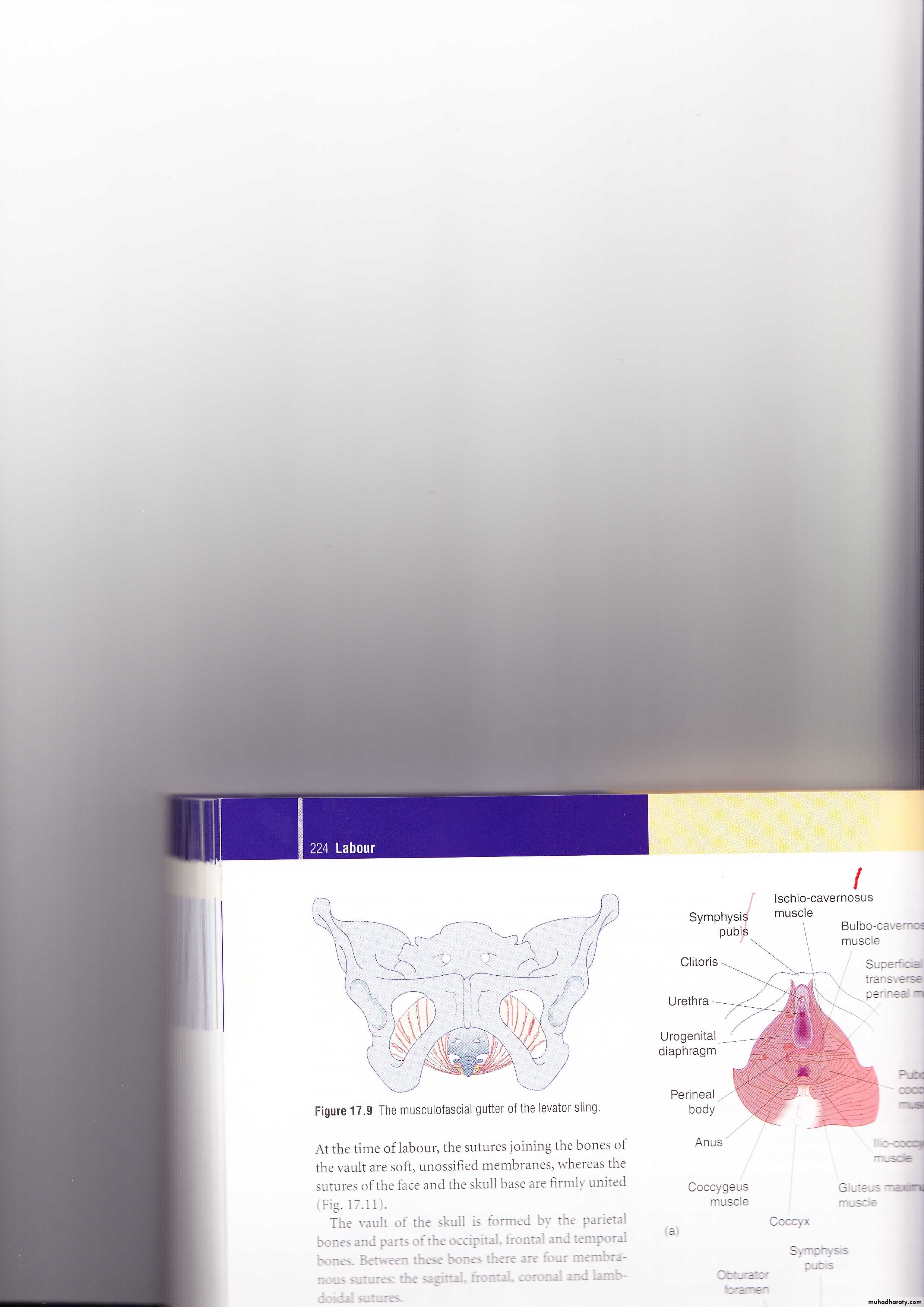
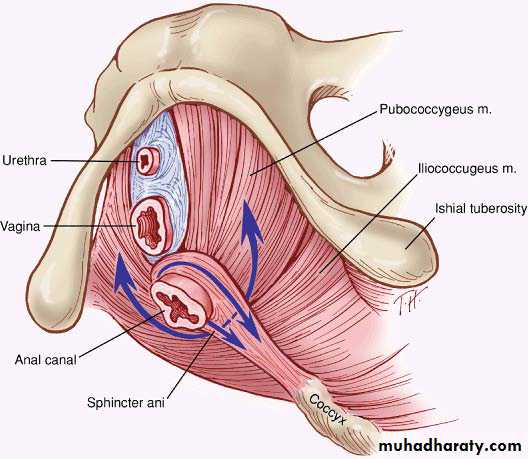
Pelvic floor
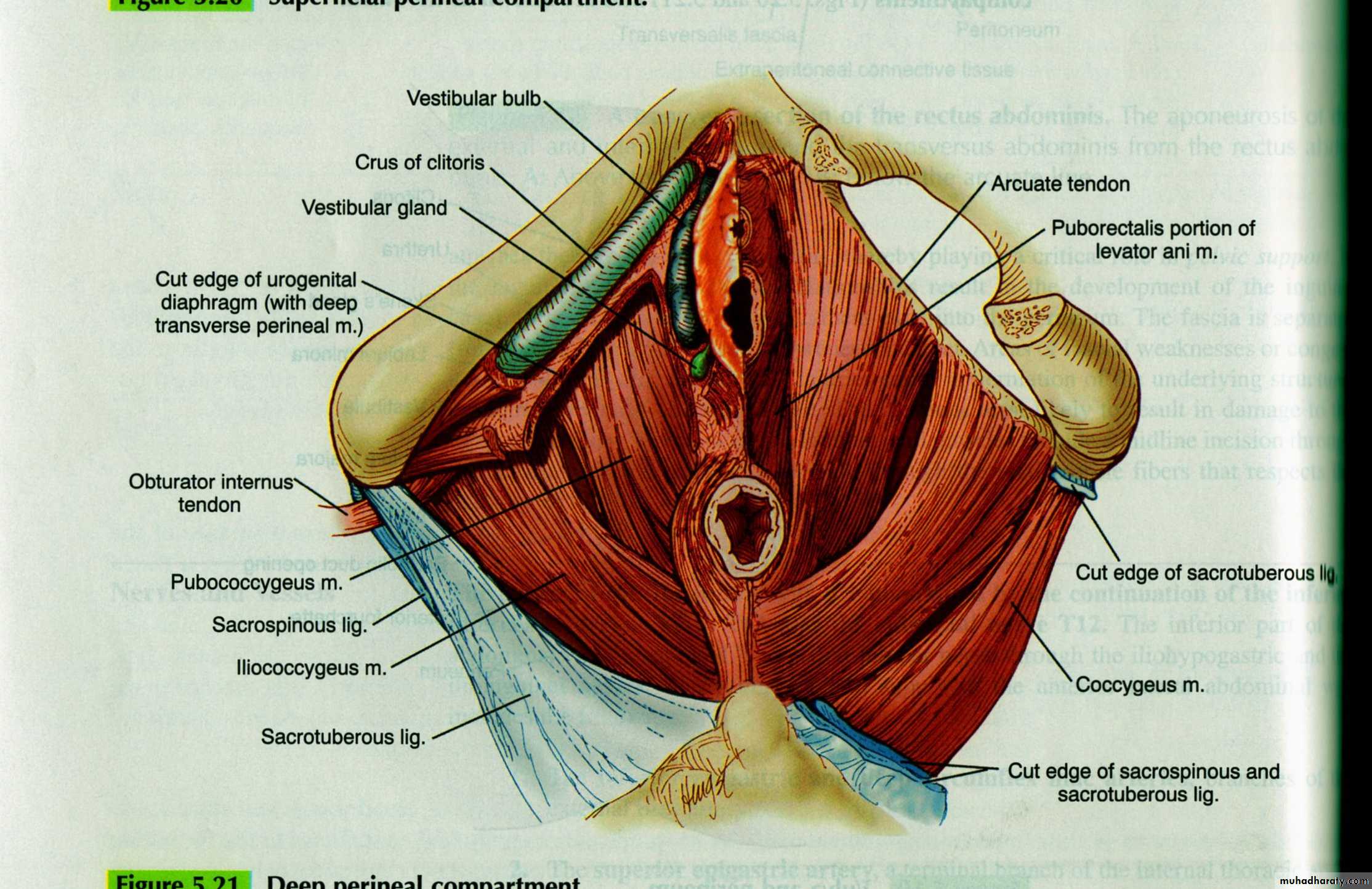
pelvic floor itself is a sling of various muscles which are pierced by the urethra, the vagina and the anal canal .LEVATOR ANI MUSCLES
This is the most important muscle in the pelvic floor and represents a critical component of pelvic organ support .Physiologically, normal levator ani muscles maintain a constant state of contraction. They provide a solid floor that supports the weight of the abdominopelvic contents against intra-abdominal forces.
