1
The Normal Menstrual cycle L1&2
Introduction :
The external manifestation of a normal menstrual cycle is the presence
of regular vaginal bleeding . This occurs as a result of the shedding of
the endometrial lining following failure of fertilization of the oocyte or
failure of implantation . The cycle depends on changes occurring within
the ovaries and fluctuation in ovarian hormone levels , that are
themselves controlled by the pituitary and hypothalamus , the
hypothalamo-pituitary-ovarian axis ( HPO ) .
Hypothalamus :
The hypothalamus in the forebrain secretes the peptide hormone
gonadotrophn-releasing hormone ( GnRH ) , which in turn controls
pituitary hormone secretion . GnRH must be released in a pulsatile
fashion to stimulate pituitary secretion of luteinizing hormone ( LH ) and
follicle stimulating hormone ( FSH ) . If GnRH is giving in a constant
high dose , it desensitizes the GnRH receptor and reduces LH and FSH
release .
Clinical view :
Drugs that are GnRH agonists ( e.g. buserelin and goserelin ) .
Although they mimic the GnRH hormone , when administered
continuously , they will downregulate the pituitary and consequently
decrease LH and FSH secretion . This has effects on ovarian function
such that oestrogen and progesterone levels also fall . These preparations
are used as treatments for endometriosis and to shrink fibroids prior
surgery .
Pituitary gland
GnRH stimulation of the basophil cells in the anterior pituitary gland
causes synthesis and release of the gonadotrophic hormones , FSH and
LH . This process is modulated by the ovarian sex steroid hormones
oestrogen and progesterone ( see Figure 1 ) . Low levels of oestrogen
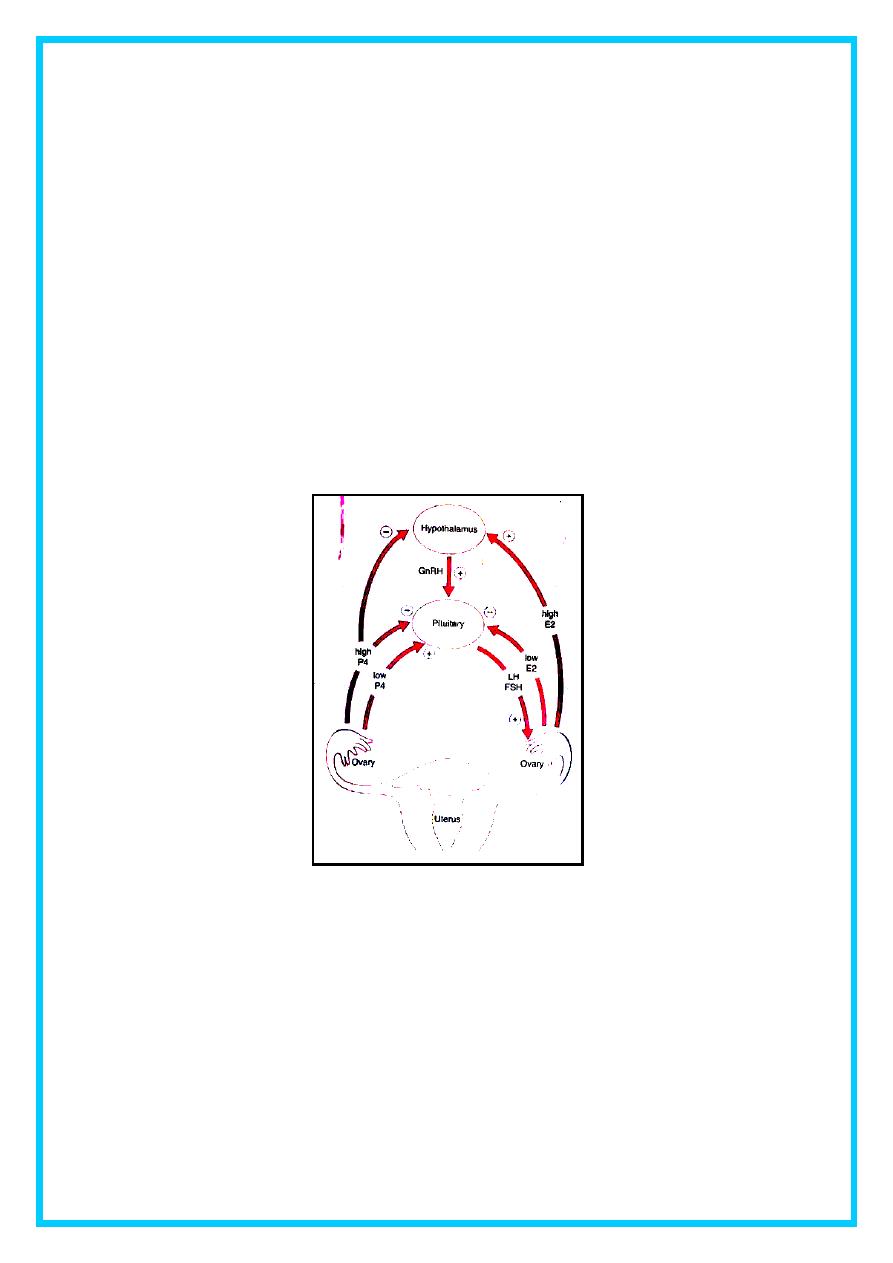
2
have an inhibitory effect on LH production ( negative feedback ) ,
whereas high levels of oestrogen will increase LH production ( positive
feedback ) . The mechanism of action for the positive feedback effect of
oestrogen involves an increase in GnRH receptor concentrations , while
the mechanism of the negative feedback effect is uncertain .
