د
.
أشرف مزاحم الشاكر
كلية طب نينوى
الجراحة الع
امة
1
TUBERCULOUS LYMPHADENITIS
Causative
organism:
Mycobacterium
tuberculosis (not M. bovis).
Site:
_ Common in neck lymph nodes.
_
Common
in
upper
deep
cervical
(jugulodigastric—54%) lymph nodes.
_ Next common is posterior triangle lymph
nodes (22%).
_ Disease can also occur in other lymph nodes
like, axillary lymph nodes, para-aortic lymph
nodes, mesenteric lymph nodes, inguinal
lymph nodes.
_ Disease may be associated with HIV
infection, lymphomas.
Mode of Infection
_ Usually through the tonsils, occasionally through blood from lungs. Tonsillar
infection shows multiple tubercles on its surface; from here infection spreads into
jugulodigastric nodes (anterior triangle nodes) then to other nodes. Infection
reach lymph node first into subcapsular space/sinus then to lymph node cortex
which contains plenty of lymph follicles. Matting is due to periadenitis involving
subcapsular sinus/space of lymph node. In children infection to neck node can
come from either tonsils or adenoids or both. When it occurs from adenoids,
lymph nodes in posterior triangle are involved through retropharyngeal
lymphatics.
_ It may be associated with pulmonary tuberculosis or renal tuberculosis.
Through blood infection reaches medullary cords of lymph node and so medulla
of lymph node.
_ Rarely spread can occur from tuberculous lesion of the apex of lung through