The levator ani muscle is a complex unit that consists of several muscle components with different origins and insertions and therefore different functions.
The most important parts are : pubococcygeus, puborectalis, and iliococcygeus
The urogenital diaphragm
This is a triangular-shaped diaphragm through it pass the urethra and vagina.0n its deep aspect are 2sets of muscles the constrictor of the urethra and vagina,& the deep transverse perinei.Superficially,there are the ischiocavernosus muscle ,the bulb (erectile tissue) with the bulbocavernosus muscle, the superficial perineal muscle,& bartholin glands.
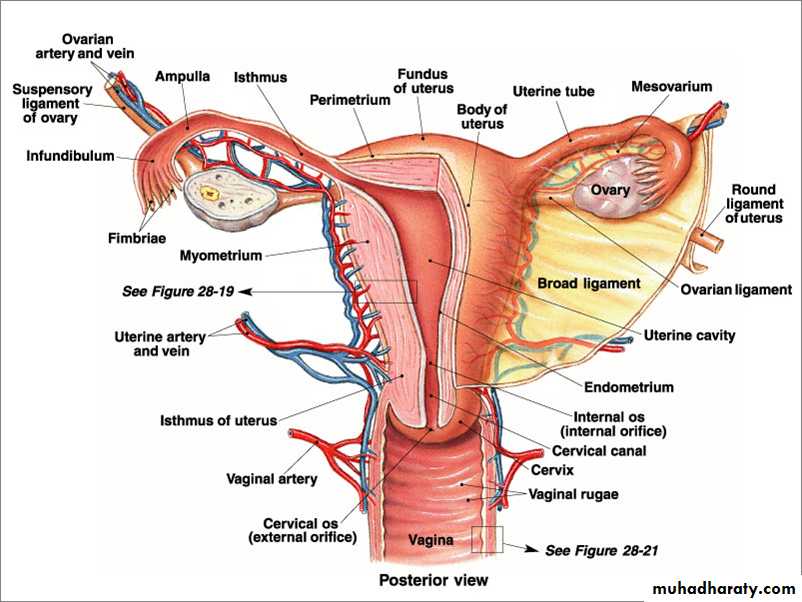
Pelvic VisceraUTERUS
The uterus is a fibromuscular hollow organ situated between the bladder and the rectum. The uterus is divided structurally andfunctionally into two portions: an upper muscular body, the corpus , and a lower fibrous cervix
The portion of the corpus that extends above the level of entry of the fallopian tubes into the endometrial cavity is known as the fundus
rugae
The shape, weight, and dimensions of the uterus vary according to parity and estrogen stimulation. Before menarche and after menopause, the corpus and cervix are approximately equal in size, but during the reproductive years, the uterine corpus issignificantly larger.
In the adult, non pregnant woman, the uterus measures approximately 7 cm in length and 5 cm in width at the fundus and weighs 30 to 50 g.
Endometrium and Serosa
The uterus consists of an inner layer of mucosa called the endometrium that surrounds the endometrial cavity and a thick muscular wall known as the myometrium. The endometrium consists of columnar epithelium and specialized stroma.The superficial portion of the endometrium undergoes cyclic changes with the menstrual cycle The spiral arterioles located in the endometrium undergo hormonally mediated constriction or spasms that cause shedding of the superficial portion of this layer with each menstrual cycle.
serosa
Peritoneal serosa overlays the outer wall except for the anterior portion of the cervix, which is covered by the bladder, and for the lateral portions of the corpus and cervix that attach to ligamentsFallopian Tubes
The fallopian tubes are tubular structures that measure 7 to 12 cm in length. Each tube has four identifiable portions.1)The interstitial portion passes through the body of the uterus at the region known as the cornua.
13)The isthmic portion begins adjacent to the uterine corpus. It consists of a narrow lumen and a thick muscular wall.
3)The ampullary portion is recognized when the lumen widens. In addition to a wider lumen, this segment has a more convoluted mucosa.
Fallopian tubes
4)The fimbriated portion is the distal continuation of the ampullary segment. The fimbriated end has many frond-like projections thatprovide a wide surface area for ovum pickup. The fimbria ovarica is the projection that is in contact with the ovary.