The high levels of circulating oestrogen in the late follicular phase of
the ovary act via the positive feedback mechanism to generate a
periovulatory LH surge from the pituitary .
The clinical relevance of these mechanisms is seen in the use of the
combined oral contraceptive pill , which artificially creates a constant
serum oestrogen level in the negative feedback range , inducing a
correspondingly low level of gonadotriphin hormone release .
Figure (1) Hyothalamo-pituitary-ovarian axis .
Unlike oestrogen , low levels of progresterone have a positive
feedback effect on pituitary LH and FSH secretion ( as seen immediately
prior to ovulation ) and contribute to the FSH surge . High levels of
progesterone , as seen in the luteal phase , inhibit pituitary LH and FSH
production . Positive feedback effects of preogesterone occur via
increasing sensitivity to GnRH in the pituitary . Negative feedback
effects are generated through both decreased GnRH production from the
3
hypothalamus and decreased sensitivity to GnRH in the pituitary . It is
known that progesterone can only have these effects on gonadotropic
hormone release after priming by oestrogen ( Figure 2 ) .
There are other hormones which are involved in pituitary
gonadotrophin secretion . Inhibin inhibits pituitary FSH secretion ,
whereas activin stimulates it .
Ovary
Ovaries with developing oocytes are present in the female fetus from
an early stage of development . By the end of the second trimester in
utero , the number of occytes has reached a maximum and they arrest at
the first prophase step in meiotic division . No new occytes are formed
during the female lifetime . With the onset of menarche , the primordial
follicles containing oocytes will activate and grow in a cyclical fashion ,
causing ovulation and subsequent menstruation in the event of non-
fertilization .
In the course of a normal menstrual cycle , the ovary will go through
three phases :
1. Follicular phase .
2. Ovulation .
3. Luteal phase .
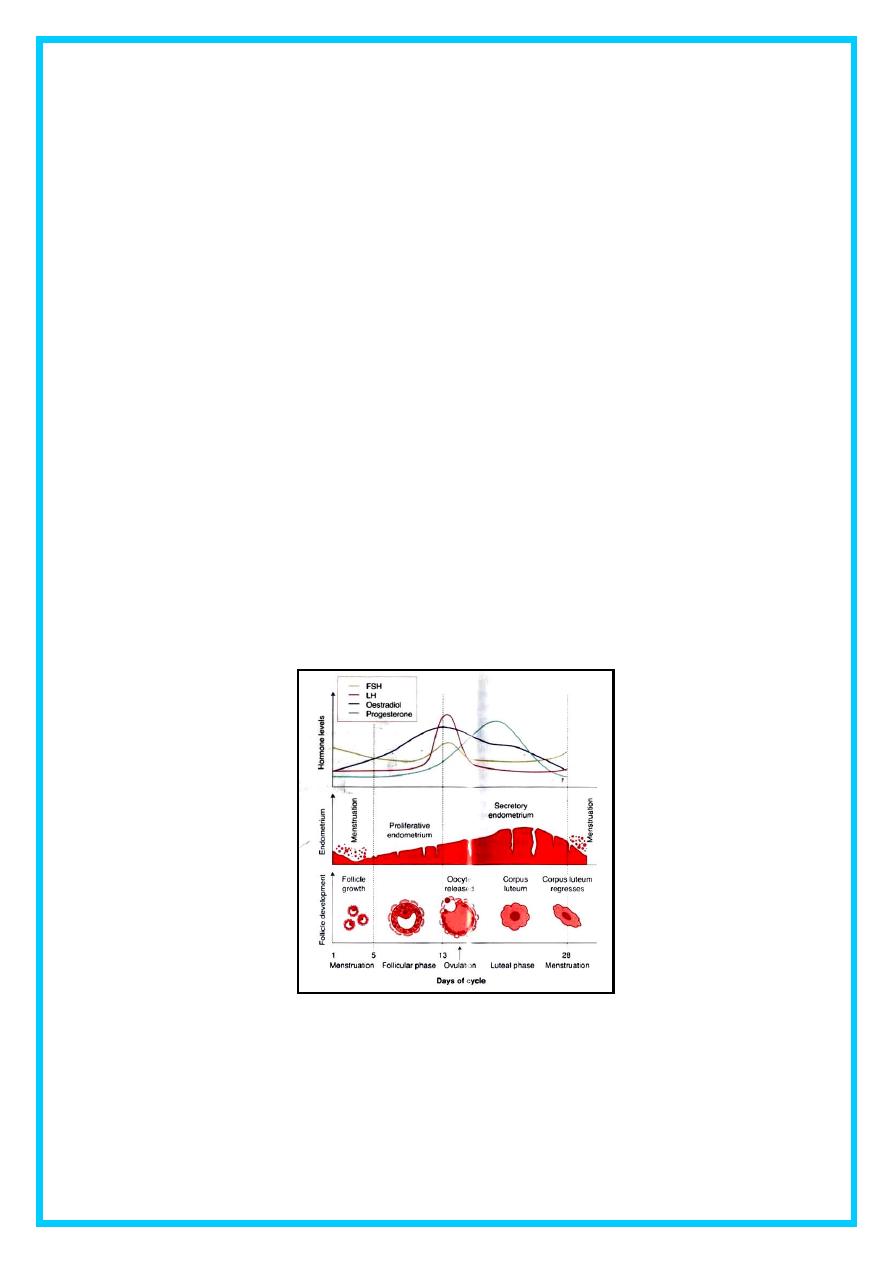
Follicular phase :
The initial stages of follicular development are independent of
hormone stimulation . However , follicular development will fail at the