suprapleural Sibson’s fascia/membrane to supraclavicular nodes.
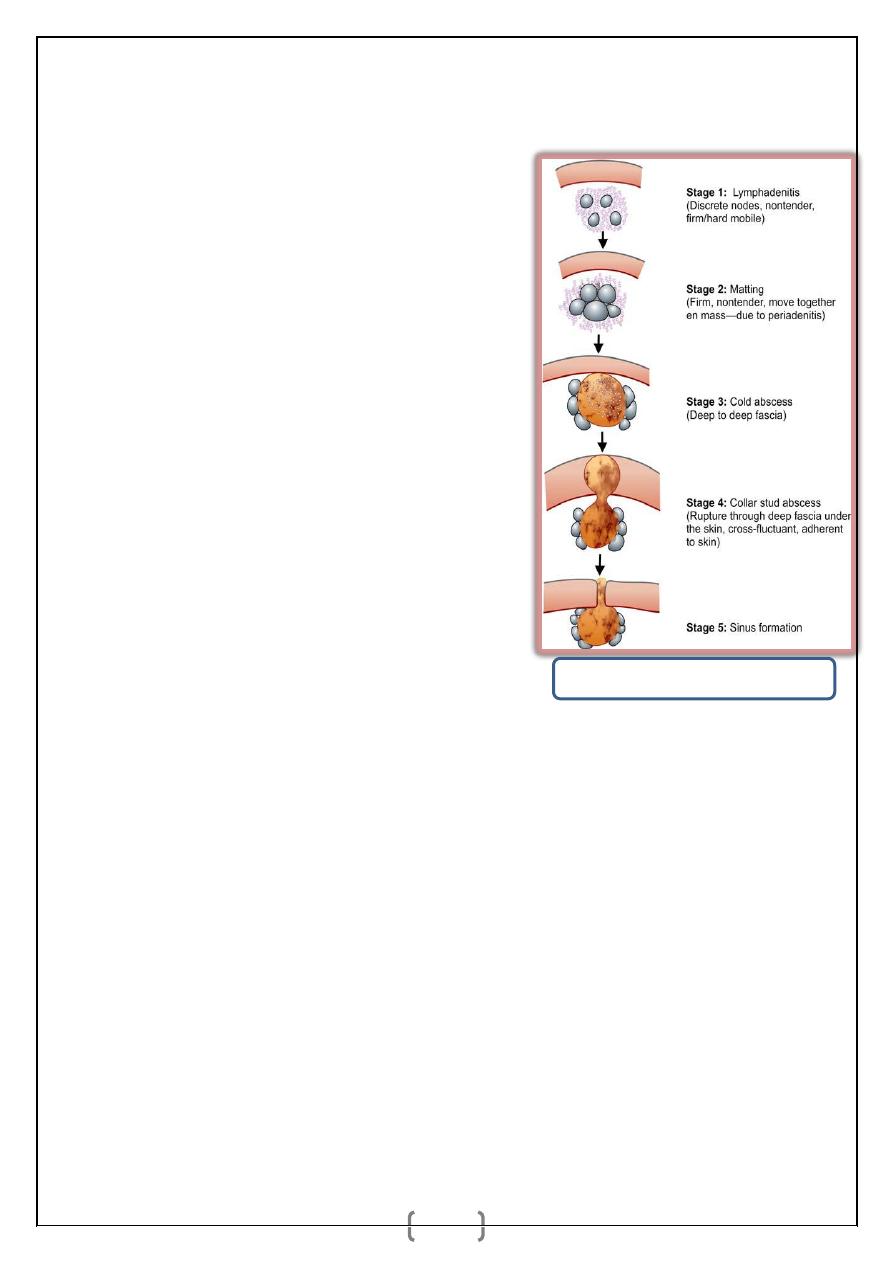
Stages of tuberculous lymphadenitis
د
.
أشرف مزاحم الشاكر
كلية طب نينوى
الجراحة الع
امة
2
_ Often fibrosis and calcification can
occur with or without treatment.
Gross Pathology
_ Firm, matted, lymph node, with
cut
section
showing
yellowish
caseating material.
Microscopic Features
_ Epithelioid cells with caseating
material are seen along with
Langhan’s type of giant cells.
Clinical Features
_ Swelling in the neck which is fi
rm, matted.
_ Cold abscess is soft, smooth,
nontender,
fluctuant,
without
involvement of the skin. It is not warm.
_ As a result of increased pressure, cold
abscess ruptures out of the deep fascia to form collar stud abscess which is
adherent to the overlying skin.
_ Once collar stud abscess bursts open, discharging sinus is formed. It can be
multiple, wide open mouth, often undermined, nonmobile with bluish color
around the edge. It is usually not indurated.
_ Tonsils may be studded with tubercles and so clinically should always be
examined.
_ Associated pulmonary tuberculosis should also be looked for. In 20% cases of
tuberculous lymphadenitis, there may be associated pulmonary tuberculosis or it
may be a primary focus.
_ Cervical spine is examined for tuberculosis.
_ Bluish hyperpigmented involved overlying skin is called as scrofuloderma.