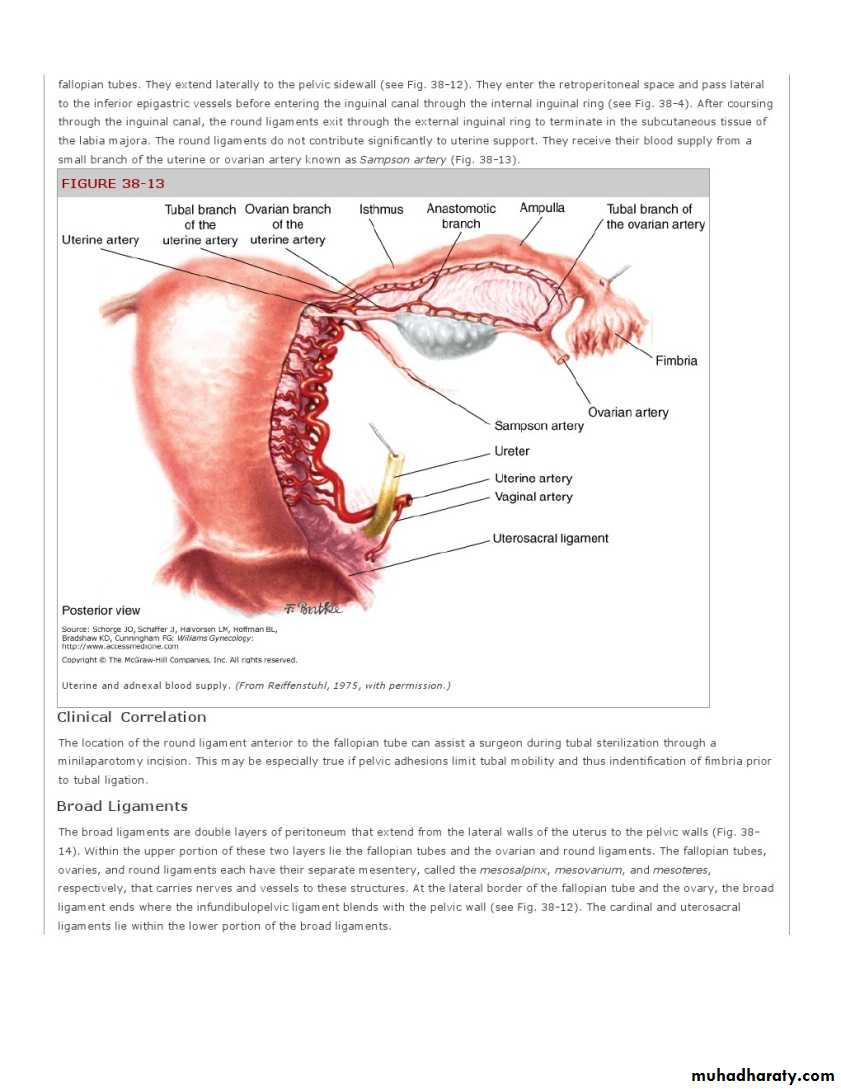
The ovarian artery runs along the hilum of the ovary and sends several branches through the mesosalpinx to supply the fallopian tubes.
The venous plexus, lymphatic drainage, and nerve supply of the fallopian tubes follow a similar course to
that of the ovaries.
Cervix
The uterine cervix begins caudal to the uterine isthmus and is approximately 2 cm in length. The wall of the cervix consists primarily of fibrous tissue and a smaller amount (approximately 10 percent) of smooth muscle.
The endocervical canal is lined by columnar, mucus-secreting epithelium.
The transformation zone
The lower border of the canal, called the external cervical os, contains a transition from squamous to columnar epithelium of the cervical canal .. At the upper border of the endocervical canal is the internal cervical os, where the narrow cervical canal becomes continuous with the wider endometrial cavity.
Uterine Lymphatic Drainage
Lymphatic drainage of the uterus is primarily to the obturator and internal and external iliac nodessuperficial inguinal nodes
lateral sacral nodes.