preantral stage and follicular atresia will ensue if pituitary hormones LH
and FSH are absent .
FSH levels rise in the first days of the menstrual cycle , when
oestrogen , progesterone and inhibin levels are low . This stimulates a
cohort of small antral follicles on the ovaries to grow .
Within the follicles , there are two cell types which are involved in
the processing of steroids , These are the theca and the granulosa cells ,
which respond to LH and FSH stimulation , respectively . LH
stimulation production of androgens from cholesterol within theca cells .
4
These androgens are converted into oestrogens by the process of
aromatization in granulose cells , under the influence of FSH . The roles
of FSH and LH in follicular development are demonstrated by studies on
women undergoing ovulation induction in whom endogenous
gonadotrophin production has been suppressed . If pure FSH alone is
used for ovulation induction , as ovulatory follicle can be produced , but
oestrogen production is markedly reduced . Both FSH and LH are
required to generate a normal cycle with adequate amounts of
oestrogen .
As the follicles grow and oestrogen secretion increases , there is
negative feedback on the pituitary to decrease FSH secretion . This
assists in the selection of one follicle to continue in its development
towards ovulation – the dominant follicle . In the ovary , the follicle
which has the most efficient aromatase activity and highest
concentration of FSH – induced LH receptors will be the most likely to
survive as FSH levels drop , while smaller follicles will undergo atresia .
The dominant follicle will go on producing oestrogen and also inhibin ,
which enhances androgen synthesis under LH control .
Figure (2) Changes in hormone levels , endometrium and follicle development
during the menstrual cycle .
5
Clinical view :
Administration of exogenous gonadotrophins is likely to stimulate
growth of multiple follicles which continue to develop and are released
at ovulation ( and can lead to multiple gestations at a rate of around 30
per cent ) .
This situation is used to advantage in patients requiring in vitro
fertilization ( IVF ) , as many occytes can be harvested from ovaries
which have been stimulated as described above .