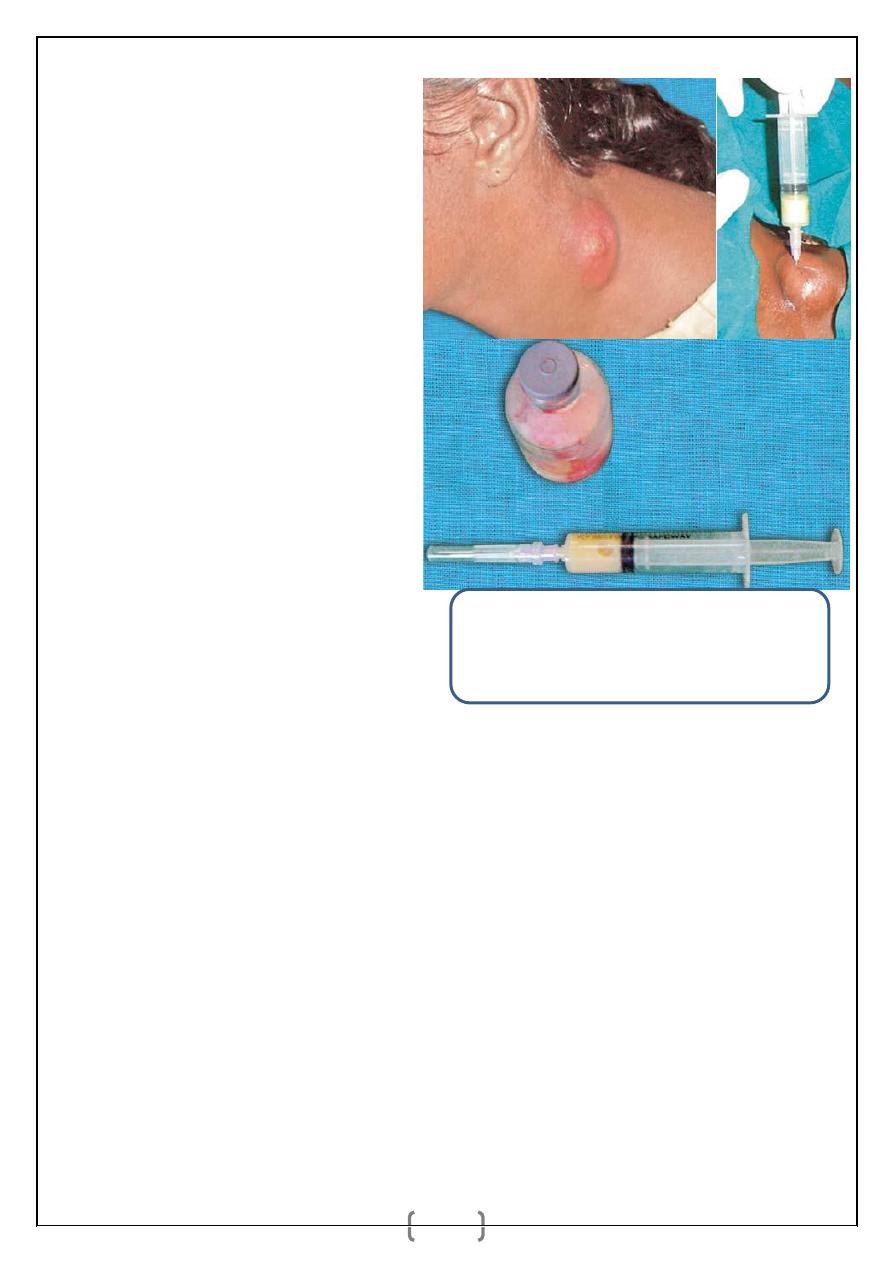
Typical cold abscess in the neck in which pus is
aspirated. Pus should be sent for cytology (for
epithelioid cells), staining (Ziehl-Neelsen—AFB)
and culture.
د
.
أشرف مزاحم الشاكر
كلية طب نينوى
الجراحة الع
امة
3
_ Tuberculous pus with caseating cheesy creamy material is infective as it
contains multiplying organisms.
_ Atypical mycobacterial tuberculosis can occur occasionally. Such disease may
be resistant to drug therapy.
_ Sinus may persist due to—fibrosis, calcification, secondary infection,
inadequate reach of drug to maintain optimum concentration in caseation.
Differential Diagnosis
1. Nonspecific lymphadenitis.
2. Lymphomas, and chronic lymphatic leukaemia.
3. Secondaries in the neck.
4. Branchial cyst mimics cold abscess.
5. Lymph cyst mimics cold abscess.
6. HIV with lymph node involvement.
7. When there is discharging sinus—actinomycosis.
Investigations
_ Haematocrit, ESR, peripheral smear.
_ FNAC of lymph node and smear for AFB and culture.
(FNAC is very useful but not as superior as open node biopsy.)