are smooth muscle extensions of the uterine corpus
and arise from the lateral aspect of the corpusjust below and anterior to the origin of the fallopian tubes
Round ligament
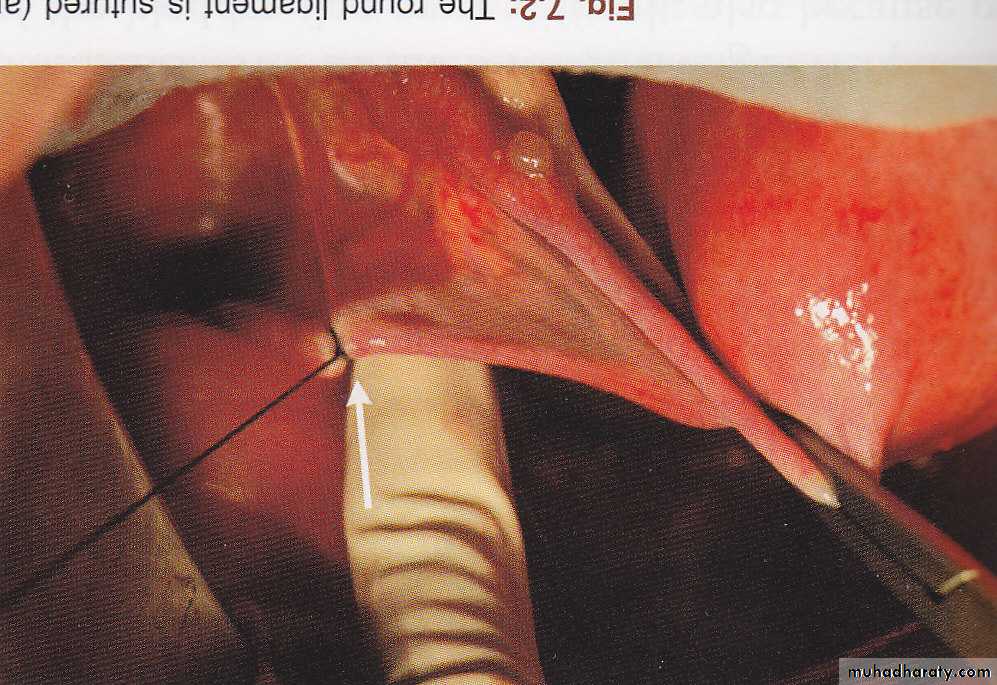
Round Ligaments
They extend laterally to the pelvic sidewall. They enter the retroperitoneal space and enter the inguinal canal through the internal inguinal ring. After coursing through the inguinal canal, the round ligaments exit through the subcutaneous tissue of the labia majora.
The round ligaments do not contribute significantly to uterine support.
Broad Ligaments
The broad ligaments are double layers of peritoneum that extend from the lateral walls of the uterus to the pelvic walls .Within the upper portion of these two layers lie the fallopian tubes and the ovarian and round ligaments.
The fallopian tubes, ovaries, and round ligaments each have their separate mesentery, called the mesosalpinx, mesovarium, and mesoteres,respectively, that carries nerves and vessels to these structures.
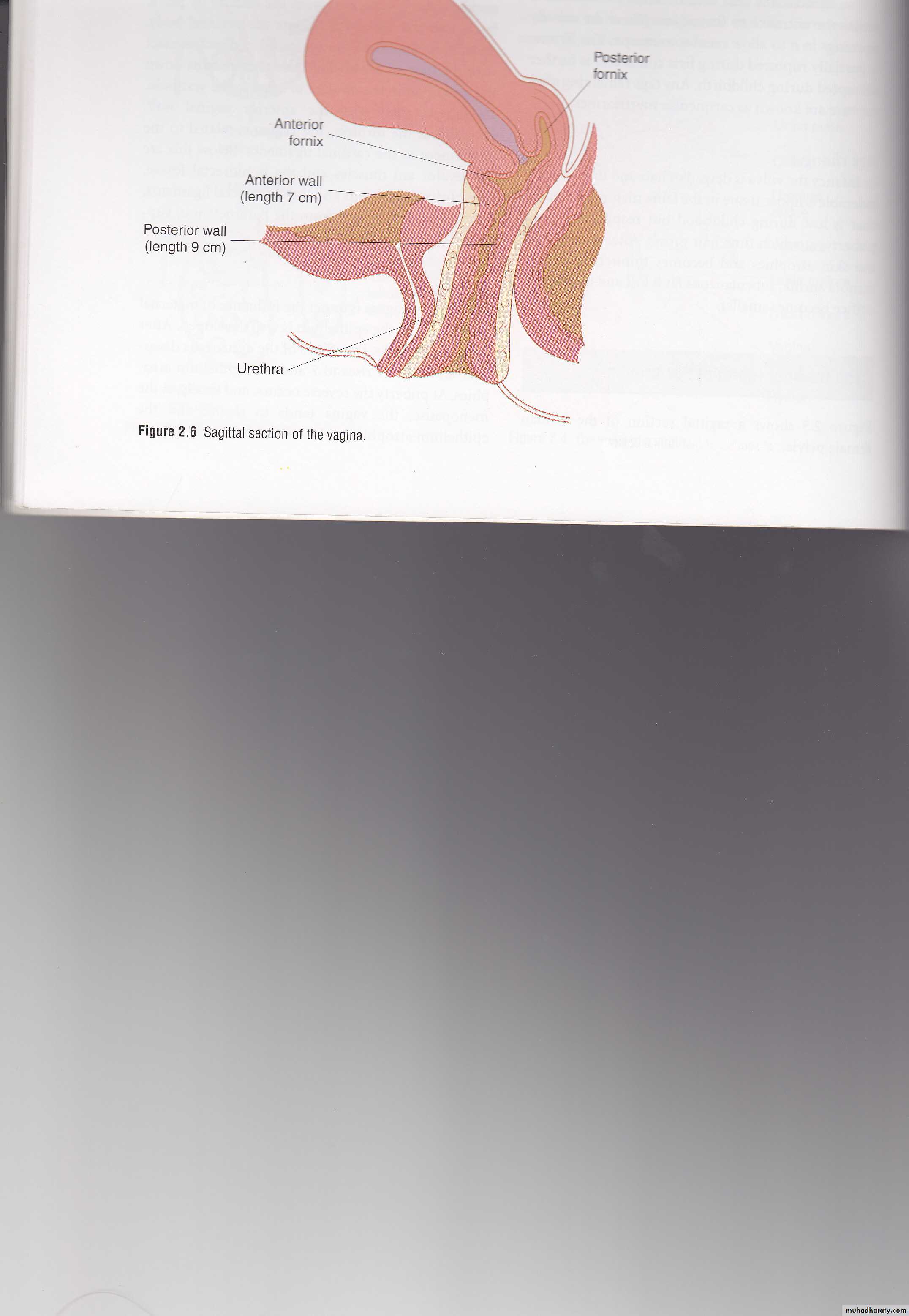
Vagina
is a distensible muscular 8-12 cm tube passes from the introitus to the cervix.anteriorly, is related to the base of the bladder and the urethra, and posteriorly, to the pouch of Douglas, rectum and anal canal . the uterine cervix project into the top of the vagina deviding it into 4 fornices and are labelled as anterior,posterior, right or left
