THE INFLAMMATORY RESPONSE
Inflammation is the response of tissues to injury or infection, and is necessary for normal
repair and healing..
PHYSIOLOGY AND PATHOLOGY
ACUTE INFLAMMATION
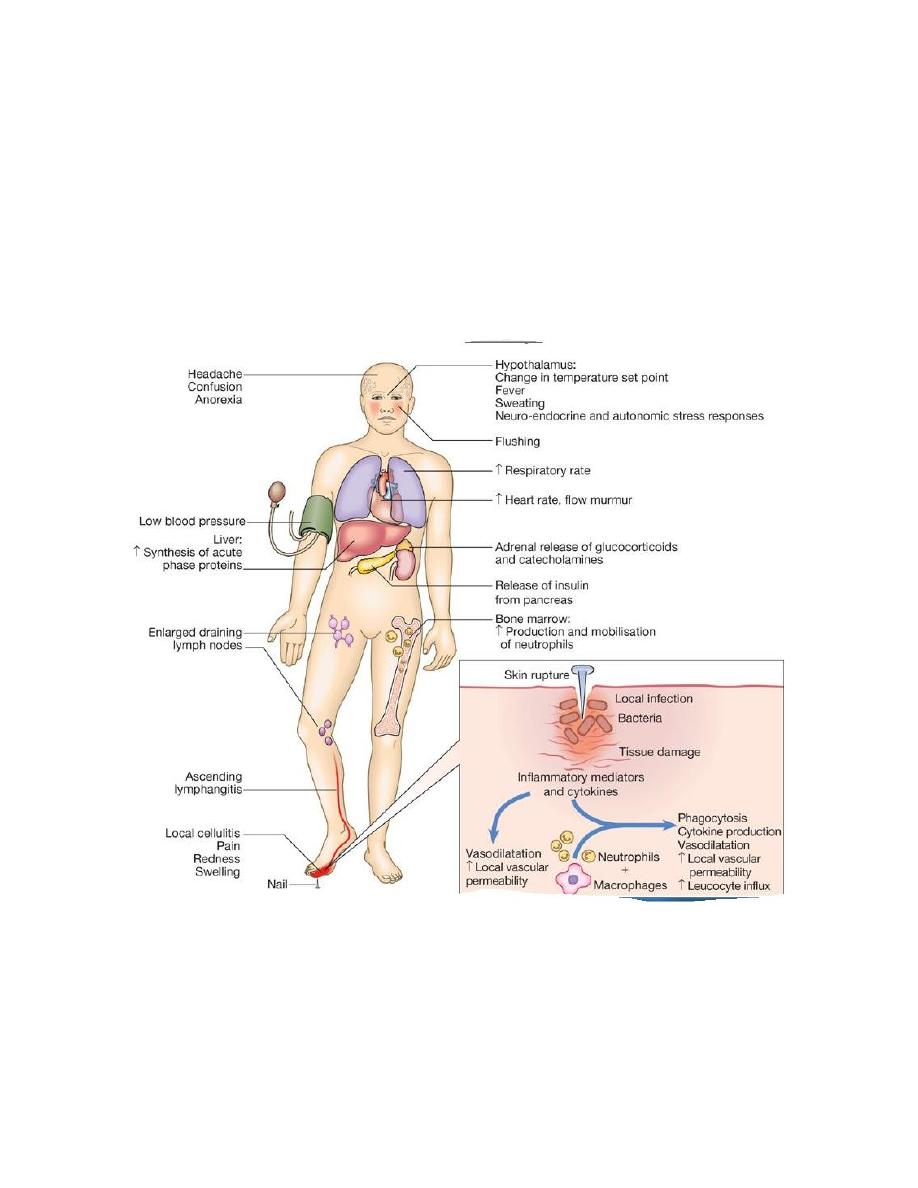
Acute inflammation is the result of rapid and complex interplay between the cells and soluble
molecules of the innate immune system. The classical external signs include heat, redness,
pain and swelling .
Figure Clinical features of acute inflammation. In this example, the response is to a
penetrating injury in the foot.
pro-inflammatory cytokines produced at the site of injury have
profound systemic effects
.(
IL-1, TNF-α and IL-6 ) act
1-on the hypothalamus to raise the temperature set-point,
2-and stimulate the production of acute phase proteins by the liver.

