Pediatrics
NEUROLOGY
1
L.3 Dr.Roua Al yaseen
Febrile Seizures
Definition:
Febrile seizures are seizures that occur between the age of 6 and 60 mo with
a temperature of 38°C (100.4°F) or higher, that are not the result of central nervous
system infection or any metabolic imbalance, and that occur in the absence of
a history of prior afebrile seizures.
There are several identified genetic mutations that contribute for FS & manifested
by positive family hx of FS. Although most FS are polygenic, in many families the
disorder is inherited as AD trait.
Simple febrile seizure is a primary generalized, usually tonic–clonic,
attack associated with fever, lasting for a maximum of 15 min, and not
recurrent within a 24-hr period,
child return to normal after the attack.
A complex febrile seizure is more prolonged (>15 min), is focal, and/or reoccurs
within 24 hr.
30–50% of children have recurrent febrile seizures
Risk factors that can predict RECURRENCE of FS including:-
Major criteria;
o
age <1 yr,
o
fever 38-390C,
o
fever duration <24 hr (i.e. an infant with simple & short duration of
fever).
Minor criteria;
o
family hx of FS or epilepsy
o
complex FS
o
male
o
day care
o
hyponatremia.
Having no risk factors carries a recurrence risk of approximately 12%; 1 risk
factor, 25-50%; 2 risk factors, 50-59%; 3 or more risk factors, 73-100%.
Pediatrics
NEUROLOGY
2
Risk factors for subsequent EPILEPSY including:-
Simple FS (1%),
Recurrent FS (4%),
Complex FS (6%),
Fever <1 hr before FS (11%),
Family hx of epilepsy (18%),
Focal complex FS (29%),
Neurodevelopmental abnormalities (33%).
Approach to patient with febrile seizure:-
The most important thing is to determine the cause of the fever and exclude CNS
infection(meningitis or encephalitis).
If any doubt exists about the possibility of meningitis ( especially if seizures are
complex or the child remains drawzy after a short postictal period). a lumbar
puncture with examination of the cerebrospinal fluid (CSF) is indicated.
Note: CSF exam by LP should be done in any infant less than 12 mo with FS
because seizure may be the only manifestation of meningitis, especially if patient
had received antibiotics which mask the other features of meningitis.
*other laboratory testing such as serum electrolytes, blood glucose& toxicology
screening can be done if need.
*EEG is not needed after simple febrile convulsion but may be usefull with
complex seizure.
Note: Early EEG after FS usually do not predict the future recurrence of FS or later
epilepsy even if the result is abnormal, thus it should be deferred for at least 2 wk
after FS.
*Neuroimaging(CT scan,MRI) may need for children with focal neurologic signs
or had risk factors for later epilepsy e.g. neurodevelopmental abnormalities or
family hx of epilepsy as well as febrile status epilepticus .
Pediatrics
NEUROLOGY
3
Treatment.
o Give short acting anticonvulsant therapy (diazepam) to control convulsion
o In case of febrile status epilepticus, IV benzodiazepines, phenobarbital,
phenytoin, or valproate may be needed .
o Antipyretics & cold sponge to control fever
o Treat the underlying cause of fever like viral URT infection, roseola, acute
otitis media which are most frequently the cause of febrile convulsion.
o if patient has risk factors for recurrences, parents should be educated about
how to handle the seizure if it recur & last >5 min by use oral, rectal diazepam
or buccal/intranasal midazolam as prophylactic.
o Iron deficiency has been associated with ↑ risk of FS, and thus screening &
Treatment for it appears appropriate.
Prevention: If the parents are very anxious about their child's seizure,
intermittent oral diazepam 0.3 mg/kg or rectal suppository 0.5 mg/kg every 8
hrs. for 2-3 days can be given during febrile illnesses to prevent recurrence of FS.
Other phenobarbital can be used.
Prognosis: Excellent, not associated with reduction in later intellectual
performance. The incidence of epilepsy later on is 1% in children with no risk
factors, while incidence increase according to risk factors that previously
mentions.