The epithelium contains no glands but is rich in glycogen in the premenopausal woman. The normal commensal, Doderleins bacillus, breaks down this glycogen to create an acid environment
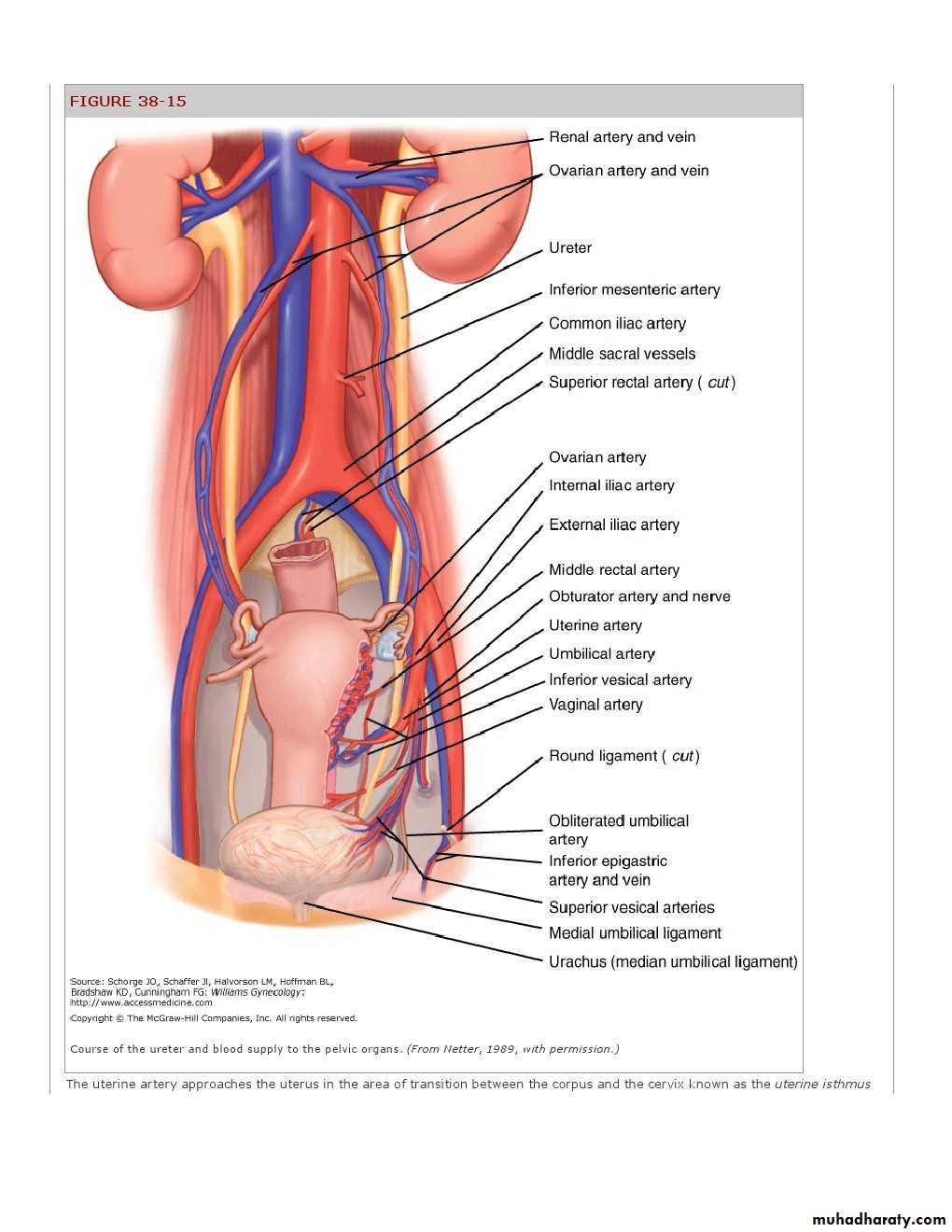
Blood supply of the vagina
vaginal arteries which arise from the internal iliac arteriesuterine arteriers (descending branches)
aided by the arteries to the bladder above ,
middle rectal &
internal pudendal arteries.
There is a profuse network of veins accompanying the arteries.
The ovaries
The ovaries and fallopian tubes constitute the uterine adnexa . The size and hormonal activity of the ovaries depend on age, time of the menstrual cycle, and exogenous hormonal suppression. During reproductive years, the ovaries measure
2.5 to 5 cm in length,
1.5 to 3 cm in thickness, and
0.7 to 1.5 cm in width.
Ovaries
consist of an outer cortex and an inner medulla. Ovarian cortex is comprised of a specialized stroma punctuated with follicles, corpora lutea, and corpora albicantia.A single layer of mesothelial cells covers this cortex as a surface epithelium( the germinal epithel ium)
The medullary portion of the ovary consists primarily of fibromuscular tissue and blood vessels.