_ Open biopsy when FNAC is inconclusive. Open biopsy is more reliable for
tuberculosis (and also in lymphoma; but it is contraindicated in node
secondaries); entire node ideally two nodes if possible has to be taken intact; one
in formalin for pathology, other in normal saline for microbiology (AFB).
_ HIV test (ELISA and western blot).
_ Lowenstein Jensen media is used for culture which takes 6 weeks to give result;
so selinite media is often used which shows growth in 5 days.
_ Mantoux test may be useful; but not very reliable.
د
.
أشرف مزاحم الشاكر
كلية طب نينوى
الجراحة الع
امة
4
_ Chest X-ray to look for pulmonary tuberculosis.
_ Polymerase chain reaction (PCR) is very useful method.
Treatment
Drugs
Antitubercular drugs has to be started:
1. Rifampicin 450 mg OD on empty stomach. It is bactericidal. It discolours
urine red. It is also hepatotoxic.
2. INH: 300 mg OD. It is bactericidal. It causes into lerance of GIT, Neuritis,
Hepatitis (INH).
3. Ethambutol 800 mg OD. It is bacteriostatic. It causes GIT intolerance,
retrobulbar neuritis (green colour blindness).
4. Pyrazinamide 1500 mg OD (or 750 mg BD). It is bactericidal. It is
hepatotoxic, also causes hyper uricaemia and increases psychosis.
Duration of treatment is usually 6-9 months.
Aspiration
When there is cold abscess, initially it is aspirated. (Wide bore needle is
introduced into the cold abscess in a nondependent site along a “Z” track (in zig-
zag pathway) so as to prevent sinus formation.)
Incision and drainage
If it recurs, then it should be drained. Drainage is done through a nondependent
incision. After draining the caseating material, wound is closed without placing a
drain.
Surgical removal
Surgical removal of tubercular lymph nodes are indicated when
1. There is no local response to drugs or
2. When sinus persists.
د
.
أشرف مزاحم الشاكر
كلية طب نينوى
الجراحة الع
امة
5
It is done by raising skin flaps and removing all caseating material and lymph