There are other autocrine and paracrine mediators playing a role in the
follicular phase of the menstrual cycle .
These include : Inhibin and activin . Inhibin participates in feedback to
the pituitary to downregulate FSH release , and also appears to enhance
ongoing androgen synthesis . Activin is structurally similar to inhibin ,
but has an opposite action is structurally similar to inhibin , but has an
opposite action . It is produced in granulosa cells and in the pituitary ,
and acts to increase FSH binding on the follicles .
Insulin-like growth factors ( IGF – I , IGT – II ) act as paracrine
regulators .
1. In the follicular phase , IGF-I is produced by theca cells under the
action of LH. IGF-I receptors are present on both theca granulosa
cells . Within theca , IGF-I augments LH-induced steroidogenesis .
In granulosa cells , IGF-I augments the stimulatory effects of FSH
on mitosis , aromatase activity and inhibin production .
2. In the preovulatory follicle , IGF-I enhances LH-induced
progesterone production from granulosa cells .
3. Following ovulation , IGF-II is produced from luteinized
granulosa cells , and acts in an autocrine manner to augment LH-
induced proliferation of granulosa cells .
Kisspeptins are proteins which have more recently been found to play a
role in regulation of the HPO axis , via the mediation of the metabolic
hormone leptin's effect on the hypothalamus , Leptin is thought to be key
in the relationship between energy production , weight and reproductive
health . Mutations in the kisspeptin receptor , gpr-54 , are associated
6
with delayed or absent puberty , probably due to a reduction in leptin-
liked triggers for gonadotrophin release .
Ovulation
By the end of the follicular phase , which lasts an average of 14 days , the
dominant follicle has grown to approximately 20 mm in diameter . As the
follicle matures :
1. FSH induces LH receptors on the granulosa cells to compensate for
lower FSH levels and prepare for the signal ovulation .
2. Production of oestrogen increases until they reach the necessary
threshold to exert a positive feedback effort on the hypothalamus and
pituitary to cause the LH surge .
3. This occurs over 24 – 36 hours , during which time the LH-induced
luteinization of granulosa cells in the dominant follicle causes
progesterone to be produced , adding further to the positive feedback
for LH secretion and causing a small periovulatory rise in FSH .
4. Androgens , synthesized in the theca cells , also rise around the time of
ovulation and this is thought to have an important role in stimulating
libido , ensuring that sexual activity is likely to occur at the time of
greatest fertility .
Clinical view :
1. The LH surge is one of the best predictors of imminent ovulation , and
this is the hormone detected in urine by most over-the-counter
'ovulation predictor' tests .
2. The LH surge has another function in stimulating the resumption of
meiosis in the occyte just prior to its release . The physical ovulation of
the oocyte occurs after breakdown of the follicular was occurs under
the influence of LH , FSH and progesterone-controlled proteolytic
enzymes , such as plasminogen activators and protaglandins . There
appears to be an inflammatory-type response within the follicle wall
which may assist in extrusion of the oocyte by stimulating smooth
muscle activity .
Thus , women wishing to become pregnant should be advised to avoid
taking prostaglandin synthetase inhibitors .
7
Luteal phase :
After the release of the oocyte , the remaining granulosa and theca
cells on the ovary form the corpus luteum . The granulosa cells have a
vacuolated appearance with accumulated yellow pigment , hence the
name corpus luteum ( ' yellow body ' )
Ongoing pituitary LH secretion and granulosa cell activity ensures a
supply of progesterone which stabilizes the endometrium in preparation
for pregnancy . Progesterone levels are at their highest in the cycle
during the luteal phase . This also has the effect of suppressing FSH and
LH secretion to a level that will not produce further follicular growth in
the ovary during that cycle .
The luteal phase lasts 14 days in most women , without great
variation . In the absence of beta human chorionic ganadotrophin
( BHCG ) being produced from an implanting embryo , the corpus
luteum will regress in a process known as luteolysis .
The withdrawal of progesterone has the effect on the uterus of causing
shedding of the endometrium and thus menstruation . Reduction in
levels of progesterone , oestrogen and inhibin feeding back to the
pituitary cause increased secretion of gonadotrophic hormone ,
particularly FSH . New preantral follicles begin to be stimulated and the
cycle begins anew .
Endometrium :
The specific secondary changes in the uterine endometrium give the
most obvious external sign of regular cycles .
Menstruation :
The endometrium is under the influence of sex steroids that circulate
in females of reproductive age .