Pediatrics
NEUROLOGY
4
CEREBRAL PALSY
CP is a diagnostic term used to describe a group of motor syndromes resulting
from disorders of early brain development. Although it was considered static, it
often change or progress over time.
It is the most common form of chronic motor disability, commonly associated with
developmental disabilities, including mental retardation, epilepsy, and visual,
hearing, speech, cognitive, and behavioral abnormalities.
Causes
1-Antenatal factors (In 80% of cases)
include:
*Cerebral malformations.
*intrauterine infection(TORCH).
*placental insufficiency.
*chromosomal anomalies & genetics.
*intrauterine exposure to maternal infection. (chorioamnionitis, inflammation of
placental membranes).
2-Perinatal factors:
*birth asphyxia.
*prematurity & low birthweight infants particularly those weighing >1,000 g at
birth because the risk of intraventricular hemorrhage
3-postnatal factors:
kernicterus, CNS infections, metabolic (hypoglycemia),CVA,
& trauma.
Clinical Manifestations
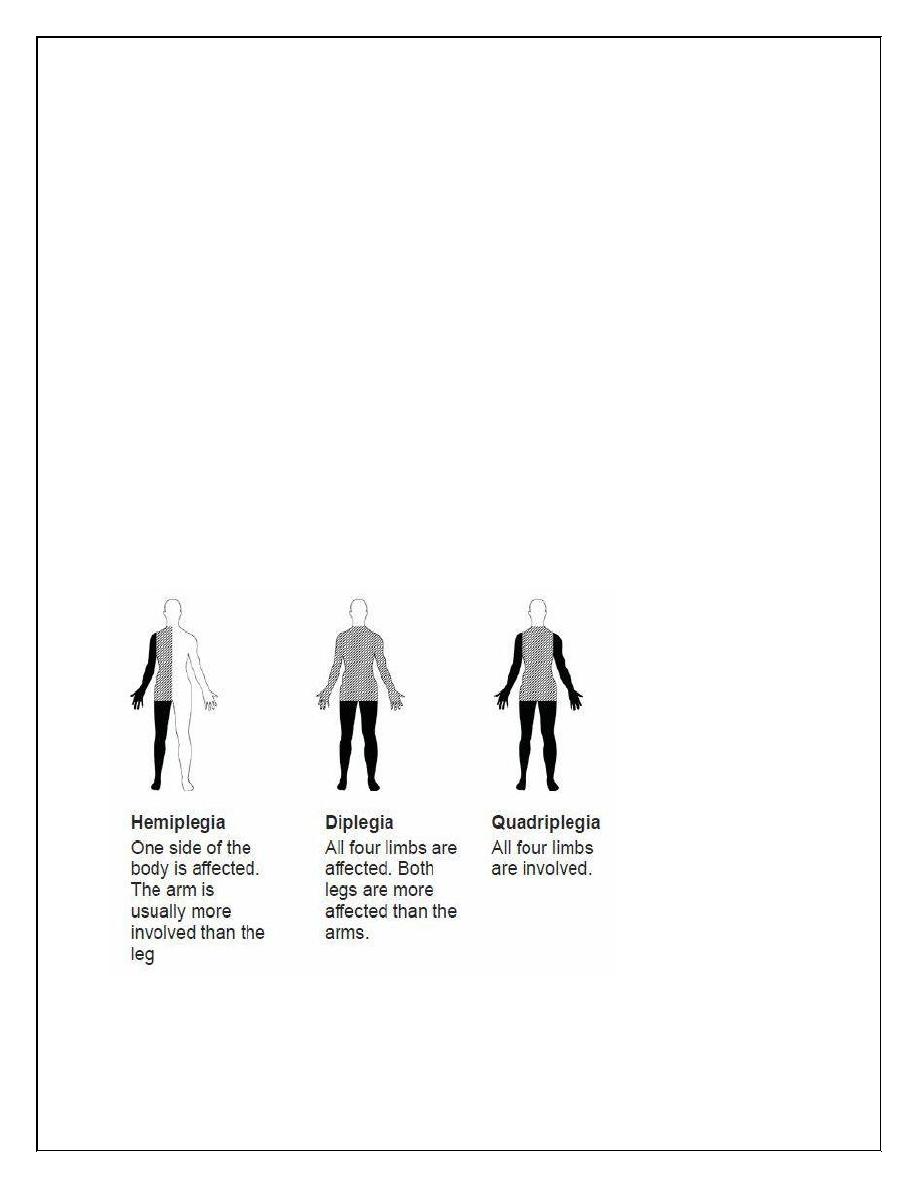
CP is classified according to the pattern of neurologic involvement into:
1-Spastic :
Pediatrics
NEUROLOGY
5
Spastic hemiplegia
Spastic diplegia
Spastic quadriplegia
2-Dyskinetic (Extrapyramidal):
Athetoid
Choreoathetoid
Spastic Hemiplegia (25%)
↓ spontaneous movements on the affected
side; the infant show hand preference at very early age. It affect the
upper > lower limbs which may show growth arrest that especially
affect distal part of the limb. walking is delayed until 18–24 mo. With
circumductive gait.