nodes. Care is taken not to injure major structures.
Excision of the sinus track is often essential when sinus develops.
SECONDARIES IN NECK LYMPH NODES
_ It is commonly from squamous cell carcinoma, but can also be from
adenocarcinoma or melanoma.
_ Squamous cell carcinoma is mainly from oral cavity,
_ Adenocarcinoma is usually from GIT, commonly involving left supraclavicular
lymph nodes.
_ Breast, lungs, abdominal viscera are other areas where primary may cause
secondaries in neck which should be examined when suspected.
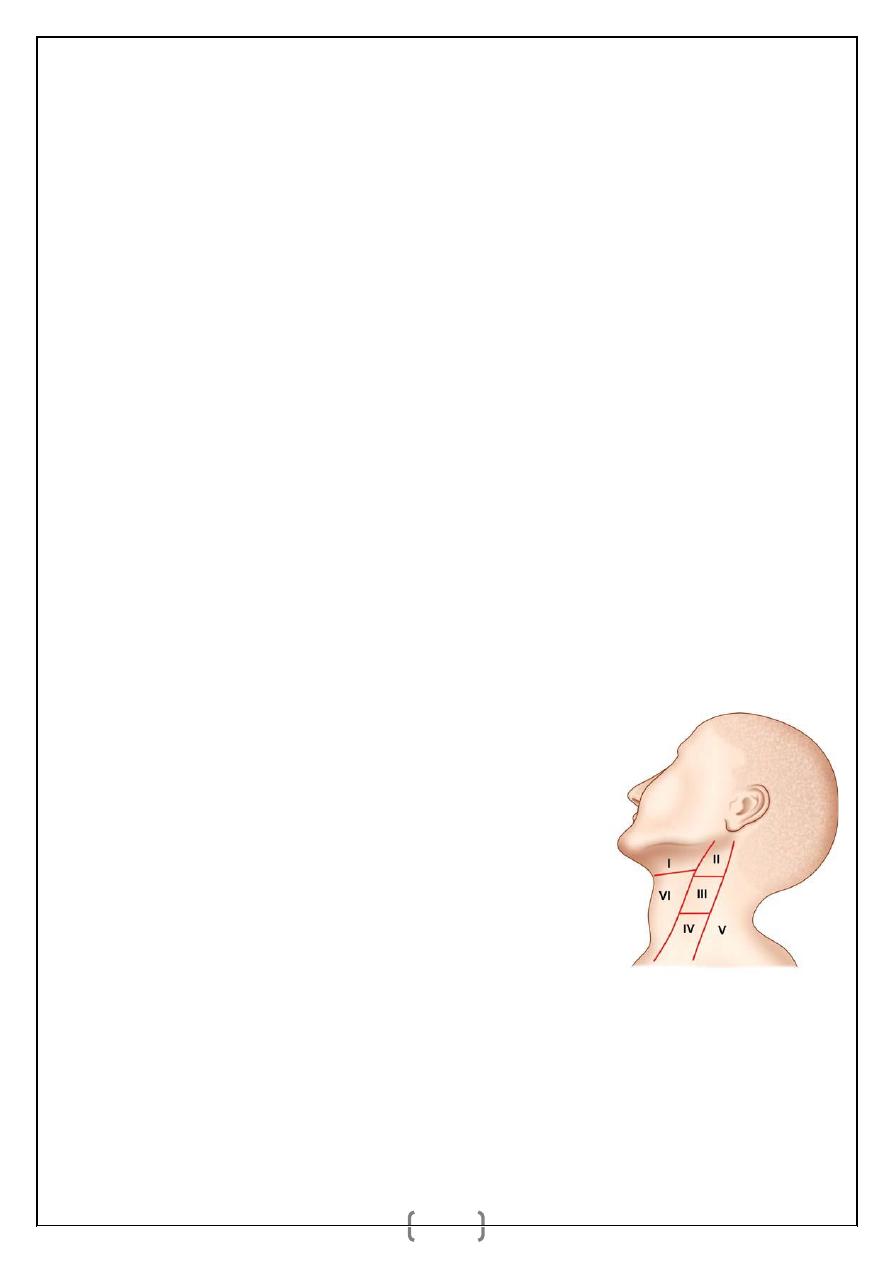
Levels in Neck Nodes (Memorial Sloan— Kettering Cancer Centre Levelling
of Neck Nodes)
Level I—Submental (Ia) and submandibular (Ib) lymph nodes.
Level II—Lymph nodes in upper deep cervical
region. (It extends from base of skull to hyoid
bone and from lateral margin of sternohyoid to
posterior margin of sternomastyoid muscle).
Level III—Lymph nodes in middle cervical
region (from hyoid bone to omohyoid muscle or
cricothyroid membrane).
Level IV—Lymph nodes in lower cervical region
(from omohyoid muscle to clavicle).
Level V—Lymph nodes in posterior triangle
including
supraclavicular
region
from
posterior
border
of
sternocleidomastoid muscle to anterior border of trapezius muscle.
Level VI—Lymph nodes in the midline neck—pretracheal and prelaryngeal
from hyoid bone above to suprasternal notch below, medial border of
carotid sheath on either side.
د
.
أشرف مزاحم الشاكر
كلية طب نينوى
الجراحة الع
امة
6
Level VII—Lymph nodes in the mediastinum. inferior to suprasternal notch
to innominate artery below.
Features of Secondaries in Neck:
1. features related to cervical lymph nodes:
Common in adult/elderly male (Male to female ratio is 4:1), presents as painless
rapidly increasing localised swelling in the neck.
_ Nodular surface and hard in consistency, often fi xed when it is advanced.
_ Secondaries from papillary carcinoma of thyroid can be soft, cystic with
brownish black fluid.