During the ovarian follicular phase , the endometrium undergoes
profileration ( the ' proliferative phase ' ) ; during the ovarian luteal
phase , it has its ' secretory phase ' , Decidualization , the formation of a
specialized glandular endometrim , is an irreversible process and
apoptosis occurs if there is no embryo implantation . Menstruation
8
(day 1) is the shedding of the 'dead' endometrium and ceases as the
endometrium regenerates ( which normally happens by day 5 – 6 of the
cycle ) .
The endometrium is composed of two layers , the uppermost of which
is shed during menstruation . A fall in circulating levels of oestrogen and
progesterone approximately 14 days after ovulation leads to loss of
tissue fluid , vasoconstriction of spiral arterioles and distal ischaemia .
This results in tissue breakdown , and loss of the upper layer along with
bleeding from fragments of the remaining arterioles is seen as menstrual
bleeding . Enhanced fibrinolysis reduces clotting .
Clinical view :
1. The effects of oestrogen and progesterone on the endometrium can
be reproduced artificially , for example in patients taking the
combined oral contraceptive pill or hormone replacement therapy
who experience a withdrawal bleed during their pill-free week
each month . Vaginal bleeding will cease after 5 – 10 days as
arterioles vasconstrict and the endometrium begins to regenerate .
2. In rare cases , the tissue breakdown and vasoconstriction does not occur
correctly and the endometrium may develop scarring which goes on to
inhibit its function . This is known as ' Asherman's syndrome ' . The
endocrine influences in menstruation are clear . However there is also
paracrine mediators influence in menstruation ,include : prostaglandin
F2 a , endothelin-1 and platelet activating factor ( PAF ) are
vasoconstrictors which are produced within the endometrium . They
may be balanced by the effect of vasodilator agents , such as
prostaglandin E
2
, prostacyclin ( PGI ) and nitric oxide (NO) , which
are also produced by the endometrium .
3. Recent research has shown that progesterone withdrawal increases
endometrial prostaglandin ( PG ) synthesis and decreases PG