Acute phase proteins
1- C-reactive protein (CRP)
2- serum amyloid A.
3- Fibrinogen plays an essential role in wound healing,
4- α1-antitrypsin
5- α1-antichymotrypsin preventing widespread tissue destruction.
Erythrocyte sedimentation rate (ESR)
In contrast to the CRP, the ESR is an indirect measure of the acute phase response.
As CRP is a simpler and more sensitive early indicator of the acute phase response, it is
increasingly used in preference to the ESR
HIGH ESR IN
1-Acute bacterial, fungal or viral infection
Necrotising bacterial infection
Chronic bacterial or fungal infection, e.g. localised abscess, bacterial endocarditis or
tuberculosis
2- Acute inflammatory diseases, e.g. Crohn's disease, systemic vasculitides, polymyalgia
rheumatica, giant cell arteritis, SLE, Sjögren's syndrome
3- Myeloma
4- Pregnancy,
5-old age,
6- end-stage renal disease
7- Macrocytic anaemia
TRANSPLANTATION AND GRAFT REJECTION
Transplantation is definitive treatment of end-stage organ disease
The major complications
are
graft rejection, drug toxicity and infection consequent on immunosuppression.
Classification of transplant rejection
Type
Time
Pathological
findings
Mechanism
1-Hyperacute
rejection
Minutes to
hours
Thrombosis, necrosis Preformed antibody and complement activation
(type II hypersensitivity)
2-Acute vascular
rejection
5-30 days
Vasculitis
Antibody and complement activation
3-Acute cellular
rejection
5-30 days
Cellular infiltration CD4
+
and CD8
+
T cells (type IV hypersensitivity)
4-Chronic allograft
failure
> 30 days
Fibrosis, scarring
Immune and non-immune mechanisms

Solid organ transplantation inevitably stimulates an aggressive immune response by the
recipient, unless the transplant is between monozygotic twins.
The type and severity of the rejection response is determined by
1-
the genetic disparity between the donor and recipient,
2-
the immune status of the host and
3-
the nature of the tissue transplanted .
The most important genetic determinant is the difference between donor and recipient
HLA proteins
Acute cellular rejection is the most common form of graft rejection. It is mediated by
activated T lymphocytes and results in deterioration in graft function. If allowed to
progress, it may cause fever, pain and tenderness over the graft. It is usually amenable
to increased immunosuppressive therapy.
Hyperacute rejection
results in rapid and irreversible destruction of the graft. It
is
mediated by pre-existing recipient antibodies against donor HLA antigens
, which
arise as a result of previous exposure through transplantation, blood transfusion or
pregnancy. It is very rarely seen in clinical practice as the use of screening for anti-
HLA antibodies and pre-transplant cross-matching ensures the prior identification of
recipients with antibodies against a potential donor.
Investigations
Pre-transplantation testing
recipients are screened for
1- the presence of anti-HLA antibodies
If antibodies are detected, the recipient is excluded from receiving a transplant which carries
these alleles.
2-Donor-recipient cross-matching
. A positive cross-match is a contraindication to transplantation because of the risk of
hyperacute rejection.
Immunosuppressive drugs used in transplantation
Drug
Mechanism of action
Anti-proliferative agents e.g.
azathioprine,
mycophenolatemofetil
Inhibit lymphocyte proliferation by blocking DNA
synthesis.
Calcineurin inhibitors e.g.
ciclosporin, tacrolimus
prevent lymphocyte activation and block cytokine
transcription.
Corticosteroids
Decrease phagocytosis and release of proteolytic
enzymes; decrease lymphocyte activation and
proliferation; decrease cytokine production; decrease
antibody production

Complications of transplant immunosuppression
1-infection
CMV ,Pneumocystis.
2-malignancy
The increased risk of malignancy arises because T-cell suppression results in failure to
control viral infections.
A-Virus-associated tumours
include
lymphoma
(associated with EBV),
Kaposi's sarcoma
(associated with human herpesvirus 8) and
skin tumours
(associated with human
papillomavirus).
B- Immunosuppression is also associated with a small increase in the incidence of common
cancers not associated with viral infection
(such as lung, breast and colon cancer),
reflecting the importance of T cells in anti-cancer surveillance.