2. features related to primary affected organ:
Types of Secondaries in the Neck
1. Secondaries in the Neck with Known Primary
Here secondaries are present and primary has been identified clinically in the oral
cavity, pharynx, larynx, thyroid or other areas. Biopsy from the primary and
FNAC from the secondaries are done. Primary is treated accordingly either by
curative radiotherapy or by surgery (wide excision). Secondaries, when mobile
are treated by radical lymph node block dissection in the neck.
2. Secondaries in the Neck with Clinically Unidentified Primary: Hard neck
lymph nodes are the secondaries, but primary has not been identified clinically.
FNAC of the neck node is done and secondaries are confirmed. Then search for
the primary is done by various investigations.
د
.
أشرف مزاحم الشاكر
كلية طب نينوى
الجراحة الع
امة
7
They are:
a. Panendoscopy
_ Nasopharyngoscopy.
_ Laryngoscopy.
_ Oesophagoscopy.
_ Bronchoscopy.
b. Blind biopsies are taken from fossa of Rosenmuller, lateral wall of pharynx,
pyriform fossa, tonsillar bed, base of tongue, subglottic region (larynx). It is
called as surveillance biopsy and is done to reveal unknown primary in 15% of
cases of secondaries in neck. If this surveillance biopsy is negative, then
ipsilateral tonsillectomy may be needed.
c. FNAC of thyroid and suspected areas.
d. CT scan.
Once the biopsy confirms the primary, it is treated either by surgery or by
curative radiotherapy. Secondaries in the neck is treated by radical neck
dissection.
3. Secondaries in the Neck with an Occult Primary:
Investigations for Secondaries in Neck:
_ FNAC of secondary: Open incision biopsy is avoided in lymph node
secondaries.
_ Biopsy from primary: Incision biopsy is the choice here.
د
.
أشرف مزاحم الشاكر
كلية طب نينوى
الجراحة الع
امة
8
_ Blind biopsies from suspected areas.
_ Nasopharyngoscopy, laryngoscopy, bronchos copy, oesophagoscopy—
panendoscopy with examination under anaesthesia.
_ CT scan is to see the base of skull, paranasal sinuses, nasopharynx, extension
of primary tumour/secondary deposits; CT scan of chest and abdomen.
_ Chest X-ray to visualise primary or secondaries in case melanomas or
mediastinal nodes.
_ MRI scan or PET scan in conjunction with CT scan or MRI. MRI identifi es
soft tissue extension/changes; guided primary biopsy is possible; extension into
bone is identified.
_ CT chest and abdomen in case of infraclavicular primaries or to assess nodes.
Triple endoscopy includes direct/indirect laryngoscopy, oesophagoscopy and
bronchoscopy.
Differential Diagnosis
1. Lymphomas.
2. Tuberculous lymphadenitis.
3. Nonspecific lymphadenitis.
4. HIV.
5. Chronic lymphatic leukaemia.
Treatment
_ Primary is treated depending on the site, either by wide excision (surgery) or
by curative radiotherapy. Then the secondaries are treated.
_ Secondaries when mobile, are treated by radical neck dissection.
_ When fixed it is inoperable. Palliative external radiotherapy is given to palliate
pain and to prevent the anticipated bleeding.
_ Sometimes initially, external radiotherapy is given to downstage the disease so
that it becomes operable and later classical block dissection can be done.
د
.
أشرف مزاحم الشاكر
كلية طب نينوى
الجراحة الع
امة
9
_ Postoperative RT is given after neck dissection when— more than two lymph
nodes are positive for metastases; nodes show metastases at two or more level;
extracapsular spread in lymph node. Suspected occult primary is
included/covered in the RT fi eld. RT is also given to contralateral neck nodes in
nasopharyngeal carcinoma. Level II lymph node alone from an occult is more
likely to be from nasopharyngeal carcinoma and RT is preferred in such
situation covering nasopharyngeal area; later RND is done.