metabolism . The COX-2 enzyme and chemokines are involved in PG
synthesis and this is likely to be the target of non-steroidal anti-
inflammatory agents used for the treatment of heavy and painful
periods .
9
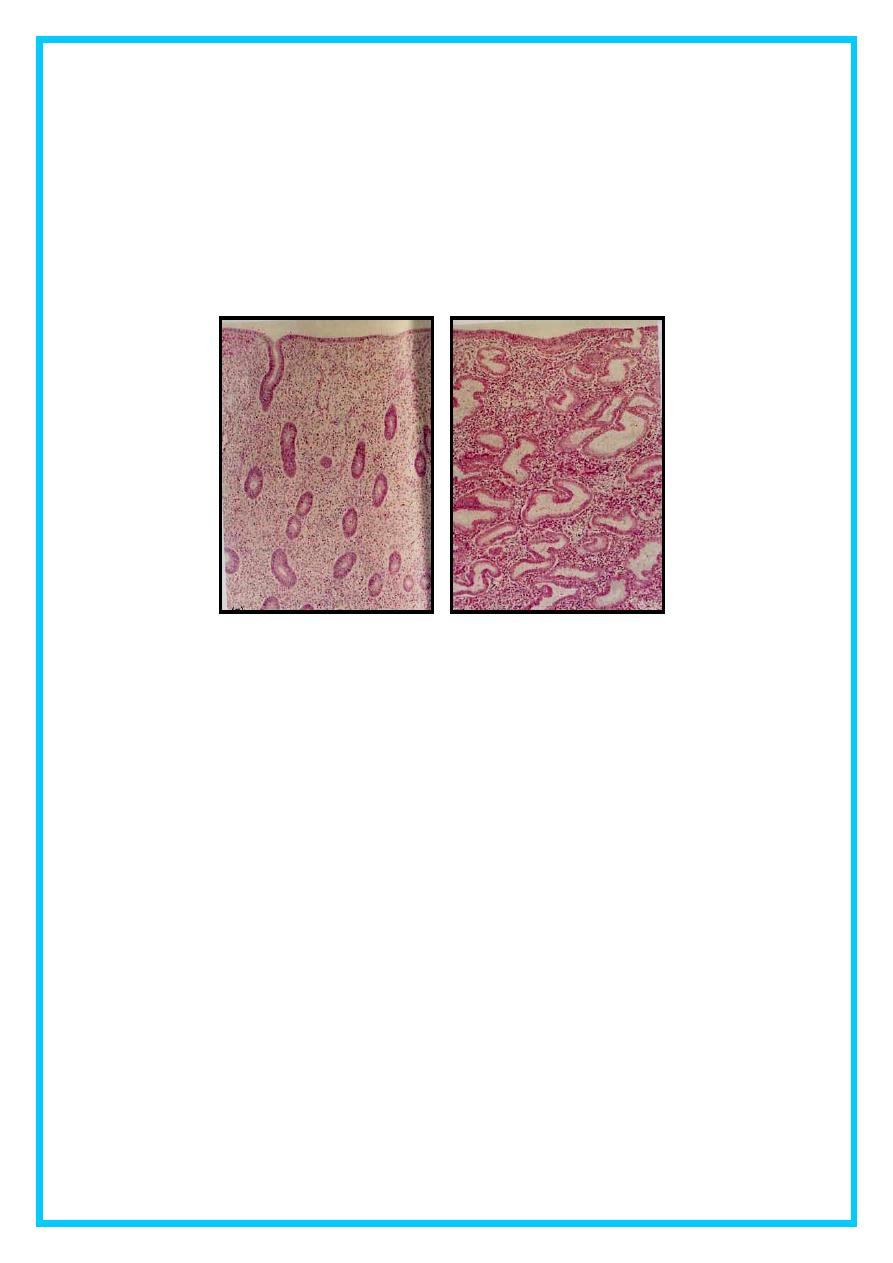
The proliferative phase :
Once endometrial repair is complete . After this time , the endometrium
enters the proliferative phase , when glandular and stromal growth occur . The
epithelium lining the endometrial glands changes from a single layer of
columnar cells to a pseudostratified epithelium with frequent mitoses .
Endometrial thickness increases rapidly , from 0.5 mm at menstruation to
3.5 – 5 mm at the end of the proliferative phase .
Figure (3) Tissue sections of normal endometrium during proilferative and
secretory phases of the menstrual cycle .
The secretory phase
After ovulation ( generally around day 14 ) , there is a period of
endometrial glandular secretory activity . following the progesterone
surge , the oestrogen-induced cellular proliferation is inhibited and the
endometrial thickness does not increase any further . However , the
endometrial glands will become more tortuous , spiral arteries will
grow , and fluid is secreted into glandular cells and into the uterine
lumen . Later in the secretory phase , progesterone induces the formation
of a temporary layer , known as the decidua . Stromal cells show
increased mitotic activity , nuclear enlargement and generation of a
basement membrane .
Recent research into infertility has identified apical membrane
projections of the endometrial epithelial cells known as pinopodes ,
which appear after day 21-22 and appear to be a progesterone-dependent
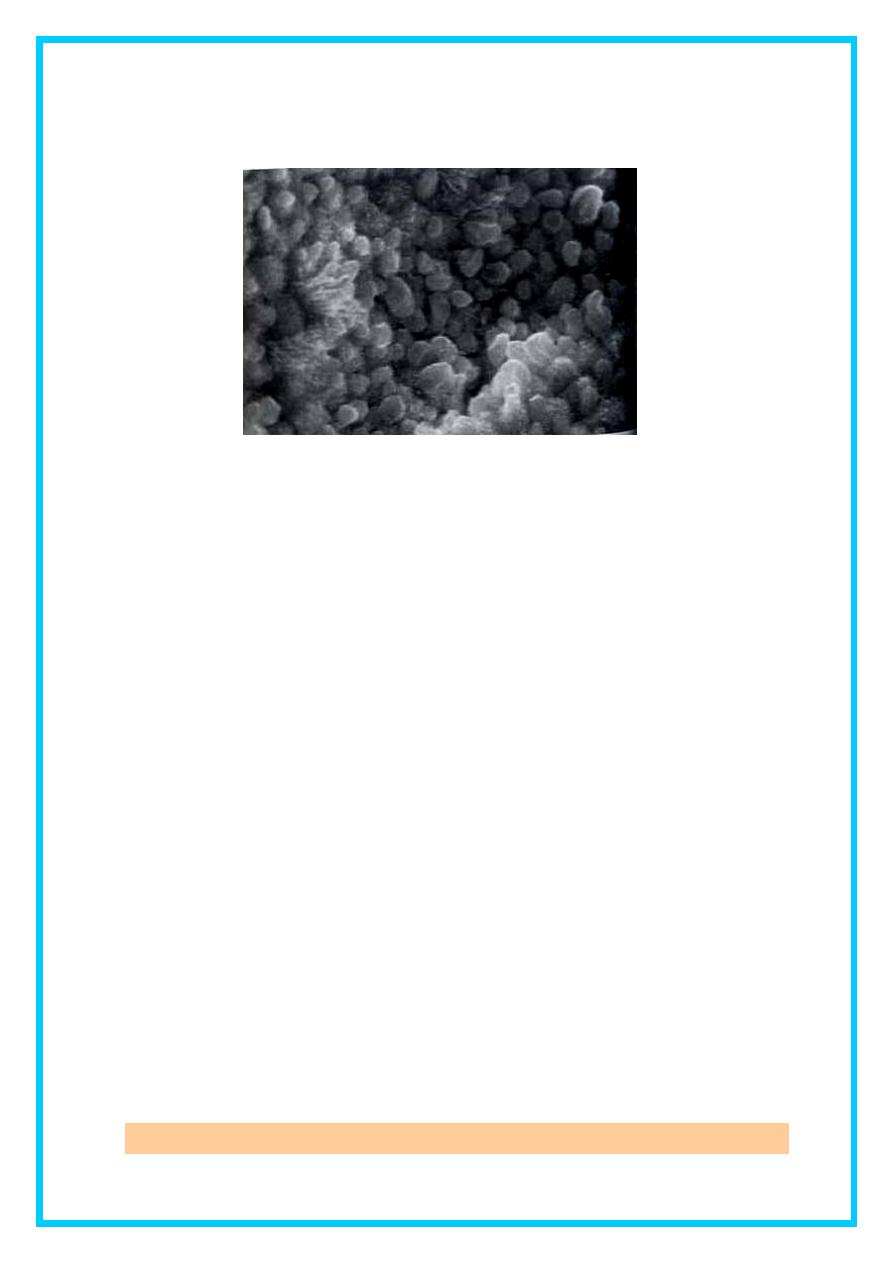
11
stage in making the endmetrium receptive for embryo implantation
( Figure 4 ) .
Figure (4) photomicrograph of endometrial pinopodes from the implantation
window .
Immediately prior to menstruation , three distinct layers of
endometrium can be seen .
1. The basalis is the lower 25 per cent of the endomtrium , which will
remain throughout menstruation and shows few changes during the
menstrual cycle .
2. The mid-portion is the stratum spongiosum with oedematous