About one third of patients have a seizure develops in the 1st or 2ed
year .
*≈25% have cognitive abnormalities including mental retardation.
Examination of the extremities showing:
1-Growth arrest, particularly in the hand and thumb .
2-Spasticity in the affected extremities, particularly the ankle, causing an
equinovarus deformity of the foot.
3-An affected child often walks on tiptoe because of the increased tone.
4-Ankle clonus and a Babinski sign (plantar extensor response) may be
present.
5-The deep tendon reflexes are increased.
Pediatrics
NEUROLOGY
6
Spastic Diplegia (30%)
bilateral spasticity of the lower > upper limbs; it usually appear when
the infant begin to crawl→ Commando crawl, but it usually not
associated with mental retardation or epilepsy
By examination:
1-Spasticity in the legs with hyperreflexia .
2-Ankle clonus, and a bilateral Babinski sign.
3-When the child is suspended by the axillae, a scissoring posture of
the lower extremities.
4-Walking is delayed , and the child walks on tiptoe
Spastic Quadriplegia (20%)
the most severe one, it affects all extremities with signs of upper motor
neuron (UMN) disease → scissoring posture of legs & later →
contracture deformities & disuse atrophy of muscles.
It usually associated with mental retardation, epilepsy, & pseudo-bulbar
palsy which cause swallowing difficulty → aspiration pneumonia.
By examination :
1-increased tone and spasticity in all extremities.
2-Decreased spontaneous movements, brisk reflexes, and Babinski sign.
3-Flexion contractures of the knees and elbows are often present by late
childhood.
Children with spastic quadriparesis often have athetosis.
Pediatrics
NEUROLOGY
7
Athetoid (Choreoathetoid CP 25%
CP accrue due to lesion in the basal ganglia most likely associated
with birth asphyxia or kernicterus causing hypotonia & head lag
early in life, then the tone will ↑ & associated with rigidity & dystonia
over several years.
Signs of UMN disease are absent, seizures are uncommon & intellect is
preserved, but speech is typically affected because the oropharyngeal
muscles are involved & IQ is normal in many patients
Investigations
C-T scan , MRI of brain
Tests for hearing & vision.
Genetic evaluation.
Treatment
The aim of treatment is to make use of all patients abilities as effective
as possible by:
Physiotherapy, occupational therapy & exercises are important to
prevent the development of contractures & enable the child to perform
the daily activities (feeding, dressing, bathing).
* Orthopaedic surgeon for contractures & tendon release.
* Speech therapist.
* Ophthalmologist for visual proplemes (Strabismus, nystagmus).
*Hearing aids.
*Treat spasticity : Several drugs used, including:
oral dantrolene sodium.
Pediatrics
NEUROLOGY
8
benzodiazepines (oral diazepam).
baclofen (oral or intrathecal).
Botulinum toxin: injected into specific muscle groups (it prevent release
of acetylcholine from the nerve ends, which leads to prolonged
relaxation of the muscle).
*Reserpine or tetrabenazine can be useful for hyperkinetic movement
disorders including athetosis or chorea.
-Treat seizure by anticonvulsants
- Constipation treated by laxative.
-Those with failure to thrive & difficult swallowing may require
nasogastric tube feeding.