Ovaries
are attached to the posterior leaf of the broad ligament by the mesovarium.In addition they are fixed in position by the ovarian ligament (to the uterus medially) and the infundibulopelvic ligament which contains the ovarian blood supply direct from the aorta.
Laterally, each ovary is attached to the pelvic wall by an infundibulopelvic ligament , also termed suspensory ligament of the ovary, that contains the ovarian vessels and nerves
Ovarian Blood Supply, Lymphatics, and Innervation
The blood supply to the ovaries comes from the ovarian arteries, which arise from the and from the ovarian branches of the uterine arteriesThe right ovarian vein drains into the inferior vena cava.
However, the left ovarian vein drains into the left renal vein.
Lymphatic drainage to the para-aortic nodes .
Innervation to the ovaries are supplied by extensions of the renal plexus that course along the ovarian vessels in the infundibulopelvic ligament.
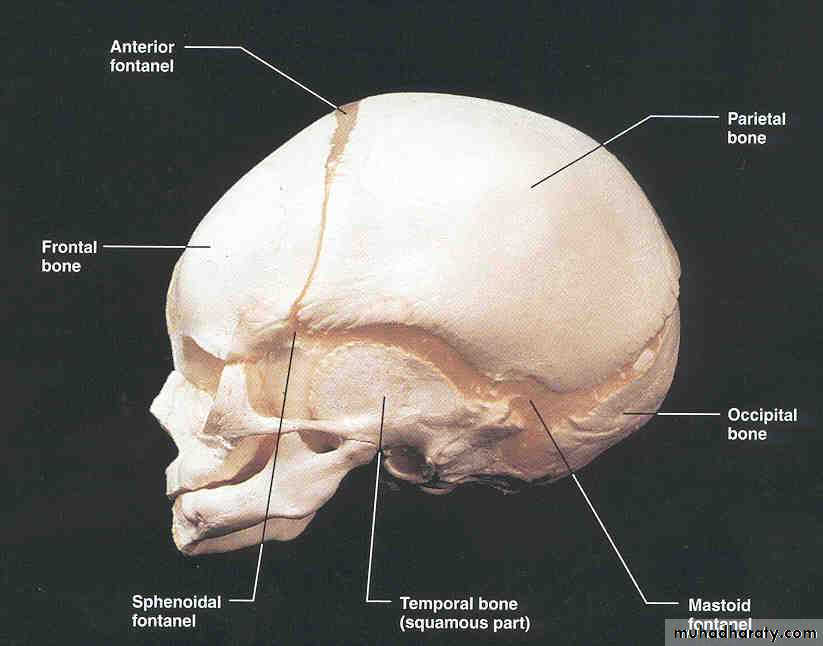
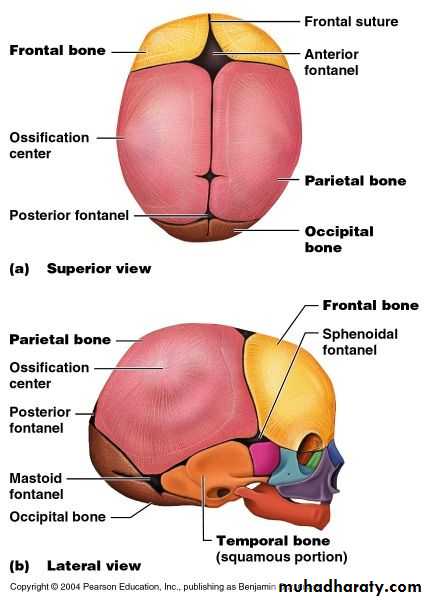
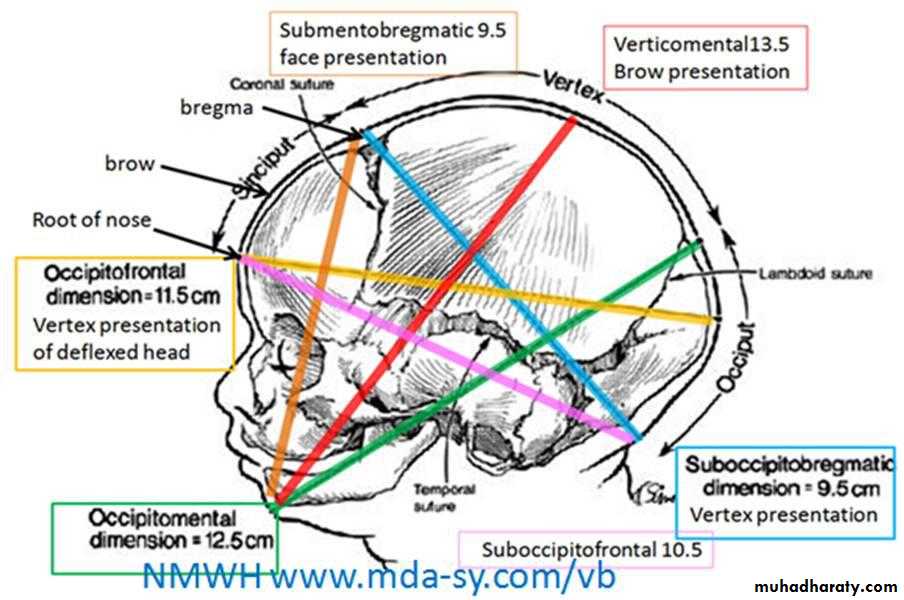
Fetal skull
Fetal skull
Is made up of the vault, the face & the base.The sutures are the lines formed where the individual bony plates of the skull meet one another.
At the time of labour, the sutures joining the bones of the vault are soft , unossified ,whereas that of the face and base are firmly united.
The fontanelles are the junctions of the various sutures
LANDMARKS
The bones form the vault are the parietal ,parts of the occipital,frontal &temporal bones.3sutures are of obstetric importance:
Sagittal suture:between the superior borders of parietal bones
Frontal suture:is the forward continuation of sagittal suture lies between the2 parts of frontal bones.
Coronal suture:between the anterior border of parietal &posterior border of frontal bones
LAMBDOIDAL SUTURE between the occipital bone behind and the parietal and temporal bones in front
TEMPORAL SUTURE between the temporal and the parietal bones
ANTERIOR FONTANELLE or BREGMA is the large diamond-shape depression at the anterior end of the cranium where frontal ,coronal &sagittal suturesmeet
POSTERIOR FONTANELL is the smaller triangular space at the posterior end of the cranium where sagital& lambdoid sutures meet.
Areas of skull
Vertex:-top of the skull,between the anterior &posterior fontanelles and the2 prietal eminenceSinciput:-the part of the head in front of the anterior fontanell .It is subdevided into the brow and the face
Occiput:-the back of he head,lies behind the posterior fontanelle.