stroma and exhausted glands .
3. The superficial portion ( upper 25 per cent ) is the stratum
compactum with prominent decidualized stromal cells . On the
withdrawal of both oestrogen and progesterone , the decidua will
collapse , with vasoconstriction and relaxation of spiral arteries
and shedding of the outer layers of the endometrium .
11
New developments :
Measurement of ovarian reserve :
Female reproductive potential is directly proportionate to the
remaining number of oocytes in the ovaries . This number decreases
from birth onwards .
It is desirable to be able to quantify the residual ovarian capacity of
women of older age or after undergoing treatment in order to give
prognostic information and management advice to patients , and also to
compare different forms of treatment . Research using :
1. Altrasound markers has looked at measurements of ovarian
volume , mean ovarian diameter and antral follicle count to
calculate ovarian reserve .
2. Biochemical markers include FSH . oestrodiol , inhibin B , anti-
Mullerian hormone ( AMH ) . AMH is produced in the granulosa
cells of ovarian follicles and does not change in response to
gonadotrophins during the menstrual cycle . As a result , it can be
measured and compared from any point in the cycle .
Harvesting ovarian tissue :
Harvesting and cryopreservation of ovarian tissue is an emerging
technique in reproductive biology . At present , its use is experimental and
offered to nulliparious women or young females undergoing gonadotrophic
therapy , for example to treat cancer . The theory is that strips of ovarian
cortex can be removed at laparoscopy or laparotomy and preserved by
freezing , in the hope that future technology will allow them to be thawed and
used to generate occytes for IVF treatment .
12
Objective
It is important to have an understanding of the physiology of the
normal menstrual cycle to understand the causes of any abnormalities ,
and also to tackle problems , such as infertility and the prevention of
unwanted pregnancy . This lecture aims to describe the mechanisms
involved in the normal menstrual cycle , with emphasis on the clinical
relevance of each phase .
